The Indian studies mostly cite screening facility
available to newborns brought in to tertiary hospitals. It is in this
context that a program to provide a centralized screening facility to
every hospital in the city at its doorstep for universal screening was
conceptualized and established in Cochin.
A two stage screening protocol with otoacoustic
emission (OAE) as the first screen, followed by auditory brainstem
response (ABR) for those who fail the first screen was introduced. This
two tier screening program (the second tier being more expensive) is
required only for a selected few – thus making the program practical and
viable. Trained personnel report to each particular hospital at a
particular time and day of the week. This protocol makes the screening
cost-effective and acceptable; it avoids the need for transporting the
neonates to a screening facility and thus significantly prevents dropouts.
This overall practicability makes it relevant for our country; making it a
potential model screening program.
Background
It is well recognized that unidentified hearing loss
can adversely affect optimal speech and language development, acquisition
of literacy skills, and academic, social and emotional development. The
risk is even more in a country like India where infrastructure is
abysmally inadequate for prevention and remediation. Neonatal hearing loss
and its developmental consequences are measurable before the age of 3
years [1-3]. If these are not remediated through early intervention, they
impact the child for life [4]. There is robust evidence that
identification and remediation of hearing loss, when done before 6 months
of age for newborn infants who are hard of hearing, enables them to
perform significantly higher on vocabulary, communication, intelligence,
social skills and behavior necessary for a successful later life [5-8].
American Academy of Pediatrics (AAP) in 1999 advocated universal new-born
hearing screening programme (UNHSP) and remedial intervention which is
being practiced in most of the developed countries. In a developing
country like India, the risk of infants to develop these disabilities is
obviously more [9,10]. In interventional programs, the Indian studies
mostly cite the screening facilities available to newborns brought in to
tertiary referral hospitals [11,12]. A hearing screening equipment
facility in every hospital with a maternity unit today may not be a viable
proposition. In this background, a practical interventional model was
conceived for the city of Cochin (which has 20 hospitals with maternity
units) in January 2003. At that time, there was no hearing screening
facility for neonates in most of the hospitals in the city. It was felt
that if successful, this centralized screening facility on a
cost-effective template can go on to become a solution and model for the
country.
Centralized Newborn Hearing Screening
The AAP Task Force on newborn and infant hearing
recommends UNHS by 3 months of age with intervention by 6 months of age.
The Joint Committee on Infant Hearing (JCIH) position statement provides
guidelines that include Newborn Hearing Screening (NHS) soon after birth,
before discharge from hospital, or before 1 month of age, diagnosis of
hearing loss through audiological and medical evaluation before 3 months,
and intervention through interdisciplinary programme for infants with
confirmed hearing loss before 6 months of age [13]. This screening
involves all newborns, with special attention to the high risk group which
include the following:
(i) family history of hereditary
childhood sensori-neural hearing loss;
(ii) in utero infection such as
cytomegalovirus, rubella, syphilis, herpes and toxoplasmosis;
(iii) craniofacial anomalies,
including those with morphological abnormalities of the pinna and ear
canal;
(iv) birth weight less than 1500 gms;
(v) hyperbilirubinemia at a serum
level requiring exchange transfusion;
(vi) ototoxic medications, including
but not limited to the aminoglycosides;
(vii) bacterial meningitis;
(viii) apgar score 0 to 4 at 1 minute, or 0
to 6 at 5 minutes;
(ix) mechanical ventilation lasting 5 days
or more; and
(x) stigmata or other findings associated in
the sensorineural and/or conductive hearing loss.
The Indian Academy of Pediatrics (IAP) Cochin Branch
mooted a centralized screening facility, initially for high risk screening
but quickly decided to choose the two-tier UNHS for all newborns. Despite
several neonatal intensive care units in the private and government
sectors in Cochin city, adequate screening facility was lacking.
Aware-ness programs and brainstorming were done with pediatricians and
obstetricians catering to those units to design an acceptable protocol.
Twenty major hospitals with maternity units catering to various
socioeconomic strata came on-board, and the program for centralized
newborn hearing screening (CNHS) facility was launched in January 2003.
Cochin Experience
Screening facility operates out of Child Care Centre,
which is also the secretariat of IAP Cochin Branch. We have acquired 3
portable screening machines. Personnel with basic knowledge in computer
and good communication skills were chosen, given basic training in hearing
screening. At present there are 3 screening machines and 3 screeners.
