|
|
|
Indian Pediatr 2019;56: 114-118 |
 |
Endoscopic Retrograde
Cholangiopancreaticography in Children: A Single-center
Experience From Northern India
|
|
Amol Sonyabapu Dahale, Amarender Singh Puri, Sanjeev
Sachdeva, Siddharth Srivastava and Ajay Kumar
From Department of Gastroenterology, GB Pant
Hospital, New Delhi, India.
Correspondence to: Dr Amarender Singh Puri,
Director-Professor and Head of the Department of Gastroenterology, GB
Pant Hospital, New Delhi 110 002, India.
Email:
[email protected]
Received: October 06, 2017;
Initial review: March 05, 2018;
Accepted: December 29, 2018.
|
|
Objective: To evaluate spectrum,
efficacy and safety of Endoscopic retrograde cholangiopancreatography
(ERCP) in pediatric population. Methods: Retrospective case
record review of pediatric patients (age
£15 y)
undergoing ERCP between January 2011 to June 2015 at a tertiary care
referral hospital in New Delhi, India. The Indications for ERCP,
cannulation success rate, procedure success rate and complications were
recorded. Results: The mean (SD) age of the participants were
11.5 (3) years. 164 ERCP procedures were done in 126 patients (67
males). All procedures were done under conscious sedation. The common
indications for ERCP were choledocholithiasis (50, 30.5%), chronic
calcific pancreatitis (38,23.2%), main pancreatic duct injury with leak
(21,12.8%), and bile leak (12,7.3%). The cannulation success rate was
90.4% (114 out of 126), while procedural success rate was 86% (141 out
of 164). Overall 8 complications were encountered; all were successfully
managed conservatively. Conclusions: ERCP in children can be
successfully performed at centers with such expertise.
Keywords: Choledocholithiasis, Diagnosis,
Endoscopy, Management.
|
|
T
herapeutic endoscopic retrograde
cholangiopancreaticography (ERCP) is an important modality for managing
biliopancreatic diseases in adults. After the first report of ERCP in a
child in 1976, it has been used extensively in the pediatric population
over the time establishing its role; with efficacy and safety comparable
to adults [1-7]. However, most studies in pediatric patients are from
the developed countries with limited reports from low- and middle-income
countries [8-11]. We aimed to share our experience of ERCP in pediatric
patients with emphasis on spectrum of diseases, efficacy and safety.
Methods
Data for this retrospective study was collected from
records of patients undergoing ERCP at GB Pant Hospital, New Delhi from
January 2011 to June 2015. Patients from pediatric age group (age
£15 years) were
included. The following data were reviewed and analyzed: indications of
ERCP, sedation used, successful cannulation of desired duct, ERCP
findings, therapeutic interventions performed technical success,
compli-cations and follow up if available. The ERCP related
complications were defined as per American Society for Gastrointestinal
Endoscopy definitions [12]. Bile leaks were classified into low grade
(leak identified only after opacification of intrahepatic duct system)
and high grade (leak observed before opacification of intrahepatic duct
system) [13]. Patients with incomplete data were excluded from the
study. Informed consent was waived by the institutional ethical
committee as the data were retrospective.
All the ERCP procedures were performed by adult
gastroenterologists using Olympus adult duodenoscope. A combination of
intravenous midazolam and propofol/ketamine in appropriate dosage was
used for sedation [14]. Statistical analysis was done with SPSS version
19.0.
Results
A total of 11,179 ERCP procedures were performed
during study period; of these, 170 were performed in children. Complete
data were available for 164 procedures. These 164 procedures were done
in 126 children (67 boys) with mean (SD) age of 11.5 (3) years (range
1-15 years). Thirteen children were aged below 5 years. Thirty-eight
(23%) were repeat procedures. Only seven ERCPs were diagnostic, while
157 (95.7%) were therapeutic. Indications of ERCP were:
choledo-cholithiasis (50, 30.5%), chronic calcific pancreatitis (CCP)
(38, 23-2%), pancreatic duct disruption (21, 12.8%), choledochal cyst
with cystolithiasis (CDC) (12, 7.3%), bile leak (12, 7.3%) and biliary
ascariasis (7, 4.3%) (Table I). Successful cannulation of
the naïve duct was achieved in 90.4% (114 out of 126) patients (biliary
93%, pancreatic 85%) and procedure was completed in 86% (141 out of
164). Biliary interventions done were: sphincterotomy in 70, stone
extraction in 22, stenting in 30 and removal of ascaris in 3 procedures.
Of 37 children with choledocholithiasis, 18 had calculus, and in 15
calculi were extracted. Calculus extraction was also done in 7 children
with CDC. In nine children with suspected biliary leak, seven had leaks
(4 minor, 3 major, 6 post-cholecystectomy leak, 3 post-traumatic).
