|
|
|
Indian Pediatr 2012;49: 411-412
|
 |
Isolated Cerebral Sinovenous Thrombosis: A
Rare Case of Neonatal Antiphospholipid Syndrome
|
|
De Carolis Maria Pia, *Salvi Silvia, Bersani Iliana and *De Carolis Sara
From the Division of Neonatology, Department of
Paediatrics; and *Department of Obstetrics and Gynecology, Catholic
University of Sacred Heart, Rome, Italy.
Correspondence to: Dr. Maria Pia De Carolis, Division
of Neonatology, Department of Paediatrics, University Hospital "A.
Gemelli", Catholic University of the Sacred Heart, Largo A. Gemelli, 8
00168 – Rome – Italy.
Email:
[email protected]
Received: May 31, 2011;
Initial review: June 24, 2011;
Accepted: August 20, 2011.
|
We describe a case of neonatal cerebral sinovenous thrombosis associated
with the presence of anti-phospholipid antibodies (aPL). We recommend
that in all cases of neonatal thrombosis, the couple mother-infant
should be extensively tested for the presence of both acquired (aPL) and
congenital thrombophilia.
Key words: Anticardiolipin, Antiphospholipid syndrome,
Neonate, Thrombosis.
|
|
Neonatal antiphospholipid syndrome (APS) is a
rare clinical entity characterized by neonatal thrombotic disease
due to the presence of antiphospholipid antibodies (aPL); its
occurrence may depend on the transplacental transfer or on the de
novo production of such antibodies. We describe a rare case of
isolated sinovenous thrombosis associated with anticardiolipin IgG (aCL
IgG) and anti-prothrombin antibodies.
Case Report
A full-term neonate (birth weight 3120 grams;
Apgar score 7 and 9 at 1 and 5 minutes, respectively) developed
severe respiratory distress due to pneumonia soon after his
delivery. During the first two weeks, his clinical condition
gradually improved; serially performed cerebral ultrasound
examinations were normal. On day 18, for the first time, a
hyperechoic area behind the right Sylvian fissure was highlighted by
routine cerebral ultrasound, in the absence of clinical
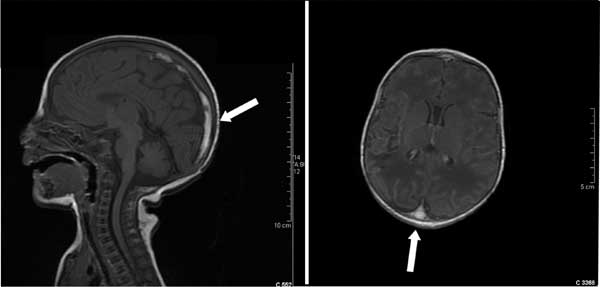
manifestations. Brain magnetic resonance imaging showed a right
parieto-temporal sub cortical malacic lesion associated with
thrombosis of the superior sagittal sinus. The lesion extended from
its medium third to the Torcular Haerophili (Fig 1)
and was confirmed by the magnetic resonance angiography. Coagulation
profile was normal; inherited thrombophilia was negative (antithrombin,
protein C and protein S were normal for the age, factor V Leiden and
G20210A prothrombin gene mutation were absent and total plasma
homocystein level was normal) while anticardiolipin (aCL) IgG (30 U/mL,
normal <19 U/mL) and anti-prothrombin IgG antibodies (61 U/ml,
normal <15 U/mL) were elevated.
 |
|
Fig. 1 Magnetic resonance imaging of the head
showing occlusion of the superior sagittal sinus.
|
His primpara mother, without familiar and
personal history of thromboses and autoimmune disease, was
additionally screened. Anti-prothrombin IgG and anticardiolipin IgM
(aCL IgM) were positive (30 U/mL and 19 U/mL, respectively) and
still present three months later.
On day 30, the neonate was discharged in good
clinical conditions. Neurologic examinations, performed on the 3 rd,
6th and 12th
months of life showed normal neurological
development.
Discussion
In the neonatal period, the aPL-related
thrombosis seems to be exceedingly rare, with only sixteen cases
reported between 1987 and 2007 and analyzed in a recent review [1].
Arterial thromboses represent about eighty percent of the reported
thromboses. To date, only three cases of venous thromboses are
described: two of these affected only peripheral circulation [2, 3];
while in the third case, both the peripheral and central circulation
were involved, since thrombosis of superior sagittal sinus with
right middle cerebral artery infarct was detected in association to
aortic and left renal artery thrombus [4].
