|
|
|
Indian Pediatr 2014;51:
359-365 |
 |
INCLEN Diagnostic Tool for Autism Spectrum
Disorder (INDT-ASD): Development and Validation
|
|
Monica Juneja, Devendra Mishra, Paul SS Russell,
Sheffali Gulati, Vaishali Deshmukh, Poma Tudu, Rajesh Sagar, Donald
Silberberg, Vinod K Bhutani, Jennifer M Pinto, Maureen Durkin, Ravindra
M Pandey, MKC Nair, Narendra K Arora and INCLEN Study Group *
From the INCLEN Trust International, New Delhi,
India.
Correspondence to: Dr Narendra K Arora, Executive
Director, The INCLEN TRUST International, F1/5, Okhla Industrial Area,
Phase-1, New Delhi, India.
Email: [email protected]
*INCLEN STUDY GROUP: Core Group: Alok
Thakkar, Arun Singh, Gautam Bir Singh, Manju Mehta, Manoja K Das,
Nandita Babu, Praveen Suman, Ramesh Konanki, Rohit Saxena, Satinder
Aneja, Savita Sapra, Sharmila Mukherjee, Sunanda K. Reddy, Tanuj Dada.
Extended Group: A.K Niswade, Archisman Mohapatra, Arti Maria,
Atul Prasad, B.C Das, Bhadresh Vyas, G.V.S Murthy, Gourie M. Devi,
Harikumaran Nair, J.C Gupta, K.K Handa, Leena Sumaraj, Madhuri Kulkarni,
Muneer Masoodi, Poonam Natrajan, Rashmi Kumar, Rashna Dass, Rema Devi,
Sandeep Bavdekar, Santosh Mohanty, Saradha Suresh, Shobha Sharma,
Sujatha S. Thyagu, Sunil Karande, T.D Sharma, Vinod Aggarwal, Zia
Chaudhuri.
Received: April 03, 2013;
Initial Review: May 21, 2013;
Accepted: February 15, 2014.
|
Objective: To develop and validate INCLEN Diagnostic Tool for Autism
Spectrum Disorder (INDT-ASD).
Design: Diagnostic test evaluation by cross
sectional design
Setting: Four tertiary pediatric neurology
centers in Delhi and Thiruvanthapuram, India.
Methods: Children aged 2-9 years were enrolled in
the study. INDT-ASD and Childhood Autism Rating Scale (CARS) were
administered in a randomly decided sequence by trained psychologist,
followed by an expert evaluation by DSM-IV TR diagnostic criteria (gold
standard).
Main outcome measures: Psychometric parameters of
diagnostic accuracy, validity (construct, criterion and convergent) and
internal consistency.
Results: 154 children (110 boys, mean age 64.2
mo) were enrolled. The overall diagnostic accuracy (AUC=0.97, 95% CI
0.93, 0.99; P<0.001) and validity (sensitivity 98%, specificity
95%, positive predictive value 91%, negative predictive value 99%) of
INDT-ASD for Autism spectrum disorder were high, taking expert diagnosis
using DSM-IV-TR as gold standard. The concordance rate between
the INDT-ASD and expert diagnosis for ‘ASD group’ was 82.52% [Cohen’s
k=0.89;
95% CI (0.82, 0.97); P=0.001]. The internal consistency of
INDT-ASD was 0.96. The convergent validity with CARS (r = 0.73, P=
0.001) and divergent validity with Binet-Kamat Test of intelligence (r =
-0.37; P=0.004) were significantly high. INDT-ASD has a 4-factor
structure explaining 85.3% of the variance.
Conclusion: INDT-ASD has high diagnostic
accuracy, adequate content validity, good internal consistency high
criterion validity and high to moderate convergent validity and 4-factor
construct validity for diagnosis of Autistm spectrum disorder.
Keywords: Childhood; Neuro developmental disorders; Resource
limited settings; Childhood austism rating scale; Pervasive
developmental disorders.
|
|
Autism Spectrum Disorder (ASD) is widely
recognized for many decades, yet there are no definitive or universally
accepted diagnostic criteria. [1]. Most diagnostic systems and measures
consider ASD to be a 3-symptom cluster disorder with varying severity
and etiology. This is reflected in the diagnostic systems of Diagnostic
and Statistical Manual of Mental Disorders- IV Text Revision (DSM-IV TR)
and International Classification of Diseases-10 (ICD-10), as well as the
various measures that evolved from them [2,3]. However, the field trials
of the draft version of Diagnostic and Statistical Manual of Mental
Disorders-5 (DSM-5) have supported a 2-symptom cluster model [4,5] of
varying severity.
