|
|
|
Indian Pediatr 2010;47: 409-414 |
 |
Reducing Use of Injections Through
Interactional Group Discussions: A Randomized Controlled
Trial |
|
R Bhunia, Y Hutin*, R Ramkrishnan, PK Ghosh
†,
S Dey# and M Murhekar
From the Field Epidemiology Training Programme (FETP),
National Institute of Epidemiology (NIE), Indian Council of Medical
Research (ICMR), Chennai; *WHO India country office, New Delhi; †Nilratan
Sircar Medical College and Hospital, West Bengal, and
#District Tuberculosis Centre, North 24
Parganas, West Bengal; India.
Correspondence to: Dr Rama Bhunia, 60A/1R, Dr S C
Banerjee Road, Kolkata, West Bengal 700 010, India.
Email: [email protected]
Received: July 21, 2008;
Initial review: August 13, 2008;
Accepted: April 24, 2009.
Published online: 2009
September.
PII:S097475590800456-1
|
|
Abstract
Objective: To determine whether "interactional
group discussions" could reduce prescriptions of injections by
physicians.
Study design: Randomized controlled trial.
Setting: Rural public health care facilities,
North 24 Parganas district, West Bengal, India.
Subjects: 72 medical officers, 36 each in
intervention and control groups.
Intervention: Interactional group discussions.
Outcome measure: Proportion of prescriptions
including at least one injection.
Results: In the intervention group, 249 of 1,080
prescriptions (23%) included at least one injection compared with 79 of
1,080 prescriptions (7%) before and after the intervention,
respectively. (RR: 0.32, 95% CI: 0.25-0.40). In the control group, 231
of 1,080 prescriptions (21%) included at least one injection before the
intervention vs 178 of 1,080 prescriptions (16%) after the
intervention (RR 0.77, 95% CI: 0.65-0.92).
Conclusion: Interactional group discussions
reduce prescription of injections.
Keywords: India, Injection use, Interactional group
discussion, Public health care facilities.
|
|
I
n 2000, in transitional and
developing countries, 16 billion injections were given (95%
therapeutic)(1-3). Of these, 40% were given with reused devices,
accounting for 40%, 30% and 2% of new hepatitis C virus, hepatitis B virus
and HIV infections, respectively(3). High rates of injection use amplify
transmission of blood borne pathogens(2,4). Thus, reducing injection use
is key to prevent injection-associated infections(5-7).
Some patients prefer injections(8-9).
However, qualitative research suggests that prescribers over-estimate the
preference for injections among patients, and that in most cases, patients
are open to use of oral medications(10,11). In fact, the second
International Conference on Improving Use of Medicine (ICIUM) underlined
that prescribers are the key target for interventions to reduce injection
use(6). In 1992, the first "interactional group dis-cussions" intervention
study conducted in Indonesia suggested that physicians prescribe fewer
injections when confronted with the actual absence of preference for
injections among patients(12). As a result, WHO designed an "interactional
group discussions" intervention guide that could be applied to countries
facing injection-associated infections(11-15).
In India, many therapeutic injections are unnecessary
and unsafe(16-23). We conducted a study to determine whether an "interactional
group discussions" intervention was effective at reducing injections use
among public sector medical officers in India.
Methods
Study population: Medical officers, formally
trained with MBBS degree, working in government rural health care
facilities of the North 24 Parganas district, West Bengal, India.
Operational definitions: A
therapeutic injection was defined as a skin-piercing procedure performed
with a syringe and needle to introduce a curative substance into a patient
by the intramuscular, intravenous or subcutaneous route. We excluded blood
transfusions, surgery, tattoos and vaccines.
Study design: We conducted a randomized controlled
trial from June to November 2007. The study consisted of three stages: (i)
a pre-intervention prescription survey; (ii) the "interactional
group discussions" intervention four weeks later during which medical
officers were confronted to community members (who according to past
experience with the method usually express to prescribers their absence of
preference for injections); and (iii) a post-intervention
prescription survey two months later. We randomized medical officers to
the intervention and control groups using a computer-generated random
number list and used quality assurance procedures to prevent any mix-up
after randomization. While we made use of qualitative methods for the
intervention, the study was quantitative in nature as we aimed at
measuring a reduction in injection use. We conducted seven interactional
group discussions to distribute medical officers in groups small enough to
interact with community members.
