edical schools came into being with the purpose
of generating a scientifically trained professional workforce for
serving the health needs of the society. Over the years, a perceptibly
increasing gap between the health professionals’ education, health care
delivered, and societal health needs has raised global concerns [1,2].
Medical schools are increasingly facing the question, ‘Are they
producing graduates who are competent to cater to health needs of the
society?’ – Perhaps, not in entirety. For any corrective action;
therefore, it is only befitting that we re-trace and work our way
backwards from first defining the expected roles of a physician that
best serve the healthcare requirements of the community (local and
global) and also to clearly state the characteristics and abilities of
doctors graduating from medical schools that enable them to perform
these roles well [3]. The curricula then need to be designed towards
achieving these outcome requirements steered by appropriate assessment
methods. Herein lies the origin and essence of Competency-based Medical
Education (CBME).
The goal of Undergraduate (UG) medical training is to
produce ‘doctors of first contact’ or ‘primary care physicians’. Having
stated this goal, most traditional curricula and training programs,
including those in Indian institutions, have been designed around the
educational/ learning objectives [2]. These objectives largely allude to
knowledge base with some reference to procedural skills, and behavior to
be developed during the course of training. The holistic description of
the outcome product of a medical school viz, the array of
abilities of a fresh graduate, so as to perform the expected roles in
providing health care to the community` has been lacking. Accordingly,
assessment methods also were traditionally designed to measure
attainment of knowledge or specific skills rather than the ability of
the graduate in delivering judicious and contextual health care in
authentic settings.
Awakened to this misalignment of training and needs,
the efforts at making the ‘competencies’ as the chief driving force of
medical training and curricular planning has gained momentum since the
turn of the century [1,2,4]. In this article we discuss the concept of
competency-based medical education in comparison to the traditional
curricula in the Indian perspective, and also its implementation,
particularly the assessment for such a medical training.
Definitions
The dictionary meaning of the terms ‘competency’ or
‘competence’ is "ability to do something" or "ability for a task". While
the two terms are used interchangeably, competencies may also be viewed
as ingredients of competence i.e., many specific competencies in
combination constitute a broader area of competence [5]. Competence in a
particular area encompasses many aspects and hence is best expressed as
a description (statement) of abilities in context of setting, experience
and time (or stage of training) [5-7].
A comprehensive and widely cited definition of
Professional competence as proposed by Epstein and Hundert in 2002,
states: "the habitual and judicious use of communication, knowledge,
technical skills, clinical reasoning, emotions, values, and reflection
in daily practice for the benefit of the individual and community being
served" [4].
With evolving understanding and increasing consensus
on the issue, a definition of Competency-based Education as proposed by
Frank, et. al. in 2010, makes the core purpose and curricular
elements of CBME more lucid: "Competency-based education (CBE) is an
approach to preparing physicians for practice that is fundamentally
oriented to graduate outcome abilities and organized around competencies
derived from an analysis of societal and patient needs. It de-emphasizes
time-based training and promises greater accountability, flexibility,
and learner-centeredness" [8]. Some experts consider CBME as another
form of outcome-based education (OBE), where learning outcomes assume
more importance than learning pathways or processes.
Global Movement Towards Competency-based Medical
Education
Competencies are context-dependent and hence are
contextually expressed and communicated. This has resulted in various
competency frameworks in use in different countries/regions. Also,
within the same country, these frameworks have undergone modifications
and refinements over time.
In United States, the Outcome Project was initiated
by the Accreditation Council for Graduate Medical Education (ACGME) in
2001 for emphasizing the ‘educational outcomes’ in terms of competencies
to be achieved during the course of training [9,10]. These competencies
were identified under six domains, also referred to as general
competencies, for all physicians irrespective of specialty. These are:
Medical Knowledge, Patient care, Interpersonal and Communication skills,
Professionalism, Practice-based learning and improvement, and
System-based practice. They provided a framework for education and
evaluation by specifying the end product rather than the desired
training process or pathway. As a refinement measure towards assessment
and defining the training pathway the ACGME launched the ‘Milestones
Project’ in 2007 [7,11]. Thus sub-competencies, that serve as
‘milestones’ along the way to becoming fully competent, and hence must
be achieved during the course of training were specified for each
outcome competency [9].