The construct, core and behavioral symptoms as well
as the reliability of the diagnosis of ASD in diverse socio-cultural
settings using the available tools have been problematic. In addition to
the evolving construct of ASD globally, the timing of the presentation
of this group of disorders [6] and racial differences have been
documented to bring about variations in the core symptoms and associated
behavioral features [7]. In multi-centric studies, the diagnostic
distinctions among sub-categories of ASD has been unreliable across
centers even while using standard diagnostic instruments, supporting a
shift from a categorical to dimensional approach in the diagnosis of ASD
[8]. The use of detailed and explicit appropriateness criteria has
significantly enhanced the diagnostic yield in other medical disciplines
[9]. Furthermore, currently available diagnostic instruments for ASD are
patented [10,11], not available in different Indian languages, and fee
is to be paid each time the instrument is used. To overcome several of
these limitations, INCLEN Diagnostic Tool for Autism Spectrum Disorder
(INDT-ASD) was developed for identification and diagnosis of ASD using
appropriateness criteria developed for Indian context.
Methods
Development of Appropriateness Criteria and Instrument
A team of 49 national experts from different parts of
India and six international experts (pediatricians, child psychiatrists,
pediatric neurologists, epidemiologist, pediatric
otorhinolanringologists, clinical psychologists, special educators,
specialist nurses, speech therapist, occupational therapists and social
scientists) developed the appropriateness criteria and tool over three
rounds of 2-day workshop in 2006-2007. During this process, the clinical
criteria for ASD as presented in the ICD-10, DSM-IV TR Autism Diagnostic
Observation Schedule (ADOS), Childhood Autism Rating Scale (CARS),
Gilliam Autism Rating Scale (GARS), Modified Checklist for Autism in
Toddlers (M-CHAT) and clinicians’ views on the construct of ASD were
reviewed. Pools of items were selected by the panel using the modified
Delphi technique [12]. From the pool of items, the symptoms were
rank-ordered by the panel members, and further reduced using endorsement
rate approach [13].
The construct and its sub-construct were adapted for
its appropriateness in the Indian cultural context and converted into
symptoms clusters for the clinicians and psychologists to rate during
the diagnostic workup. The tool was named as INCLEN Diagnostic Tool for
ASD (INDT-ASD). The tool has two sections: Section A has 29
symptoms/items and Section B contains 12 questions corresponding to B
and C domains of DSM-IV-TR, time of onset, duration of symptoms, score
and diagnostic algorithm. It takes approximately 45-60 minutes to
administer the instrument and score. A trichotomous endorsement choice
(‘yes’, ‘no’, ‘unsure/not applicable’) is given to the assessor/
interviewer. In addition, the clinician/psychologist has to make
behavioral observations on the child and score the item as well. For any
discrepancy in parental response and interviewer’s assessment, it is
indicated for each question whether parental response or assessor’s
observation should take precedence. Each symptom/item is given a score
of ‘1’ for ‘Yes’ and ‘0’ for ‘No’ or ‘unsure/not applicable’. Presence
of ³ 6
symptoms/item (or score of ³
6), with at least two symptom/item each from impaired communication and
restricted repetitive pattern of behavior, is used to diagnose ASD [Web
Appendix I].
The instrument was first developed in English, and
forward and backward translated to Hindi and Malayalam by two teams with
two independent, bilingual translators in each, to achieve the proximity
of the source and target versions. This instrument was piloted (first
pilot psychometric evaluation round, described below). Based on the
feedback, the instrument was modified in Hindi version and then forward
translated to English, Malayalam and six additional Indian languages (Odia,
Konkani, Urdu, Khasi, Gujarati and Telugu) and backward translated
in a similar manner.