Sampling: We sampled medical officers on the
employment list from the 135 working in rural facilities (i.e.,
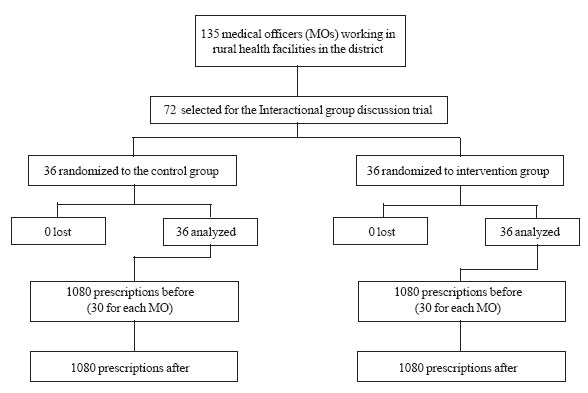
block primary health centres and primary health centres) (Fig. 1).
For each selected medical officer, we sampled every third prescription on
the day of the survey. We calculated the sample size on the basis of the
number of prescriptions to be analyzed before and after the intervention,
using the Epi Table Software. Our assumptions included a proportion of
prescriptions including at least one injection of 50% and 40% before and
after the intervention, respectively; an alpha error of 5% and a power of
99%. As the software generated an estimate of 925 prescriptions, we
anticipated 5% of non-response and therefore aimed at surveying 971
prescriptions before and after, for the intervention and the control
group. To round up and obtain an even count, we included 30 prescriptions
for 36 medical officers in the intervention and control groups, before and
after (30×36 = 1,080, twice)
 |
|
Fig. 1 Diagram summarizing the randomized
controlled trial. |
Data collection and analysis: Health workers
unaware of the intervention/ control status surveyed prescriptions of
medical officers from outpatient register without interviewing the medical
officer. The principal investigator verified 15% prescriptions. We
calculated the crude frequency of prescriptions, injections, the WHO "OT8
indicator" (i.e., the number of prescriptions including at least one
injection), the effect size [(% after - % before) intervention – (% after
- % before) control] and relative risks. We tested the significance of the
differences in the ratio of injections per 100 prescriptions before and
after in the two groups using a paired MacNemar Chi square(24).
Human subjects protection: We explained the
voluntary nature of participation and collected written informed consent
from participants, including medical officers (who were the target of the
intervention) and community members who took part in the discussions. We
ensured confidentiality through codes. The ethical committee of the
National Institute of Epidemiology, Chennai cleared the protocol.
Results
Age and sex distribution was comparable in the control
and intervention group (mean (±SD) age: 35 (±6.3) y vs 35 (±7.3) y;
M:F ratio: 33.3 vs 31.5; respectively). Overall, 17% of outpatients
were under 15 age group. Before the intervention, there were 37 injections
per 100 prescriptions in the intervention group versus 33 in the control
group (Table l). Commonly prescribed injections included
antiemetics, H 2 blockers,
antibiotics and vitamins.
TABLE I
Proportion of Prescriptions Including at Least One Injection Before and After the Intervention
| |
Proportion of prescriptions including at least one
injection |
| Stage of the study |
Intervention group |
Control group |
Relative risk |
| |
(n=1080) No. (%) |
(n=1080) No. (%) |
(95% CI) |
| Pre-intervention |
249 (23) |
231 (21) |
1.1 (0.92-1.3) |
| Post-intervention |
79 (7) |
178 (16) |
0.44 (0.35-0.57) |
After the intervention, the ratio of injections per 100
prescriptions decreased to 11 and 21 per 100, in the intervention and
control groups, respectively (P = 0.009). The proportion of
prescriptions including at least one injection decreased in both the
intervention and control group (Effect size: -11%). However, in the
control group, the reduction was larger among the 15 medical officers who
shared their assignment location with a medical officer who was part of
the intervention group than among 21 others (RR: 0.47, 95% CI: 0.36 – 0.63
vs. RR: 1.1, 95% CI: 0.86-1.4, respectively).
Discussion
Before the intervention, a high proportion of
prescriptions included injections in both the intervention and control
groups. After intervention, the proportion of prescriptions including at
least one injection reduced significantly in both groups. However, the
decrease was more marked in intervention group. Furthermore, in the
control group, the reduction was more marked among medical officers who
were assigned at a facility where a medical officer of the intervention
group worked.
Unsafe and high level of use of injections has been
reported previously in India(16-23). The effectiveness of our intervention
is consistent with the results of similar "interactional group
discussions" intervention studies conducted in Indonesia(12), Pakistan(13)
and Cambodia(14). In 1992, a controlled trial in Indonesia led to a
significant decrease in injection use in the intervention group compared
to the control group. However, in that study, there was also a decrease in
injection frequency in the control group, probably as a result of a
contamination of the intervention to the control group(13). More recently,
in Pakistan(25, 26), an intervention in a different target group -the
informal private sector-led to a significant reduction of injection use in
the intervention group in the absence of change in the control group(14).
A similar study in Cambodia led to a reduction in injection use in the
intervention group while there was no change in the control group(27).