In United Kingdom, the General Medical Council
defined the outcomes and standards of graduate medical education, and
brought out the details of competency framework in form of the document
‘Tomorrow’s Doctors’ in 1993, that underwent further refinements over
time [12]. Three broad outcomes were specified for medical graduates: (i)
Doctor as a scholar and a scientist, (ii) Doctor as a
practitioner, and (iii) Doctor as a researcher. Under each of
these heads, sub competencies were further specified. The standards of
teaching learning and assessment were further grouped under nine
domains. For each domain, the standards, the criteria and the evidence
(for evaluation) were specified in concrete terms [12].
The Royal College of Physicians and Surgeons of
Canada (RCPSC) expressed the outcome of undergraduate medical training
in terms of seven ‘roles’ of a physician and developed competency
framework based on these – the Canadian Medical Education Directions for
Specialists (CanMEDS) [13]. These roles were: medical expert,
communicator, collaborator, manager, health advocate, scholar and
professional.
The National Undergraduate Framework in Netherlands
is yet another example of a well implemented outcome competency-based
medical education framework [3]. Medical educationists from the
Netherlands further propose that competencies are perhaps better
observed and measured as Entrustable Professional activities (EPA),
discussed later in the article [14]. An effort at defining outcomes has
also been noted from Vietnam, Mexico and China [15].
Comparison With Traditional Curriculum
A comparative analysis of traditional
discipline-based curriculum and competency-based curriculum is provided
in Web Table I [2,3,5,14,16-18]. However, this analysis
should not lead us to believe that one approach should completely
replace the other. Incorporating elements of competency-based training
utilizing the systems approach, and retaining the strengths of the
traditional curricula would be desirable. This would certainly be a
challenging task.
The three key steps in planning a competency-based
curriculum, as suggested by experts and utilized by institutions running
such programs [5,19-22] are:
1. Identification of competencies
2. Content identification and program
organization
3. Assessment planning and program evaluation
For implementation, they can be further divided into
component steps and strategies as shown in Table I.
Additionally, faculty development and creating conducive environment is
a must for effective delivery of the curriculum.
TABLE I Steps of Competency-based Curriculum Planning and Strategies for Implementation
|
Steps for planning Competency-based Curriculum |
Steps and strategies for implementation |
|
I |
Identification of competencies |
• |
Competency identification by consensus opinion of experts,
health needs, analysis of physician activities, self-report by
physicians to identify critical elements of behavior, critical
incidents, public health statistics, medical records, practice
setting and resources. |
|
|
• |
Exactly define required competencies and their components: Bring
out statement of learning outcomes and communicate to faculty
and students |
|
II |
Content identification & Program organization |
• |
Identify corresponding course content |
|
|
• |
Course organization: sequencing, learning opportunities, select