Psychometric evaluation
The first round of psychometric (pilot) testing for
INDT-ASD was done with 266 children at two sites (New Delhi-178 and
Thiruvananthapuram-88). These included 81 children of ASD, 120 with
other neuro-developmental disorders (NDDs) and 65 with typical
development. However, as the ability of INDT-ASD to differentiate autism
from other NDDs (specificity 69%) and the agreement with CARS [14] was
moderate (kappa=0.69), further training and modifications in translation
(12 items), item changes (3 items) and reframing (7 items with new
examples) was done.
In the second round, psychometric (field) testing of
the INDT-ASD was conducted in four public sector tertiary-care pediatric
referral centers: All India Institute of Medical Sciences (AIIMS),
Maulana Azad Medical College (MAMC), and Lady Hardinge Medical College
(LHMC), New Delhi; and Child Development Centre (CDC) in
Thiruvananthapuram.
Consecutive children (2-9 yr) with written informed
consent from their primary caregivers were enrolled into the study from
the Child development and Child neurology outpatient clinics. The
children were recruited until the a priori sample size was
reached. The validation exercise was conducted from June 2008 to April
2010.
 |
|
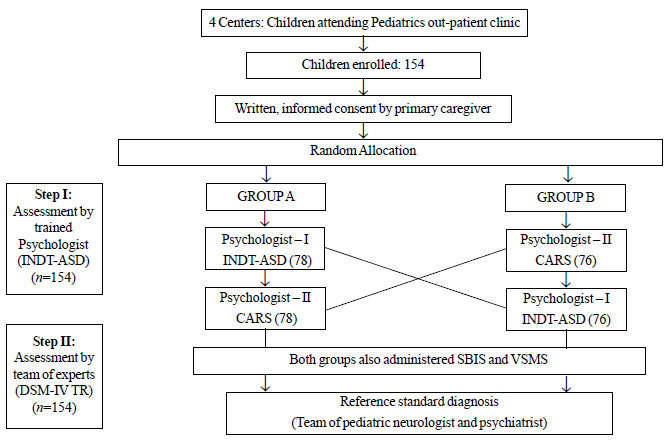
Fig. 1 Process of subject grouping,
randomization and assessment for psychometric validation of
INDT-ASD.
|
Fig. 1 depicts the method for patient
selection, assessment and interview. At every center, the study
coordinator, who was not part of any assessment, evaluated the children
attending the clinic for eligibility and enrolled them in the study. The
subjects were randomly allocated into Group A (N=78) and Group B
(N=76). In Group A, INDT-ASD was administered followed by CARS
and the sequence was reversed in Group B. This was done by independent
psychologists to minimize rating bias. Thereafter, each child was
assessed by a two-member expert team (pediatric neurologist and child
psychiatrist) who based their diagnosis on DSM-IV TR criteria. The
diagnostic protocol required approximately four hours over two days, and
consisted of (i) a face-to-face interview with parent/primary
caregiver, as well as (ii) direct observations of children in
play activities. Each evaluator was blinded to original diagnosis and
assessment results of other evaluator; their evaluations were separately
sealed in opaque envelops immediately after the assessment.
Sample size and sampling technique: Sample size
for diagnostic accuracy was calculated assuming the sensitivity and
specificity of INDT-ASD to diagnose ASD to be 85%, with a precision of
±10% at 95% confidence level. The sample size was calculated to be 50
children in each of the three categories: ASD, other NDD, and normal
development. This sample was also adequate for exploratory factor
analysis during validation [15]. CARS was used to study the convergent
validity of INDT-ASD as well as divide the participants in to mild and
severe autism groups [16]. The Stanford-Binet Intelligence Scale (SK
Kulshreshtha, Hindi version) (SBIS) [17] and Vineland Social
Maturity Scale (VSMS) [18] were used in all subjects to measure
divergent validity of INDT-ASD.
The CARS is a 15-item behavior-rating scale designed
to detect and quantify
symptoms of autism. Each item on the CARS is scored on a Likert
scale, from 1 (no symptoms of autism) to 4 (severe
symptoms). The maximum CARS
score is 60, and a score of 30.5 is suggestive of autism. Children with
scores of 30.5 to 37 are rated as mildly-moderately autistic,and 37.5 to 60 as severely autistic by CARS.
A comprehensive and structured three day training
workshop was conducted for psychologists using standardized manual
developed for INDT-ASD, CARS, SBIS, and VSMS. Separate training groups
(A and B; Fig. 1) of psychologists for INDT-ASD and CARS
were created. Both groups were trained to administer SBIS and VSMS. Two
pediatric neurologists and two child psychiatrists with over ten years
of professional experience were the trainers.