Biliary sphincterotomy was performed in all nine patients with stent
being placed in three patients. In seven children with suspected biliary
ascariasis, ascaris was seen and removed in three children. In benign
biliary stricture, all patients were stented (4 post cholecystectomy, 1
tubercular). Patient with tuberculosis had periportal necrotic lymph
nodes causing compression at lower end, probably eroding into it. After
ERCP, jaundice improved; complete improvement was noted with
antitubercular therapy, and stent was removed later. In three children
with hydatid cyst, no communication could be seen. Two patients with
portal biliopathy, one patient with pancreatic malignancy and one
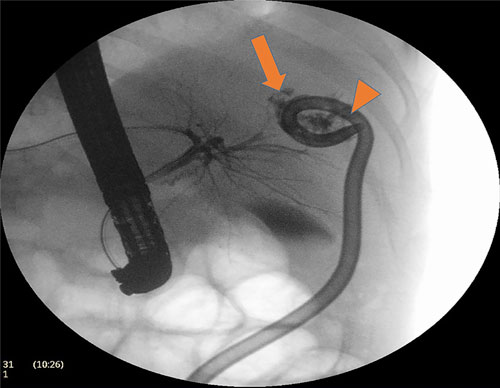
patient having liver abscess with biliary communication (Fig.
I) also underwent biliary stenting.
TABLE I Indications for Endoscopic Retrograde Cholangiopancreaticography in Children ≤15 Years (N=126)
|
Indication |
Number of procedures/patients |
|
Biliary Indications |
|
|
Choledocholithiasis
|
50/37
|
|
Choledochal cyst/Cystolithiasis
|
12/8
|
|
Biliary leak
|
12/9
|
|
Ascariasis
|
7/7
|
|
Benign biliary stricture
|
5/5 |
|
Hydatid cyst with biliary communication
|
3/3
|
|
Portal biliopathy
|
2/2
|
|
Liver abscess with biliary communication
|
1/1
|
|
Pancreatic tumour/Biliary obstruction |
1/1
|
|
Choledochal cyst (diagnostic)
|
3/3
|
|
Periampullary carcinoma (diagnostic)
|
1/1
|
|
Primary sclerosing cholangitis (diagnostic)
|
1/1
|
|
Pancreatic Indications
|
|
|
Chronic pancreatitis
|
38/24
|
|
Pancreatic leak
|
21/17
|
|
Pseudocyst
|
3/3 |
|
Recurrent acute pancreatitis
|
2/2
|
|
Pancreatic divisum |
2/2
|
 |
|
Fig. 1 Cholangiogram showing liver abscess with drain
in situ (arrowhead) with biliary communication (arrow).
|
Sixty-six procedures were performed on 48 children
with pancreatic disease. The interventions done were ncterotomy in
46, duct stenting in 20, and stone removal in nine children. Twenty-four
cases with CCP underwent endotherapy for pain. Major pancreatic duct
dilatation was seen in 18, whereas stricture and ductal calculi were
each seen in ten each. Stricture dilatation was done in eight patients,
followed by stenting. Thirteen patients had pain improvement at three
months, but long-term follow-up of these patients was not available.
Pancreatic duct leak was documented in 17 children with duct disruption;
sphincterotomy was done in all with stenting in 10 children.
Post-traumatic leak was most common etiology (13), followed by acute
pancreatitis (2); one each had CCP and post-surgical duct leak. Three
children underwent transpapillary drainage for pancreatic pseudocyst. In
two children with pancreatic divisum, minor duct sphincterotomy was
done, while two children having recurrent acute pancreatitis underwent
ERCP for diagnostic purpose.
Twelve patients had cannulation failure [mean (SD)
age: 11 (2) years]. Five of these had chronic pancreatitis, four had
choledocholithiasis, two had pancreatic duct leak while one had biliary
leak. Repeat procedure was attempted in ten patients and was successful
in nine of them. Two failures were sedation related, and repeat
procedure was successful. Eight (4.8%) children developed complications
following the ERCP procedure: mild pancreatitis (2), retro-peritoneal
duodenal perforation (2), sphincterotomy-related bleed (2) and hypoxia
(2). All were managed conservatively, and there was no mortality.
Discussion
ERCP is still underutilized in pediatric patients,
especially in low- and middle-income countries. In 164 ERCP procedures
in 126 patients, we observed good observed cannulation success (90.4%)
and procedure completion rate (86%). The most common indication for the
ERCP procedure was choledocholithiasis, followed by chronic
pancreatitis. Complications occurred in very few patients, and all of
them were successfully managed conservatively.
The main limitations of this study is retrospective
nature of data. Long-term follow-up is not available, which is
especially more relevant to endotherapy in chronic pancreatitis.
Moreover, risk factors for complications could not be studied due to
small number.
Only few studies have been published from India till
date on pediatric ERCP, two of these studies were primarily diagnostic.
Sharma, et al. [8] studied 8 patients with CDC preoperatively
(all diagnostic), while Poddar, et al. [9] reported a series in
which 84% procedures were diagnostic. Two recently published studies
from India, which report therapeutic ERCPs, focused mainly on pancreatic
disorders [10,11]. Majority of the procedures were done for pain in CCP.