Cerebral sinovenous thrombosis (CVT) occurs in
neonates with an incidence of at least 0.67 per 100,000 per year
[5]. However, this impact is likely underestimated for several
reasons as the lack of knowledge of this condition by many
clinicians, the difficulty in obtaining a correct radiological
diagnosis and, above all, the absence of a specific clinical
presentation [6]. In recent years, the diagnosis of neonatal CVT has
dramatically increased by the improved sensitivity of the
neuroimaging techniques and the more frequent application of cranial
imaging in the neonatal period.
It is necessary to consider several genetic and
acquired conditions that are predisposing factors for thrombosis in
neonatal age: inherited thrombophilias, aPL antibodies, and
additional perinatal conditions asphyxia, dehydration and infection.
The presence of aPL antibodies and infection are the only risk
factors for thrombotic event detectable in our patient. In the
present case, the occurrence of thrombotic phenomena is associated
with the presence of aPL antibodies. The presence of anti-prothrombin
IgG antibodies in the serum of both neonate and his mother suggests
the transplacental transfer of these antibodies. Instead, the aCL
IgG were positive in the neonate and negative in his mother.
Neonatal APS is rare, if not exceptional,
disease; it is likely that its rarity is attributable to the fact
that aPL alone are not sufficient to cause disease and others
factors are probably implicated. So, in the pathogenesis of neonatal
thrombosis, a second hit (usually an inflammatory event) is required
as an additional prothrombotic risk factor [7,8]. In the present
case, probably pneumonia was the second trigger event for the onset
of thrombotic event.
This case supports a previous reported
observation: not-treated women with unknown aPL are probably at
greater risk to have neonatal thrombosis then women successfully
treated with aspirin and low molecular weight heparin [9]. Motta,
et al. [7] proposed that heparin, when administered to the
mother during gestation, is able to bind circulating aPL, limiting
the transplacental transfer to the fetal circulation and thus
reducing their pathogenicity.
We recommend that in all cases of neonatal venous
and/or arterial thrombosis, the mother-infant pair should be
extensively tested for the presence of both acquired (aPL) and
congenital thrombophilia.
Acknowledgments: Papacci Patrizia (Department
of Pediatrics, Division of Neonatology, for echographic evaluation;
Costantino Romagnoli (Department of Pediatrics, Division of
Neonatology, Catholic University of Sacred Heart) and Angela Botta
(Department of Obstetrics and Gynecology for other support.
Contributors: All authors contributed
to the literature search, drafting manuscript. Final manuscript was
approved by all authors.
Funding: None; Competing interests:
None stated.
References
1. Boffa MC, Lachassinne E. Infant perinatal
thrombosis and antiphospholipid antibodies: a review. Lupus.
2007;16:634-41.
2. Contractor S, Hiatt M, Kosmin M, Kim HC.
Neonatal thrombosis with anticardiolipin antibody in baby and
mother. Am J Perinatol. 1992;9:409-10.
3. Hage ML, Liu R, Marcheschi DG, Bowie JD, Allen
NB, Maćk BG. Fetal renal vein thrombosis, hydrops fetalis, and
maternal lupus anticoagulant. A case report. Prenat Diagn.
1994;14:873-7.
4. Tabbutt S, Griswold WR, Ogino MT, Mendoza AE,
Allen JB, Reznik VM. Multiple thromboses in a premature infant
associated with maternal phospholipid antibody syndrome. J
Perinatol. 1994;14:66-70.
5. deVeber G, Andrew M, Adams C, Bjornson B,
Booth F, Buckley DJ, et al. Cerebral sinovenous thrombosis in
children. N Engl J Med. 2001;345:417-23.
6. Ramenghi LA, Govaert P, Fumagalli M, Bassi L,
Mosca F. Neonatal cerebral sinovenous thrombosis. Semin Fetal
Neonatal Med. 2009;14:278-83.
7. Motta M, Rodriguez-Perez C, Tincani A,
Lojacono A, Nacinovich R, Chirico G. Neonates born from mothers with
autoimmune disorders. Early Human Development. 2009;85:S67-70.
8. Meroni PL, Borghi MO, Raschi E, Tedesco F.
Pathogenesis of antiphospholipid syndrome: understanding the
antibodies. Nat Rev Rheumatol. 2011;7:330-9.
9. Boffa MC, Lachassinne E, Boinot C, De Carolis
S, Rovere-Querini P, Avcin T, et al. European registry of
babies born to mothers with antiphospholipid syndrome. A result
update. Lupus. 2009;18:900-4.
|
|
|
 |
|