Data processing and statistical analysis:
Participants’ assessment details were entered into a pre-designed
instrument with unique identification numbers. Statistical analysis was
done using SPSS (version 19) and MedCalc (version 12.2.1.0) after data
was entered into Intelligent Character Recognition (ICR) sheets. These
were processed using ABBYY Form Reader 4.0 software. Psychometric
parameters of diagnostic accuracy, construct validity, criterion
validity and internal consistency of INDT-ASD were estimated. The
performance of INDT-ASD was compared with CARS for convergent validity.
IndiaCLEN Review Board and the local Institutional
Review Boards/Ethical Committees of all the participating centers
provided approval for the study. Written informed consent was obtained
from parent/primary caregiver and verbal assent from children, whenever
possible. At the end of the assessment, parents were informed regarding
the child’s needs and appropriate referrals were facilitated, when
warranted.
Results
The mean (SD) age of enrolled children was 64.2
(25.3) months (n=154; 110 boys). Ninety children had average and
64 had subnormal intelligence.
According to the expert diagnosis based on DSM-IV TR
(considered as the gold standard), 51 children were diagnosed as ASD:
autism (44), Pervasive developmental disorder not otherwise specified
(PDD-NOS) (5), Rett syndrome (1), and CDD (1). Severe ASD was
present in 41 and mild-to-moderate in 10 children. Forty-nine "Other
NDDs" included intellectual disability (29), neuro-motor impairments
including cerebral palsy (6), epilepsy (4),
attention-deficit/hyperactivity disorder (2), vision/hearing impairment
(2), and speech and language disorder (1); multiple NDDs were noted
among 5 children.
The INDT-ASD had high diagnostic accuracy against
expert evaluation using DSM-IV-TR for diagnosing ASD (Table I).
The area under-curve (AUC) for INDT-ASD against the expert diagnosis,
was 0.97 (95% CI 0.93, 0.99; P=0.0001). None of the
symptoms/items in the criteria were assigned a score of ‘0’ by more than
half of the children with autism in this study.
The high concordance rate of 82.5% and a significant kappa value
(Cohen’s k=0.89;
95%CI 0.82, 0.97; P=0.001) between the INDT-ASD and expert
diagnosis indicated a high criterion validity for INDT-ASD. The
INDT-ASD had a false positive rate of 5.8%. All the five false positive
cases had "other NDDs": cerebral palsy (N=3), intellectual disability
(N=1), and speech and language disorder (N=1). One child with ASD was
missed (false negative). No normal child was misclassified as having
autism.
TABLE I Diagnostic Accuracy of INDT-ASD Against Expert Diagnosis Using DSM-IV TR Criteria
|
Comparison Group |
Sensitivity
|
Specificity
|
Positive predictive |
Negative predictive |
Positive likelihood |
Negative likelihood
|
|
% (95% CI) |
% (95% CI) |
value % (95%CI) |
value % (95% CI) |
ratio % (95% CI) |
ratio % (95% CI) |
|
ASD vs. normal
|
98.0 (89.5-99.9) |
95.1 (89.0-97.9) |
90.9 (80.4-96.1) |
99.0 (94.5-99.8) |
20.1 (8.5-47.5) |
0.02 (0.003-0.1) |
|
Autism vs. normal
|
95.5 (84.9-98.7) |
90.9 (84.1-95.0) |
80.8 (68.1-89.2) |
98.0 (93.1-99.7) |
10.49 (5.7-19.0) |
0.05 (0.01-0.1) |
|
ASD vs. other NDD
|
98.0 (89.5-99.5) |
87.8 (75.8-94.3) |
89.3 (78.5-95.0) |
97.0 (88.2-99.6) |
8.00 (3.7-16.9) |
0.02 (0.003-0.1) |
|
Autism vs. other NDD
|
95.5 (84.9-98.7) |
82.1 (70.2-90.0) |
80.8 (68.1-89.2) |
95.8 (86.0-98.8) |
5.34 (3.0-9.4) |
0.05 (0.01-0.2) |
|
INDT-ASD total score
|
|
|
|
|
|
|
|
> 5 and possibility of ASD
|
98.1 (93.0-100) |
90.8 (83.3-95.7) |
85.7 (74.5-93.3) |
98.9 (94.0-100) |
10.6 (9.9-11.5) |
0.02 (0.03- 0.2) |
|
n=51 for ASD, 54 for normal, 44 for autism, 49 for other
NDD; INDT-ASD: INCLEN Diagnostic Tool for Autism Spectrum
Disorder; DSM-IV TR: Diagnostic and Statistical Manual of Mental
Disorders Text Revision; ASD: Autism Spectrum Disorder; NDD:
Neuro-developmental Disorder. |
The convergent validity between the INDT-ASD and CARS
was high (r = 0.73, P= 0.001). Divergent validity
calculated by correlating INDT-ASD scores to the SBIS showed a moderate
negative correlation (r = -0.37; P=0.004).
