From the Department of Cardiology, P.D. Hinduja
Hospital and Medical Research Centre and *Glenmark Cardiac Centre,
Mumbai 400 016, India.
Correspondence to: Dr. Yashkhandwala, P.D. Hinduja
Hospital and Medical Research Center, Veer Savarkar Marg, Mahim,
Mumbai 400 016, India.
E-mail:
[email protected]
Manuscript received: February 1, 2002; Initial
review completed: February 25, 2002; Revision accepted: January 1,
2003.
A two-month-old child having WPW syndrome and
orthodromic tachycardia was on treatment with digoxin, flecainide and
amiodarone. Despite this, he continued to have severe, very frequent
episodes of tachycardia. The left-sided accessory pathway was hence
ablated via a patent foramen ovale.
Key words: Arrhythmia storm, pre-excitation, WPW syndrome.
Radiofrequency ablation (RF) is the standard
treatment for symptomatic WPW syndrome. Usually this procedure is not
performed in very small children due to technical limitations. The case
reported herein was undertaken as a last resort.
Case Report
A one-month-old child born as a full term normal baby
was referred to us with a diagnosis of WPW syndrome. The child first had
an episode of paroxysmal tachycardia at the age of 15 days. Since then
the child had experienced 2 more episodes. During the episodes, the
child would appear limp. The ECG revealed narrow QRS tachycardia at 250
beats/min. The ECG in sinus rhythm suggested a left sided accessory
pathway. The tachycardia could be terminated by intra-venous adenosine.
The child had been started on digoxin and amiodarone. These medica-tions
were continued and a weekly follow-up was advised. The echocardiographic
exam-ination was normal; a patent foramen ovale was seen. Since the
child continued to have episodes of tachycardia, flecainide 1 mg/kg
twice a day was added. Despite this, episodes of tachycardia continued.
At the age of 2 months the child, weighing 3.2 kg was admitted in the
intensive pediatric care unit with tachycardia storm. In a period of 24
hours he had six episodes of orthodromic tachycardia, every time
requiring 1.5 mg/kg adenosine. In view of his precarious state, a
"rescue" ablation was considered.
The procedure was performed under general anesthesia.
Both femoral veins were accessed percutaneously. A 4-F quadripolar
electrode catheter (Bard) was introduced via the left femoral vein into
right ventricle. A 5F (Medtronic) ablation catheter with a 4 mm tip was
introduced via the right femoral vein into the right atrium. Orthodromic
tachycardia was easily inducible and could be terminated by ventricular
extra stimuli. The ablation catheter was passed into the left atrium
through the patent foramen ovale. An early activation site was found in
the left lateral region (Fig. 1). Transient "bumping" of the
pathway was noted by catheter contact. Radiofrequency energy at this
site led to immediate abolition of pre-excitation (Fig. 2). The
peak temperature setting was kept at 60ºC and the maximum temperature
achieved was 53ºC. The ECG next day showed that the preexcitation had
returned. In view of this, flecainide was continued while amiodarone was
stopped. Over the next 5 months the child has not had a single episode
of tachycardia. Digoxin was stopped at 7 months of age. Serial ECGs have
revealed intermittent pre-excitation. He is growing well with normal
milestones. His echocardiogram revealed mild mitral regurgitation but no
structural abnormality of the mitral valve apparatus was seen. At the
last follow up the weight was 9 kg at 11 months of age.
 |
 |
|
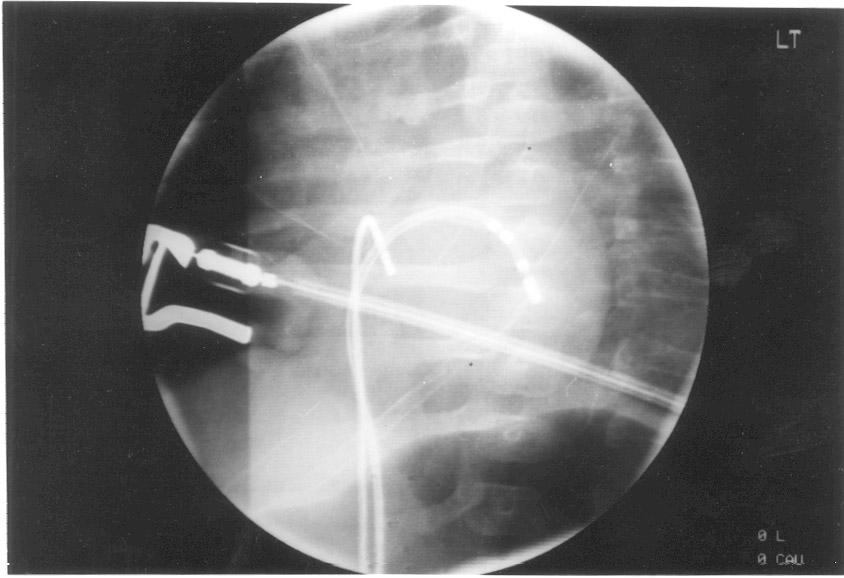
Fig. 1. Fluoroscopy of successful RF
ablation site. (a) 20º RAO, 10º cranial angulation. The ablation
catheter is on mitral annulus across the patent foramen ovale. The
diagnostic catheter is in the right ventricle. (b) 40º LAO view.
The ablation catheter tip is seen in the left lateral region. |
 |
|
Fig. 2. RF energy delivery. Preexcitation is
abolished from 10th QRS complex onwards. The initial 9 QRS
complexes show a negative delta wave in lead aVF and a positive
delta wave in lead V1, which disappear later. |
Discussion
RF ablation is rarely performed in infancy. The small
diameter of femoral vessels imposes severe limitations on catheter
choices. Apart from vascular complications, there are concerns of damage
to the fragile intracardiac structures at such a tender age. We
undertook RF ablation after all other measures had failed. The return of
pre-excitation in our patient was unusual, because adenosine had
demonstrated transient AV block after RF ablation. The intermittent
nature of pre-excitation at follow-up is indicative of a long antegrade
refractory period of the accessory pathway. The absence of tachycardia
recurrence suggests that retrograde conduction over the pathway has been
markedly diminished, if not eliminated by the RF ablation.
There are apprehensions regarding increase in RF
lesion size with growth based on studies in lambs(1). Hence RF ablation
in infancy is undertaken only when severe tachycardia persists despite
adequate trial of drug therapy. There are several reported series of RF
ablation in children(2,3,4), but the proportion of infants in these
studies have been very small. Our patient is the youngest reported
hitherto from India. A previous report from India(5) highlighted a
similar problem in a thirteen month old child. The mild mitral
regurgitation noted in our patient has been well tolerated. It is
possible that the RF lesion in some way has led to this regurgitation.
However the absence of any visible damage to the leaflets or chordae is
reassuring. The satisfactory clinical progress that we observed indicate
a good prognosis in this regard.
Contributors: BD conducted initial clinical and
echocardiographic evaluation, CKP assisted in the RF ablation procedure,
KC assisted in the management and help in writing the manuscript, YL
helped in patient care and preparation of the manuscript and will act as
guarantor of the paper.
Funding: None.
Competing Interests: None stated.