The difference of effect between the intervention and
the control group was lower (–11%) in our study, than in Indonesia (–19%),
Pakistan (–32%) and Cambodia (–20 to –23%). A reduction in the proportion
of prescriptions including at least one injection in the control group in
our study may partly explain this smaller effect size. In the control
group, the reduction of injection use mostly occurred among those who
shared their health care facility of assignment with a medical officer of
the intervention group. This finding supports the hypothesis of a
contamination of intervention, as was the case in the Indonesian
study(12). This contamination is a
limitation of our study from a methodological standpoint (although
observing an effect despite the contamination that would dilute it
suggests that the effect does occur). However, from a public health
standpoint, it suggests that communication of results of the "interactional
group discussions" can be beneficial by itself, even though a prescriber
did not participate personally in the discussions.
Our study had two main limitations. First, the
post-intervention survey was conducted only once. Unlike the Indonesian
study, we were unable to conduct those at regular intervals for a
prolonged period to assess the sustainability of the intervention. As a
result, we could not conclude about the sustainability of the effect we
measured. Second, our post-intervention prescription survey was based on
outpatient registers only and was not validated by observations. Thus, we
could not exclude that the difference among groups exposed and unexposed
to the intervention was in fact a consequence of a desire to satisfy the
interviewer or of an observer-induced bias ("Hawthorne effect"). However,
even if that was the case, the differences in two groups suggest that the
intervention was at least successful in communicating the acceptable
standards to the target audience.
Our results support the findings of three comparable
trials in other countries and suggest that ‘interactional group
discussions" were also effective as an intervention to reduce
prescriptions of injections in the rural public health care facilities in
West Bengal, India. Our study also suggested that prescriber-to-prescriber
dissemination of the outcome of discussions could be effective by itself
in reducing injection prescription habits. On the basis of these
conclusions, we recommended scaling up similar intervention through "interactional
group discussions" sessions for more medical officers. Dissemination of
this message should help reducing injection use and prevent
injection-associated infections.
Acknowledgment
Dr Tapas Sen, State Public Health Cell and Dr Kusum
Kumar Adhikari, Chief Medical Officer of Health, North 24 Parganas
District of the Department of Health and Family Welfare, Government of
West Bengal.
Contributors: BR: Concept, design, acquisition of
data, analysis, interpretation and writing of manuscript; HY: Concept,
design, analysis and critical editing of manuscript; RR: Design, analysis
and interpretation; GPK: Acquisition of data, analysis and critical
revision of manuscript; DS: Acquisition of data, interpretation and
writing of manuscript; MM: Analysis, interpretation and writing of
manuscript.
Funding: ICMR, WHO, Government of West Bengal.
Competing interests: None stated.
|
What is Already Known?
• "Interactional group discussions" between
patients and prescribers is an effective strategy to reduce use of
medical injections.
What This Study Adds?
• "Interactional group discussions" were
effective in reducing prescriptions of injections among medical
officers in West Bengal, India.
|
References
1. Hutin Y, Hauri AM, Armstrong GL. Use of injections
in healthcare settings worldwide, 2000: literature review and regional
estimates. BMJ 2003; 327: 1075-1078.
2. Reeler AV. Anthropological perspectives on
injections: a review. Bull World Health Organ 2000; 78: 135-143.
3. Injection safety. Factsheet N° 231, revised October
2006. http://www.who.int/mediacentre/factsheets/fs231/en/. Accessed on
19th December, 2007.
4. Simonsen L, Kane A, Lloyd J, Zaffran M, Kane M.
Unsafe injections in the developing world and transmission of bloodborne
pathogens: a review. Bull World Health Organ 1999; 77: 789-800.
5. Dziekan G, Chisholm D, Johns B, Rovira J, Hutin Y.
The cost-effectiveness of policies for the safe and appropriate use of
injection in health care settings. Bull World Health Organ 2003; 81:
277-285.
6. Hutin YJF. Recent progress towards the safe and
appropriate use of injections worldwide. Essential Drugs Monitor 2005; 34:
6-7. Available at http://mednet2.who.int/edmonitor/34/67_Progress.pdf.
Accessed on 7 April, 2009.
7. Hutin Y, Hauri AM, Chiarello L, Catlin M, Stilwell
B, Ghebrehiwet T, et al. Best infection control practices for
intradermal, subcutaneous, and intramuscular needle injections. Bull World
Health Organ 2003; 81: 491-500.
8. Altaf A, Fatmi Z, Ajmal A, Hussain T, Qahir H,
Agboatwalla M. Determinants of therapeutic injection overuse among
communities in Sindh, Pakistan. Ayubmmed.edu.pk/JAMC/PAST/16-3/Arshadaltaf.htm.