educational activities, experiences and instructional methods |
|
|
• |
Time organization: delineate minimum and maximum time period of
training; Create space for feedback sessions and opportunity to
reflect. |
|
|
• |
Define the desired level of mastery/expertise in each area |
|
|
• |
Define milestones or achievement points along development path
for competency i.e. charting of student progression pathway. |
|
III |
Assessment planning and Program evaluation |
• |
Identify observable and measurable form of competencies in real
settings; e.g. EPA |
|
|
• |
Define performance criteria: Establish minimum acceptable norms
of summative performance and intervening levels of expertise. |
|
|
• |
Select assessment tools to measure progress along the charted
pathways i.e. formative assessment for achievement of milestones |
|
|
• |
Develop a longitudinal assessment program (rather than
standalone formative and summative assessments), with emphasis
on WPBA methods: Make a blueprint with areas to be assessed,
timing and assessors |
|
|
• |
Design an outcomes evaluation program with scope for curricular
review and improvement |
|
|
• |
Faculty development and student orientation |
|
|
• |
Ensuring conducive educational environment |
|
|
• |
Student selection: incorporate some mechanism for assessing
aptitude and motivation towards pursuing medical studies and
delivering health care |
For program organization and assessment planning, it
is important to remember that the competencies are developmental, i.e.,
expertise in a said area progressively changes over time and with
experience. This has two implications: first, attainment of a competency
can be viewed as passing through intermediate levels of expertise in
various aspects of that competency, to be achieved (corresponding to the
stage of learning) during the course of becoming fully competent – akin
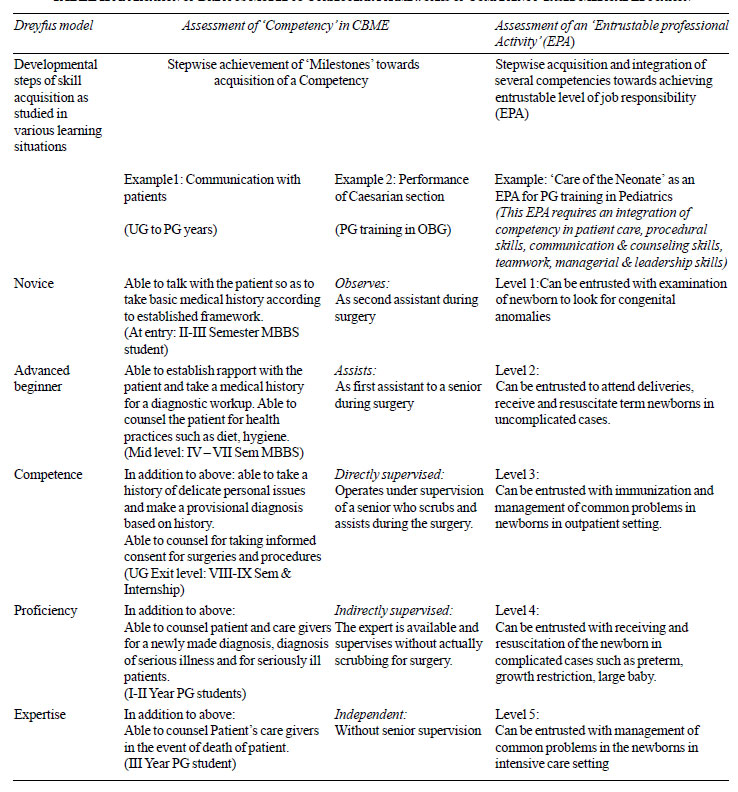
to the rungs of a ladder. Dreyfus and Dreyfus proposed a model of
phase-wise learning with developmental stages of skill acquisition, the
stages being Novice, Advanced beginner, Competence, Proficiency and
Expertise [23,24]. This model can also be applied to medical education
as illustrated in Table II. These meaningful achievement
points that mark the attainment of a predefined performance level during
the learning phase have been given different labels, e.g., the
Accreditation Council for Graduate Medical Education (ACGME), USA,
refers to these as ‘Milestones’ to be achieved on way towards becoming
fully competent [7,25].
|
TABLE II Application of Dreyfus Model to
Curricular Frameworks of Competency-based Medical Education
|
 |
The second consequence is, that a level of expertise
for being called ‘fully competent’ needs to be specified. This cut-off
is not set at the minimum level of expertise but at a level when the
person can act independently and take responsibility for his action or
performance in that area. Therefore, it is rightly said that the
ultimate goal in CBME is not merely attainment of competency but an
expertise (specified) in the area [16]. These two aspects are an
important consideration in designing the formative and summative
assessment in competency-based education.
Assessment in CBME
Some pertinent issues with regards to assessment in
CBME are discussed below:
What to assess?
