[4].
However, there are no prospective studies done exclusively in neonates.
We set out to find out the correlation between OI and
OSI as well as determine the values of OSI corresponding to mild,
moderate and severe lung disease.
This was a prospective study conducted on
mechanically ventilated neonates who had blood sampling done for
arterial blood gas measurement for their clinical indications. Neonates
with congenial heart disease and who had SpO2 above 98% were excluded.
Arterial blood gas was done using Gem 6000 machine 30 seconds after
recording a stable SpO2 from post-ductal site with Philips intellivue
monitor.
Formulae used for calculation of OSI:
OSI = (MAP) X (FiO2)) / (SpO2). FiO2 and SpO2 are
expressed as decimals
OI = (MAP) X (FiO2%) / (PaO2)
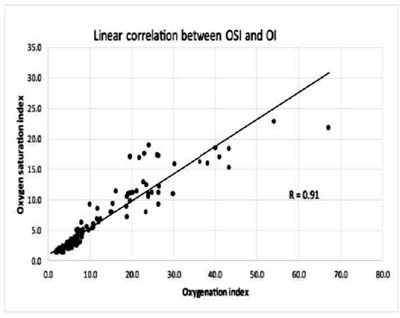
Pearson product moment correlation and Correlation
coefficient with linear mixed effect model between OI and OSI and OSI
corresponding to OIvalues for mild, moderate and severe disease (OI of
<5, 5-15 and >15) was calculated. Fifty-four neonates, both term and
preterm, were recruited. Thirty six neonates were on conventional, and
18 were on high frequency ventilation. A total of 141 datasets were
obtained. Minimum SpO2 recorded was 70% in one patient. Pearson product
moment correlation (r) for OSI and OI was 0.91 (Fig. 1).
Sub group analysis yielded R = 0.96 for babies on high frequency and R =
0.95 for babies on conventional ventilation (P<0.001). Linear
Mixed effect model yielded the y intercept of 1.6 and constant (B) of
0.4 for OSI; OSI = 1.6 + 0.4 OI (P = 0.001).
 |
|
Fig. 1 Correlation between Oxygen saturation index and
Oxygenation Index.
|
OI of 15 represented a PF ratio of 100 with
sensitivity of 97% and specificity of 100%. OI of 5 represented a PF
ratio of 200 with sensitivity of 94.7% and specificity of 93.5%. Hence
OI of 5 and 15 represented moderate and severe disease, respectively.
OSI of 3 and 6.5 corresponded to OI of 5 and 15, respectively with high
sensitivity and specificity (Table I).
TABLE I Oxygen Saturation Index cuJt-offs for different Oxygenation Index
|
Oxygenation Index |
<5
|
5 - 15 |
>15
|
|
(Mild) |
(Moderate) |
(severe) |
|
Oxygen Saturation Index |
2.9 |
3.0 |
6.5 |
|
Sensitivity |
89 |
89.4 |
100 |
|
Specificity |
93 |
93.6 |
93.7 |
OI has traditionally been the assessment tool for
acute lung disease in newborn [5-7] and need for arterial sampling is
its major limitation. OSI can overcome this limitation. In our study OSI
has shown high correlation of 0.91 with OI. Such non-invasive
assessments have the potential to reduce invasive procedures, workload
and cost.
Several other retrospective studies have noted high
correlation between OSI and OI [8-10]. We conclude that OSI has high
correlation with OI in neonates with hypoxemic respiratory failure, and
it has the potential to be used, both in clinical management and
research, to quantify the severity of lung disease.
References
1. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson
ND, Caldwell E, Fan E, et al. Acute respiratory distress
syndrome: the Berlin Definition. JAMA. 2012;307:2526-33.
2. Hallman M, Allen Merritt T, Jarvenpaa AL, Boynton
B, Mannino F, Gluck L, et.al. Exogenous human surfactant for
treatment severe respiratory distress syndrome: A randomized prospective
clinical trial. J Pediatr. 1985;106:963.
3. Brower RG, Matthay MA, Morris A, Schoenfeld D,
Thompson TB; writing committee for The Acute Respiratory Distress
Syndrome Network. Ventilation with lower tidal volumes as compared with
traditional tidal volumes for acute lung injury and the acute
respiratory distress syndrome. N Engl J Med. 2000;342:1301-308.
4. Thomas NJ, Shaffer ML, Willson DF, Shih MC, Curley
MAQ. Defining acute lung disease in children with the oxygenation
saturation index. Pediatr Crit Care Med. 2010;11:12-17.
5. Konduri G, Solimano A, Sokot GM, Singer J, Richard
A. Ehrenkranz, et.al. A randomized trial of early versus standard
inhaled nitric oxide therapy in term and near-term newborn infants with
hypoxic respiratory failure. Pediatrics. 2004;113:559-64.
6. Clark RH, Kueser TJ, Walker MW, Southgate WM,
Huckaby JL, Perez JA, et al. Low dose Nitric oxide therapy for
persistent pulmonary hypertension for newborn. N Engl J Med.
2000;342:469-74.
7. Ballard RA, Truog WE, Cnaan A, Martin RJ, Ballard
PL, Merrill JD, et al. Inhaled nitric oxide in preterm infants
undergoing mechanical ventilation. N Engl J Med. 2006;355:343-53.
8. Khemani RG, Thomas NJ, Venkatachalam V, Scimeme
JP, Ty Berutti, Schneider JB, et.al. Comparison of SpO2 to PaO2
based markers of lung disease severity for children with acute lung
injury. Crit Care Med. 2012; 40:1309-16.
9. Lobete C, Medina A, Rey C, Colunga JM, Concha A,
Menéndez S. Correlation of oxygen saturation as measured by pulse
oximetry/fraction of inspired oxygen ratio with PaO2/fraction of
inspired oxygen ratio in a heterogeneous sample of critically ill
children. J CritCare. 2013;28:538e1–538e7.
10. Khemani RG, Patel NR, Bart RD, Newth CJL.
Comparison of the Pulse Oximetric Saturation/Fraction of Inspired Oxygen
Ratio and the PaO2/Fraction of Inspired Oxygen Ratio in Children. Chest.
2009;135:662-8.