To investigate the construct validity, we explored
the factor structure of the items in the INDT-ASD. We extracted the
factors with an Eigen value of >1 and thus, a 4-factor structure was
derived. There was no INDT-ASD item that did not achieve the required
factor loading (0.4) on to at least one factor (Web Table I).
In INDT-ASD, 14 symptoms/items loaded onto the
socialization-communication factor, three symptoms/items loaded onto the
repetitiveness-socialization factor, two symptoms/items loaded on to the
restricted repertoire of interest factor, and finally all the 10 sensory
symptom factor also cross-loaded on to other factors. This four-factor
structure explained 85.3% of the variance.
The Cronbach’s a
coefficient for the whole construct of ASD was high (a
= 0.96) suggesting that the INDT-ASD in this
population has high internal consistency and Cronbach’s
a coefficients for
the sub-constructs ranged between 0.82 and 0.96.
The performance of INDT-ASD was equally good among
pre-school (<6 yrs) and primary-school children ( ³6
yrs), among both genders, children with normal and subnormal
intellectual ability, and in children with mild to moderate and severe
ASD (AUC between 0.78 and 0.99).
Discussion
Diagnosis of ASD involves eliciting extensive
history, and detailed observation by experienced clinicians and
psychologists. The sensitivity and specificity of ASD of INDT-ASD was
98% and 95.1%, respectively in our study. This is better than the
performance documented in the DSM-III field trial [19] and the ICD-10
field trial [20]. The DSM-IV TR [21] sensitivity of 93% is closer to our
findings, although the specificity was only 78%. The specificity of
INDT-ASD is similar to that of DSM-5 (95%) but the sensitivity is much
higher (76%) [22].
High Cronbach’s alpha coefficient for internal
consistency demonstrated that the symptom clusters of INDT-ASD as used
in the Indian context were homogeneous. Some previous studies for
homogeneity of the symptom groups support our findings [21], whereas
others differ with the present findings [23,24].
The agreement rate between INDT-ASD and DSM-IV-TR
(used by expert team) is better than that reported for the DSM-III,
DSM-III-R and ICD-10 [19]. Our false positive rate of 5.8% is comparable
with that of the values reported for DSM-III but lower than that of
DSM-III-R [19]. In our study, children with cerebral palsy and
intellectual disability had impairment in proto-declarative and
proto-imperative pointing and were poorly communicative. This possibly
resulted in false positivity of INDT-ASD. The false negative diagnosis
was also far lower than that reported for DSM-III and DSM-III-R [19].
The only false negative case in the current study had low-average
Intelligence quotient (IQ) with mild autism symptoms.
The convergence between the INDT-ASD and CARS was
high suggesting that the construct of autism as measured by INDT-ASD and
CARS are theoretically related to each other. The negative correlation
between INDT-ASD and IQ as measured by SBIS shows that INDT-ASD has the
ability to diverge from theoretical constructs that are different from
its own, like construct of autism from other childhood disabilities.
However, data for comparison of the concurrent validity for DSM and ICD
are not readily available in the literature.
The factor analysis of the symptom clusters of
autism, as a measure of external validity of the construct has yielded
diverse structure models across different studies [23-28]. For instance,
the study by Tadevosyan-Leyfer, et al. [26] demonstrated a
6-factor structure, while other studies have documented a classical
3-factor [26] like represented in DSM-IV-TR and ICD-10 or alternative
3-factor structure [29,30] and even a 1-factor structure explaining the
construct of autism. Our item loading, the 4-factor structure and 85.3%
of variance being explained, makes it closer to the existing model
offered by Tanguay, et al. [25].