In CBME, the outcome is expressed in terms of
competencies. Medical education literature distinguishes between the
terms ‘competence’ (meaning ‘able to do’) and ‘performance’ (meaning
‘actually does’). According to Miller’s pyramid model of clinical
competence, the assessment of performance is at the highest level
i.e. the ‘Does’ ; and competence assessment is a level below i.e
‘Shows how’. Naturally, performance assessment provides a more authentic
picture of trainees’ functionality in real clinical settings [17]. While
competence can be assessed in examination setting using simulations and
with tools such as Objective Structured Clinical Examination (OSCE), it
can perhaps be better inferred from observable workplace performance
using Workplace-based Assessment (WPBA) tools [18] .
What to Measure While Assessing?
Assessment requires identification of measurable and
observable entities. This could be in the form of whole tasks that
contribute to one or more competencies or assessment of a competency
per se. While it appears reasonably justifiable to work on this
framework, there have been concerns that attaining individual
competencies may not actually lead to actual or acceptable performance.
A trainee who is competent in history taking, physical examination and
treatment planning, may still be unable to actually treat a patient. In
this context, the concept of ‘Entrustable Professional Activity’ (EPA)
[6] makes a lot of sense.
The EPA encompasses a set of professional work
activities that together constitute the particular profession or
specialization. Only after mastering a certain set of competencies can a
trainee be entrusted with carrying out a particular professional
activity with responsibility [14,26]. Observing and measuring
competencies in form of EPA gives a more authentic information about the
ability of the trainee to function as a professional in real life
situation, and hence a better validity to assessment.
Let us try to illustrate this concept by using a
simple example. While teaching driving to a novice, we set certain
objectives for ourselves. For example, he ‘should be able to start the
engine’, ‘change the gears’, and ‘coordinate the release of clutch and
accelerator’ and so on. Attainment of these does not mean that he will
be able to drive a car. However, if we change our outcome to ‘competent
to drive a car’ then this problem can be avoided and we will continue
our training till the trainee is able to drive a car. When the trainee
demonstrates his ability to drive a car, we can call him competent.
However, there may be more issues to it. He may be able to drive a small
car but not a large one or he may be able to drive a car in a small town
but not in the traffic of a metropolis or not in a hilly terrain. We may
entrust a trainee driver to drive us in a small town with not much of
traffic but need to provide more training before we can entrust him to
drive us in a metro. On the same analogy, we have different levels of
trust on the trainees depending upon their degree of expertise, stage of
training and context of performance. The concept of EPA will be further
discussed in detail in our next article in this series.
In our day-to-day practice, we all entrust night on-
call residents with different levels of tasks – we depend on someone to
be able to decide on what samples to collect but may not depend on
him/her to make the choice of an antibiotic. EPAs help us to decide the
level of trust we can place on a trainee to independently handle a given
task.
It is also easier to observe and judge the
proficiency with which a certain job activity is performed rather than
trying to observe and measure each competency contributing to it. The
term ‘entrustable’ in EPA inherently conveys the minimum acceptable
standard i.e., the trainee is able to carry out the said clinical
activity independently, can take responsibility for the same and hence
can be entrusted with it. Ten Cate proposed that once the EPA is of an
acceptable standard, a written statement to this effect may be issued to
the trainee: a Statement of awarded responsibility (STAR) [14].
Assessment of EPA may have a relatively more meaningful and utilitarian
interpretation, especially in formative assessments.
Also, it is of extreme importance to define standards
of measurement of sub-competencies (e.g., Milestones or
benchmarks; Levels of EPA) to be achieved at various stages of training.
This charts out the desired pathway to becoming fully competent.
Examples of developmental phases of attainment of competency and
entrustment of professional activity, based on Dreyfus model are shown
in Table II. Though the framework of EPA appears more
suitable for Postgraduate training, it may also by utilized for
Undergraduate medical training thus providing a developmental continuum
to specialist training [27] The next paper in this series of medical
education articles is dedicated to a full discussion on EPA.