In comparison, the present study described the whole pediatric ERCP
spectrum. Present study had choledocholithiasis in biliary group while
CCP in pancreatic group as the most common indication for ERCP, which is
comparable with recent reports [3,7]. This study also had cannulation
success rate of 90% which is slightly less compared to 95% from
published studies, but complication rate in present study was also less
compared to these studies (4.8% vs 7.7%) [4,6]. We used conscious
sedation in all compared to the practice in Western countries where
majority use general anesthesia [9].
In conclusion, our study suggests that ERCP is safe
and effective in pediatric population. Also, conscious sedation may be
safely used in pediatric population.
Contributors: ASD: designed the study, acquired,
analyzed and interpreted the data. He also drafted manuscript and
revised it critically for intellectual content; ASP: substantial
contribution to design of work and interpretation of data. He was also
involved in drafting of work as well as its revision regarding
intellectual content; SS: contributed to design of study and interpreted
data. He revised the draft critically for its intellectual content; AK:
contributed to acquisition, analysis and interpretation of data. He
contributed to manuscript drafting as well as critically revising it.
All authors approved the final version of manuscript, and agree to be
accountable for its accuracy and integrity.
Funding: None; Competing
interest: None stated.
|
What This Study Adds?
• Pediatric ERCP is safe and efficacious with
acceptable adverse event rate.
• Conscious sedation seems to be effective and safe in
children during ERCP procedure.
|
References
1. Waye JD. Endoscopic retrograde
cholangiopancreato-graphy in the infant. Am J Gastroenterol.
1976;65:461-3.
2. Varadarajulu S, Wilcox CM, Hawes RH, Cotton PB.
Technical outcomes and complications of ERCP in children. Gastrointest
Endosc. 2004;60:367-71.
3. Cheng CL, Fogel EL, Sherman S, McHenry L, Watkins
JL, Croffie JM, et al. Diagnostic and therapeutic endoscopic
retrograde cholangiopancreatography in children: A large series report.
J Pediatr Gastroenterol Nutr. 2005;41:445-53.
4. Enestvedt BK, Tofani C, Lee DY, Abraham M, Shah P,
Chandrasekhara V, et al. Endoscopic retrograde
cholangio-pancreatography in the pediatric population is safe and
efficacious. J Pediatr Gastroenterol Nutr. 2013;57:649-54.
5. Pant C, Sferra TJ, Barth BA, Deshpande A, Minocha
A, Qureshi WA, et al. Trends in endoscopic retrograde
cholangiopancreatography in children within the United States,
2000-2009. J Pediatr Gastroenterol Nutr. 2014; 59:57-60.
6. Giefer MJ, Kozarek RA. Technical outcomes and
complications of pediatric ERCP. Surg Endosc. 2015;29: 3543-50.
7. Troendle DM, Fishman DS, Barth BA, Giefer MJ, Lin
TK, Liu QY, et al. Therapeutic endoscopic retrograde
cholangiopancreatography in pediatric patients with acute recurrent and
chronic pancreatitis: Data from the INSPIRE (International Study Group
of Pediatric Pancreatitis: In search for a cuRE) study. Pancreas.
2017;46:764-9.
8. Sharma AK, Wakhlu A, Sharma SS. The role of
endoscopic retrograde cholangiopancreato-graphy in the management of
choledochal cysts in children. J Pediatr Surg. 1995;30:65-7.
9. Poddar U, Thapa BR, Bhasin DK, Prasad A, Nagi B,
Singh K. Endoscopic retrograde cholangiopancreaticography in the
management of pancreaticobiliary disorders in children. J Gastroenterol
Hepatol. 2001;16:927-31.
10. Agarwal J, Nageshwar Reddy D, Talukdar R,
Lakhtakia S, Ramchandani M, Tandan M, et al. ERCP in the manage-ment of pancreatic
diseases in children. Gastrointest Endosc. 2014;79:271-8.
11. Poddar U, Yachha SK, Borkar V, Srivastava A,
Saraswat VA. Clinical profile and treatment outcome of chronic
pancreatitis in children: a long-term follow-up study of 156 cases.
Scand J Gastroenterol. 2017;52:773-8.
12. Anderson MA, Fisher L, Jain R, Evans JA,
Appalaneni V, BenMenachem T, et al. Complications of ERCP.
Gastrointest Endosc. 2012;75:467-73.
13. Sandha GS, Bourke MJ, Haber GB, Kortan PP.
Endoscopic therapy for the bile leak a new classification: results in
207 patients. Gastrointest Endosc. 2004;60: 567-74.
14. Chung HK, Lightdale JR. Sedation and monitoring
in the pediatric patient during gastrointestinal endoscopy. Gastrointest
Endosc Clin N Am. 2016;26:507-25.
|
|
|
 |
|