The main methodological differences, such as population
characteristics, factor-extraction and factor-retention procedures,
language versions, and statistical approaches, are aspects that might
explain the variability of findings across these factor analyses of the
autism criteria.
As the study was conducted in tertiary-care
hospitals, the participants may not be representative of the children
with autism in the general population and those presenting in primary
and secondary care. Further community-based studies to establish the
sensitivity and specificity of
INDT-ASD are suggested. Another limitation is that the
tool was validated in children 2-9 years of age, and may not capture the
diagnosis in children less than two years of age. Moreover, a larger
sample size could have generated more stable factor structure models
thereby improving the confidence in the validity of identified
constructs, providing more accurate estimates of sensitivity,
specificity, and predictive values.
Establishing the appropriateness of the international
criteria in the Indian context enhances the possibility of accurate
clinical diagnosis and paves way to developing as well as validating new
measures for autism in India. With similar approach and appropriate
modification, tools may be developed for use in other resource limited
settings.
Contributors: All authors have contributed,
designed and approved the study. NKA will act as a guarantor for this
work.
Funding: Ministry of Social Justice
and Empowerment (National Trust), National Institute of Health
(NIH-USA); Fogarty International Center (FIH), and Autism Speaks (USA).
Competing interests: None stated.
|
What is Already Known?
• Autism spectrum disorder (ASD) is a
clinical diagnosis by experienced and trained developmental
pediatricians, child psychiatrists and psychologists. Currently
available diagnostic tools are developed for Western populations
and are subject to payment of fee.
What This Study Adds?
• The INDT-ASD is a simple, validated
diagnostic algorithm for Autism Spectrum Disorders in children,
designed on DSM-IV TR criteria through expert consensus.
|
References
1. Volkmar F, State M, Klin A. Autism and autism
spectrum disorders: diagnostic issues for the coming decade. J Psychol
Psychiatry. 2009; 50:108-15.
2. The International Classification of Disease
(ICD-10): Classification of Mental and Behavioral Disorders. Clinical
Descriptions and Diagnostic Guidelines: World Health Organization,
Geneva; 2002.
3. American Psychiatric Association (APA). Diagnostic
and Statistical Manual of Mental Disorders (4th ed, text rev.)
(DSM-IV-TR): Washington, DC; 2000.
4. Mandy WP, Charman T, Skuse DH. Testing the
construct validity of proposed criteria for DSM-5 autism spectrum
disorder. J Am Acad Child Adolesc Psychiatry. 2012; 51:41-50.
5. Frazier TW, Youngstrom EA, Speer L, Embacher
R, Law P, Constantino J, et al. Validation of proposed DSM-5
criteria for autism spectrum disorder. J Am Acad Child Adolesc
Psychiatry. 2012; 51:28-40.
6. Bakare MO, Munir KM. Excess of non-verbal cases of
autism spectrum disorders presenting to orthodox clinical practice in
Africa - a trend possibly resulting from late diagnosis and
intervention. S Afr J Psychiatr. 2011; 17:118-20.
7. Sell NK, Giarelli E, Blum N, Hanlon AL, Levy SE. A
comparison of autism spectrum disorder DSM-IV criteria and associated
features among African American and white children in Philadelphia
County. Disabil Health J. 2012; 5:9-17.
8. Lord C, Petkova E, Hus V, Gan W, Lu F, Martin DM,
et al. A multisite study of the clinical diagnosis of different
autism spectrum disorders. Arch Gen Psychiatry. 2012; 69:306-13.
9. de Bosset V, Froehlich F, Rey JP, Thorens J,
Schneider C, Wietlisbach V, et al. Do explicit appropriateness
criteria enhance the diagnostic yield of colonoscopy? Endoscopy. 2002;
34:360-8.
10. Lord C, Risi S, Lambrecht L, Cook EH Jr,
Leventhal BL, DiLavore PC, et al. The autism diagnostic
observation schedule-generic: a standard measure of social and
communication deficits associated with the spectrum of autism. J Autism
Dev Disord. 2000; 30:205-23.