How to Measure: the Methods, Tools and Reporting
Since CBME focuses on the outcome, it is important to
observe and assess (and learn) at workplace. Daily practice area
provides a richer source of information rather than isolated hand-picked
tasks in examination setting. The WPBA methods assess at the ‘does’
level of Miller’s pyramid and hence are most suitable [18]. These
include mini-Clinical Evaluation Exercise (mini-CEX), Directly Observed
Procedural Skills (DOPS), mini-Peer Assessment Tool (mini-PAT),
Multisource feedback (MSF) as some of the common ones. Each of the tools
can provide information about more than one competency; and any
competency can be assessed in a better way by using more than one tool
(triangulation). We have already discussed WPBA in detail in an earlier
paper [27].
Another aspect is the recording and reporting of
observations. There has been an undue emphasis on objectification of
assessment scores [16]. Subjective interpretations of assessment have
been underutilized and in fact been maligned to some extent. To some
extent, it has been so because subjectivity has been misinterpreted as
bias. This concern can be minimized by utilising multiple assessors over
multiple occasions and settings. Judgment by an expert can be well
expressed subjectively in words. It may in fact be more meaningful and
useful to the trainee than a set of scores or categories conveyed at the
end of assessment. This is particularly true for CBME since competencies
are developmental and their progression depends heavily on the
appropriate steering by assessment. The formative function of assessment
is served well by subjective reporting of assessment.
Recently, there is increasing emphasis on utilising
qualitative approach in assessment [16]. Use of student narratives and
portfolios can be a rich source of information about student learning.
Tekian, et al. [28] propose redefining of ‘competence’ itself in
terms of construct narratives rather than as a checklist of component
tasks.
Feedback: Whatever the assessment method, tool or
reporting format, it is of utmost importance to provide an early and
effective feedback to the trainee, preferably based on direct
observation. Development of competencies hinges on the feedback received
by the student trainee so that student progresses through the charted
milestones. There is evidence in literature that establishes feedback as
the most important determinant of learner progression [16].
When to Assess?
Frequent (or continuous) formative assessments that
allow for and promote developmental progression are desirable in CBME.
This helps to keep the trainee on the correct trajectory towards end
outcomes [18]. Hence there is a greater emphasis on formative assessment
in CBME.
Who Should Assess?
Faculty, peers, colleagues may assess depending on
the competency being assessed. It is more important that the assessors
are trained in using the method and tools that they use. Inter-rater
variation in assessment can be reduced by assessor training as well as
defining the standards for expected outcomes.
Standards of Assessment in CBME
It is well expressed by educationists that expertise
and not competence is the ultimate goal in CBME [16]. The standards of
acceptable level of expertise must be well- defined in competency-based
training programs, and these must be defined not just for the outcome-
competencies but also for the intervening milestones to be achieved by
the trainee. While establishing cut off standards, it is important to
adopt a criterion-based approach [16,17]. That is, the set standard is
an absolute level of performance (or competence) and is not dependent on
the performance of other students. Adopting a normative-approach has the
inherent risk that the standards may be set below acceptable level of
expertise.
CBME: The Indian Scenario
In India, there has been a relatively recent
need-driven movement towards competency based medical education, and it
is yet in a fledgling stage of discussions and planning. The Graduate
Medical Education Regulations 1997 (GMER) of the Medical Council of
India (MCI) mention the term ‘competent’ under institutional goals but
do not define it further [29]. Following a series of meetings and
deliberations, reforms were suggested in the form of ‘Vision 2015’
document in 2011 [30]. For the first time, the outcomes of graduate
medical education were expressed as the competencies that an ‘Indian
Medical Graduate’ would develop so as to function as a ‘Basic Doctor’ or
physician of first contact to the people of India and the world. The
five roles of a Basic doctor were stated as: Clinician, Leader and team
member, Communicator, Lifelong learner, and Professional (who is
ethical, responsive and accountable to patients, community and
profession). The competencies to be developed to perform the above roles
were also specified. The term competency was meant to imply ‘desired and
observable ability in the real life situation’. Unfortunately, in these
deliberations, assessment was neither discussed in appropriate details
nor was an assessment program aligned to outcome- measurement included.