The co-ordination with the medical and nursing staff in
the neonatal units is done by the screener. She is also in-charge of the
screening register. The respective pediatrician apprises the parents of
the infant about the procedure and its need. As per guidelines, the
neonate gets screened before the day of discharge. If there is an abnormal
result, repeat test is done on the day of the infant’s next scheduled
visit. If the repeat test also is abnormal, the baby is referred for ABR
(available in most hospitals in the city). Babies with abnormal ABR are
referred to National Institute of Speech and Hearing (NISH), Trivandrum,
for comprehensive evaluation and remediation. The evaluator records the
medical history from the discharge card/inpatient file of the infant, to
identify the high risk factors recorded. High risk infants who miss
screening are screened on subsequent scheduled follow up visit. Screening
takes only about 3-4 minutes, if the baby is in natural sleep. Older
babies may require sedation. Babies requiring repeat test are given
specific dates by the hospitals for the scheduled follow up visits, so
that it will coincide with the visit of the screener.
OAE, ABR and Automated ABR (AABR) testing have all been
used in newborn hearing screening programs. ABR assesses auditory function
from the eighth nerve through the auditory brainstem. OAEs are used to
assess structural integrity and are physiologic measurements of the
response of outer hair cells of the cochlea to acoustic stimuli. They
serve as a fast objective screening test for normal cochlear function.
OAE tests are used to assess the outer, middle and
inner ear portions of the auditory system. ABR testing helps in assessing
the whole system, form periphery to the auditory nerve and brainstem. If
an infant has normal OAE and abnormal ABR, he may be having auditory
neuropathy or auditory dyssynchrony. The ABR and OAE are tests of
structural integrity of the auditory pathway and not tests of hearing;
therefore, even if ABR and OAE test results are normal, hearing cannot be
considered definitely normal until a child is mature enough for a reliable
behavioral audiogram. All infants, regardless of newborn hearing screening
outcome are recom-mended to receive ongoing monitoring for development of
age-appropriate auditory behaviors and communication skills. Any infant
who demonstrates delayed auditory and/or communication skill development,
even if he or she passed newborn hearing screening should receive an
audiological evaluation to rule out hearing loss. These are also
communicated to the parents by the pediatrician.
Over the period of 7 years from January 2003 till
December 2009, we screened a total of 10,165 babies and the incidence of
hearing loss as per our observation in the high risk group is 10.3 per
1000 and 0.98 per 1000 in the well baby group (Fig. 1).
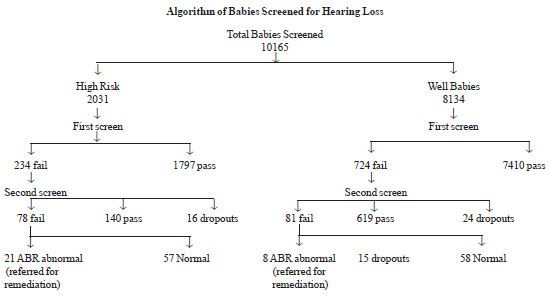 |
|
Fig. 1 Result of newborn hearing screening
for high risk and well babies. |
The relative advantages and disadvantages of a 2 stage
(OAE/ABR) protocol for newborn hearing screening need to be considered
carefully for individual circumstances. In locations where getting infants
to return for out patient screening and testing is very difficult, the
substantially lower failure rate that will likely be achieved by using
both OAE and ABR at the same sitting has significant advantages. In a
setting like ours, this may not be very practical, but has to be
considered wherever possible.
Problems Faced and Solutions
One challenge we initially faced was getting the infant
who failed the first screen for retest after 2 weeks (AAP guidelines).
This was solved by coinciding the immunization visit with that of
screening. Performing test at that age period was a little time consuming
because one has to wait for the baby to go to natural sleep. Another
challenge was convincing parents (in some cases grandparents) the need for
ABR in babies with abnormal OAE. It required counseling and cajoling,
which was time consuming. The biggest hurdle was convincing the need for
fixing a hearing aid in ABR abnormal babies, probably due to the stigma
attached to having a hearing aid. As the programme is gaining roots, these
are becoming easier.
Conclusions
UNHS has become a national practice in most developed
countries. The identification of all newborns with hearing loss before 6
months has now become an attainable realistic goal, as our program of UNHS
in Cochin now crosses 7 years and over 10 thousand cases. With our limited
data, it is too early to arrive at any conclusions or definite
interpretations yet. Our unique experience is still evolving.
Nevertheless, the detected cases represent a rate of about 1% hearing loss
among high risk newborns. This correlates well with national and
international figures and therefore calls for UNHS to be made a national
practice.
UNHS need not detect all cases of congenital hearing
loss - it only provides an indication of the baby’s hearing at the time of
the screening. Mild hearing loss and hearing loss outside the main speech
frequencies may not be detected. Hearing impairment may develop after the
neonatal period and therefore, it is crucial for the pediatrician to
encourage parents to continue to have their child’s hearing checked. The
pediatrician should maintain a high index of suspicion if there are
manifestations of hearing loss such as speech and language delay. Any
parental concern regarding a child’s hearing should also be thoroughly
investigated. At Cochin, we have instituted a practical model and a cost
effective protocol for early identification of hearing loss through a CNHS
facility. This can be replicated in other parts of the country with the
unified strength of pediatricians in every town.