11. Lord C, Rutter M, Le Couteur A. Autism Diagnostic
Interview-Revised: a revised version of a diagnostic interview for
caregivers of individuals with possible pervasive developmental
disorders. J Autism Dev Disord. 1994;24:659-85.
12. Fischer RG. The Delphi method: a description,
review and criticism. J Acad Librarianship. 1978:64-70.
13. Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
Evaluating patient-based outcome measures for use in clinical
trials. Health Technol Assess. 1998; 2:1-74.
14. Schopler E, Reichler RJ, DeVellis RF, Daly K.
Toward objective classification of childhood autism: Childhood Autism
Rating Scale (CARS). J Autism Dev Disord. 1980; 10:91-103.
15. McColl E, Jacoby A, Thomas L, Soutter J, Bamford
C, Steen N, et al. Design and use of questionnaires: a review of
best practice applicable to surveys of health service staff and
patients. Health Technol Assess. 2001; 5:1-256.
16. Russell AJ, Mataix-Cols D, Anson MAW, Murphy DGM.
Psychological treatment for obsessive-compulsive disorder in people with
autism spectrum disorders – A pilot study. Psychother Psychosom. 2009;
78:59-61.
17. Kulsrestha SK. Stanford Binet Intelligence Scale
and Manual. Hindi Adaptation (Under third revision) Allahabad: Manas
Seva Sansthan Prakashan; 1971.
18. Doll EA. A generic scale of social maturity. Am J
Orthopsychiatry. 1935; 5:180-8.
19. Volkmar FR, Cicchetti DV, Dykens E, Sparrow SS,
Leckman JF, Cohen DF. An evaluation of the Autism Behavior Checklist. J
Autism Dev Disord. 1988; 18:81-97.
20. Spitzer RL, Siegel B. The DSM-III-R field trial
of pervasive developmental disorders. J Am Acad Child Adoles Psychiatry.
1990; 29:855-62.
21. Volkmar FR, Klin A, Siegal B, Szatmari P, Lord C,
Campbell M, et al. Field trial for autistic disorder in DSM-IV.
Am J Psychiatry. 1994; 151:1361-7.
22. McPartland JC, Reichow B, Volkmar FR. Sensitivity
and specificity of proposed DSM-5 diagnostic criteria for autism
spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2012; 51:368-83.
23. Ronald A, Happe F, Bolton P, Butcher LM, Price
TS, Wheelwright S, et al. Genetic heterogeneity between the three
components of the autism spectrum: A twin study. J Am Acad Child Adolesc
Psychiatry. 2006; 45:691–9.
24. Ronald A, Happe F, Price TS, Baron-Cohen S,
Plomin R. Phenotypic and genetic overlap between autistic traits at the
extremes of the general population. J Am Acad Child Adolesc Psychiatry.
2006; 45:1206–14.
25. Tanguay PE, Robertson J, Derrick A. A dimensional
classiûcation of autism spectrum disorder by social communication
domains. J Am Acad Child Adolesc Psychiatry. 1998; 37:271-7.
26. Tadevosyan-Leyfer O, Dowd M, Mankoski R, Winklosky
B, Putnam S, McGrath L, et al. A principal component analysis of
the Autism Diagnostic Interview-Revised. J Am Acad Child Adolesc
Psychiatry. 2003; 42:864-72.
27. Charman T, Taylor E, Drew A, Cockerill H, Brown
JA, Baird G. Outcome at 7 years of children diagnosed with autism at age
2: predictive validity of assessments conducted at 2 and 3 years of age
and pattern of symptom change over time. Child Psychol Psychiatry. 2005;
46:500-13.
28. Sigman M, McGovern CW. Improvement in cognitive
and language skills from preschool to adolescence in autism.
J Autism Dev Disord. 2005; 35:15-23.
29. Van Lang NDJ, Boomsma A, Sytema S, de Bildt AA,
Kraijer DW, Ketelaars C, et al. Structural equation analysis of a
hypothesized symptom model in the autism spectrum. J Child Psychol
Psychiatry. 2006; 47:37-44.
30. Boomsma A, Van Lang NDJ, De Jonge MV, De Bildt
AA, Van Engeland H, Minderaa RB. A new symptom model for autism
cross-validated in an independent sample. J Child Psychol Psychiatry.
2008; 49:809-16.
|
|
|
 |
|