The document did mention in passing that assessment be ‘criterion
referenced’ without giving any further details.
Based on above deliberations and documents, the new
Graduate Medical Education Regulations 2012 (GMER 2012) were proposed
[31]. A salient feature of this revision of medical curriculum was
emphasis on competency-based curriculum. While subject-wise specific
outcome competencies were mentioned in this document, the alignment of
assessment towards measuring competencies again remained largely
unaddressed. The Postgraduate Medical Education Regulations 2000 (PGMER)
of the MCI merely mention that the PG curriculum be competency-based,
and that each department must produce statement of competencies [32].
Hence, we as a country still have a long road ahead
towards implementing competency-based medical training. There is a need
to review and revise our curriculum respecting the key role of
assessment in achieving the deliverables. With the benefit of the
existent curricular frameworks in use in different nations, we need to
develop a competency framework suited to our needs and feasible in our
settings and resources.
Faculty Development
Since the competency-based training program and
assessment methods differ in many ways from the traditional curricula,
it is important not only to orient the faculty to it but also to train
the faculty in using the appropriate assessment methods. Of particular
importance is the faculty training for improving the direct observation
skills and feedback skills.
Where We Stand and What Needs to be Done
As we move towards developing a competency-based
approach to medical education in our country, it is crucial to sensitize
and prepare the faculty for the change. An initial combined and
organized effort for identification of general competencies and
specialty competencies may be a good starting point. Assessment has a
key role in shaping the outcomes and success of a curriculum and hence
must be carefully planned.
1. Long DM. Competency-based residency training: The
next advance in Graduate Medical Education. Acad Med. 2000;75:1178-83.
2. Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N,
Evans T, et al. Health professionals for a new century:
transforming education to strengthen health systems in an interdependent
world. Rev Peru Med Exp Salud Publica. 2011;28:337-41.
3. Harris P, Snell L, Talbot M, Harden RM for the
International CBME Collaborators. Competency-based medical education:
implications for undergraduate programs. Med Teach. 2010;32:646-50.
4. Epstein RM, Hundert EM. Defining and assessing
professional competence. JAMA. 2002;287:226-35.
5. Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio
C, Swing SR, et al. Competency-based medical education: theory to
practice. Med Teach. 2010;32:638-45.
6. Englander R. Glossary of Competency-based
Education terms. Available from: http://dev.im.org/AcademicAffairs/milestones/Documents/CBME%20Glossary.pdf.
Accessed November 15, 2014.
7. Orgill BD, Simpson D. Towards a glossary of
competency-based medical education terms. J Grad Med Educ. 2014;6:203-6.
8. Frank JR, Mungroo R, Ahmad Y, Wang M, De Rossi S,
Horsley T. Toward a definition of competency-based education in
medicine: a systematic review of published definitions. Med Teach.
2010;32:631-7.
9. Accreditation Council for Graduate Medical
Education. ACGME Outcome Project enhancing residency education through
outcomes assessment: General Competencies. 1999. Available from:
http://www.acgme.org/outcome/comp/compFull.asp. Accessed November 9,
2014.
10. Joyce B. Introduction to Competency-based
education. Facilitators guide ACGME. 2006. Available from:
http://www.paeaonline.org/index.php?ht=a/GetDocument Action/i/161740.
Accessed December 27, 2014.
11. Weinberger SE, Pereira AG, Lobst WF, Mechaber AJ,
Bronze MS, Alliance for Academic Internal Medicine Education Redesign
Task Force II. Competency-based education and training in Internal
Medicine. Ann Intern Med. 2010;153:751-6.