Accessed on 19th December, 2007.
9. Murhekar MV, Rao RC, Ghosal SR, Sehgal SC.
Assessment of injection-related practices in a tribal community of Andaman
and Nicobar Islands, India. Public Health 2005; 119: 655-658.
10. Centres for Disease Control and Prevention.
Frequency of vaccine-related and therapeutic injections–Romania, 1998.
MMWR 1999; 48: 271-274.
11. WHO. Reducing injection overuse through patients-
prescribers interactional group discussions: A practical guide. Geneva:
WHO; 2003.
12. Hadiyono JE, Suryawati S, Danu SS, Sunartono,
Santoso B. Interactional group discussion: results of a controlled trial
using a behavioural intervention to reduce the use of injections in public
health facilities. Soc Sci Med 1996; 42: 1177-1183.
13. Agboatwalla M, Hutin Y, Luby S, Mussarat A. A pilot
intervention to improve injection practices in the informal private sector
in Karachi, Pakistan. Presentation given at the second International
Conference on Improving Use of Medicines (ICIUM), Chiang Mai, Thailand. 30
March-2 April 2004, abstract #AC 112.
14. Men C. Interactive group discussion: an
intervention to reduce the overuse of injections at public health care
facilities in Cambodia. Presentation given at the second International
Conference on Improving Use of Medicines (ICIUM), Chiang Mai, Thailand, 30
March-2 April 2004, abstract #AC051.
15. Massele A, Nsimba S, Kayombo E, Mugoyela V.
Reducing injection overuse through interactive group discussion with
patients and prescribers at primary care facilities in Dar es Salaam,
Tanzania. Presentation given at the second International Conference on
Improving Use of Medicines (ICIUM), Chiang Mai, Thailand, 30 March-2 April
2004, abstract#AD 025.
16. Hutin Y. Injection safety in India: From assessment
to policy changes (Assessment of injection practices in India 2004.
Presentation on behalf of An IndiaCLEN Program Evaluation Network (IPEN)
Study). In: Report of the Global Infection Control and Injection Safety
Meeting, pp. World Health Organization, WHO/EHT/04.17. Available at:
http://www.who.int/injection_safety/SIGNCPT FinalReportCleared.pdf.
Accessed 7 April, 2009.
17. Rajasekaran M, Sivagnanam G,
Thirumalaiko-lundu Subramainan P, Namasivayam K, Ravindranath C. Injection
practices in Southern part of India. Public Health 2003; 117: 208-213.
18. Kermode M, Muani V. Injection practices in the
formal & informal healthcare sectors in rural north India. Indian J Med
Res 2006; 124: 513-520.
19. Kermode M, Holmes W, Langkhan B, Thomas MS, Gifford
S. Safer injections, fewer infections: injection safety in rural north
India. Trop Med Int Health 2005; 10: 423-432.
20. Kotwal A, Priya R, Thakur R, Gupta V, Kotwal
J, Seth T. Injection practices in a metropolis of North India:
perceptions, determinants and issues of safety. Indian J Med Sci 2004; 58:
334-344.
21. Lakshman M, Nichter M. Contamination of medicine
injection paraphernalia used by registered medical practitioners in South
India: an ethnographic study. Soc Sci Med 2000; 51: 11-28.
22. Anand K, Pandav CS, Kapoor SK, Undergraduate Study
Team. Injection use in a village in north India. Nat Med J India 2001; 14:
143-144.
23. Narendranathan M, Philip M. Reusable needles-a
major risk factor for acute virus B hepatitis. Trop Doct 1993; 23: 64-66.
24. Dziekan G, Hutin Y. The effectiveness of
interventions to improve injection use: In: "Evidence and Information for
National Injection Safety Policies". (PhD dissertation), Uni Basel,
Switzerland. 2003, pp 71-82. Available at: http://pages.unibas.ch/diss/2003/DissB_6912.htm
Accessed 7 April, 2009.
25. Luby SP, Qamruddin K, Shah AA, Omair A, Pahsa O,
Khan AJ, et al. The relationship between therapeutic injections and
high prevalence of hepatitis C infection in Hafizabad, Pakistan. Epidemiol
Infect 1997; 119: 349-356.
26. Khan AJ, Luby SP, Fikree F, Karim A, Obaid S,
Dellawala S, et al. Unsafe injections and the transmission of
hepatitis B and C in a periurban community in Pakistan. Bull World Health
Organ 2000; 78: 956-963.
27. Vong S, Perz JF, Sok S, Som S, Goldstein S, Hutin
Y, et al. Rapid assessment of injection practices in Cambodia,
2002. BMC Public Health 2005; 5: 56.
|
|
|
 |
|