12. General Medical Council. Tomorrow’s Doctors:
Education Outcomes and standards for undergraduate medical education.
Available from:
http://www.gmcuk.org/Tomorrow_s_Doctors_0414.pdf_48905759.pdf.
Accessed December 27, 2014.
13. Frank JR, Danoff D. The CanMEDS Initiative:
implementing an outcomes-based framework of physician competencies. Med
Teach. 2007;29:642-7.
14. ten Cate O, Scheele F. Competency-based
Postgraduate training: Can we bridge the gap between theory and clinical
practice. Acad Med. 2007;82:542-7.
15. Harden RM. Outcome-based education – The future
is today. Med Teach. 2007;29:625-9.
16. Holmboe ES, Sherbino J, Long DM, Swing SR, Frank
JR, for the International CBME Collaborators. The role of assessment in
competency-based medical education. Med Teach. 2010;32:676-82.
17. van Mook WNKA, Bion J, van der Vleuten CPM,
Schuwirth LWT. Integrating education, training and assessment:
competency-based intensive care medicine training. Neth J Crit Care.
2011;15:192-8.
18. Boursikot K, Etheridge L, Zeryab S, Sturrock A,
Ker J, Smee S, Sambandam E. Performance in assessment: Consensus
statement and recommendations from the Ottawa conference. Med Teach.
2011;33:370-83.
19. Chacko TV. Moving towards competency-based
education: Challenges and the way forward. Arch Med Heath Sci.
2014;2:247-53.
20. McGaghie WC, Miller GE, Sajid AW, Telder TV.
Competency–based Curriculum Development in Medical Education. An
Introduction. Geneva: World Health Organization; 1978.
21. Harden RM. Outcome-based education – the ostrich,
the peacock and the beaver. Med Teach. 2007;29:666-71.
22. Smith SR, Dollase R. AMEE guide No. 14: Outcome-
based education Part 2 – Planning, implementing and evaluating a
competency–based curriculum. Med Teach. 1999;21:15-22.
23. Dreyfus HL, Dreyfus SE. Mind over Machine: The
Power of Human Intuition and Expertise in the Age of the Computer.
Oxford: Basil Blackwell; 1986.
24. Batalden P, Leach D, Swing S, Dreyfus H, Dreyfus
S. General competencies and accreditation in Graduate medical education.
Health Affairs. 2002;21:103-11.
25. Nasca TJ, Philibert I, Brigham T, Flynn TC. The
next GME accreditation system – rationale and benefits. New Eng J Med.
2012;366:1051-6.
26. van Loon KA, Driessen EW, Teunissen PW, Scheele
F. Experiences with EPAs, potential benefits and pitfalls. Med Teach.
2014;36:698-702.
27. Singh T, Modi JN. Workplace based assessment: A
step to promote competency based training. Indian Pediatr.
2013;50:553-9.
28. Tekian A, Hodges BD, Roberts TE, Schuwirth L,
Norcini J. Assessing competencies using milestones along the way. Med
Teach. 2014;19:1-4.
29. Medical Council of India Regulations on Graduate
Medical Education 1997. Available from:
http://www.mciindia.org/RulesandRegulations/GraduateMedicalEducation
Regulations1997.aspx. Accessed November 10, 2014.
30. Medical Council of India. Vision 2015. Medical
Council of India. New Delhi. 2011. Available from:
http://www.mciindia.org/tools/announcement/MCI_booklet.pdf.
Accessed November 10, 2014.
31. Medical Council of India Regulations on Graduate
Medical Education 2012. Available from:
http://www.mciindia.org/tools/announcement/Revised_GME_2012.pdf .
Accessed October 2, 2014.
32. Medical Council of India, Post Graduate Medical
Education Regulations 2000, Medical Council of India, New Delhi.
Available from:
http://www.mciindia.org/Rules-and-Regulation/Postgraduate-Medical-Education-Regulations-2000.pdf.
Accessed November 29, 2014.

