he World Health Organization
(WHO) Framework for Action on Interprofessional Education (IPE) and
Collaborative Practice has defined IPE as "an approach where
students from two or more professions learn about, from and with each
other" [1]. Centre for Advancement of Interprofessional Education
recognizes IPE as "occasions when members or students of two or more
professions learn with, from and about each other to improve
collaboration and the quality of care and services" [2].
As is evident from the definition, IPE stresses the
need for collaborative learning among learners drawn from different
streams of health care profession viz. – medical profession, nursing,
dental, physiotherapy and pharmaceutical professions. It must be
differentiated from multiprofessional education which is defined as
"occasions when two or more professions learn side by side for whatever
reason", thus defying any chance of collaborative and interdependent
learning [3].
Building the Case for Interprofessional Education and
Practice
The case-study (Box 1) provides
a classic description about the range of problems faced by health care
professionals due to lack of interprofessional coordination and
collaboration which may compromise the quality and safety of patient
care. In this backdrop, we discuss the curricular need to invest in
inter-professional education (IPE) to address the collaborative failures
featured in this case. IPE is recommended as an alternative to address
the current maladies associated with education and working in silos. The
paper shall delineate the way an interprofessional approach can offer
healthcare professionals with the much-required competencies in
providing a team based collaborative care. Besides highlighting the
range of fundamental issues related to IPE and inter-professional
practice (IPP), the review also attempts to emphasize the need for
patient centeredness and collaborative leadership.
|
BOX 1 Case Study to Illustrated Need for
Interprofessional Coordinations
N was brought to a pediatrician at the age of 2
years. Parents were concerned about his poor health. He weighed 10
kg, often had chest infections, and seemed to be developmentally way
behind peers in the community. N was operated at birth for duodenal
atresia and parents were told that he has a genetic problem that has
no cure. The family was on a regular follow up with their surgeon at
a tertiary care teaching hospital, until one year of age. After that
they had visited local doctors as and when required. Examination
revealed the child to have Down syndrome and malnutrition (PEM Grade
II). His developmental age was 9-12 months. The child also had a
pathologic cardiac murmur.
The pediatrician discussed Down syndrome with the
parents with overt surprise that they had not consulted him earlier
for vaccinations, infections, or poor growth and development. She
was dismayed over the past consultations that overlooked the
pertinent needs of an infant with Down syndrome. Later,
investigations revealed hypothyroidism and a ventricular septal
defect. Suitable medical management was started. Further follow-up
to plan growth monitoring and initiation of vaccination was
discussed with the parents.
|
Introduction to Interprofessional Education and
Practice
IPE provides opportunities for learners from
different health professions to come together to learn "from", "with"
and "about" each other [1]. This may be a starting point of coordinated
care among physicians, nurses, pharmacists and healthcare workers to
enhance patient outcomes. It reinforces a team-based approach towards
collaborative care.
With improved technology and new diagnostic and
treatment options available, healthcare is becoming complex day-by-day.
With the dawn of corporate-health culture, team-based and collaborative
approach to health care is establishing itself as the norm rather than
the exception. Though a healthcare team is assumed to work as a cohesive
unit, it is not uncommon to see health team members blaming each other
for patients’ problems and unfavorable health outcomes. Although the
contemporary health care requires ability to work in a team – and the
team is expanding, yet we never teach the students how to work with
other members.
Lack of knowledge to work as and in a health care
team, over-the-board assumption of superiority of one’s profession, and
cultural and communication gaps may be some of the reasons for failure
to work as a team. It has been reported that failure to learn and work
as healthcare team is resulting in poor patient-related outcomes. More
than a decade ago, it was reported that 70% of adverse events in
patient-care were avoidable. Report stated that these adverse events
were due to ‘compartmentalized and fragmented’ type of approach of
patient care and this fragmentation of care was preventing advancement
of patient care and patient safety [4]. A coherent and collaborative
approach to learn and work is the need of the hour.
Why Interprofessional Education?
It is assumed that if members of different
professions learn with, from, and about one another, they will
collaborate and work better together to progress in their professional
field as well as they will render improved services to the patients
resulting in improved clinical outcomes and quality of care being
provided to the patients [5]. The fragmented way in which healthcare is
being provided to the patients, and the disconnect between different
professions engaged in patientcare are often cited as barriers in
providing best healthcare to the patients [6]. It is argued that IPE
will ultimately produce a work-force ready for collaborative practice
guided by local health needs while working with the local health
infrastructure [4]. In a sense, IPE and collaborative practice is
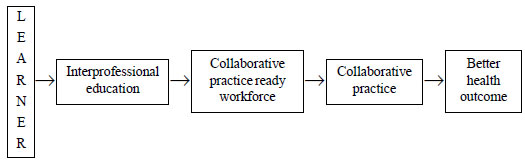
interdependent and the concept is detailed in Fig. 1 [7].
 |
|
Fig. 1 Interdependence of
interprofessional education and collaborative practice leading
to better health outcomes.
|
A judiciously planned and systematically introduced
and conducted IPE program can enhance flexible, complementary,
patient-centered, and cost-effective coordination in interprofessional
teams while at the same time recognizing requirements of each profession
in the team and safeguarding profession-specific identity [8]. The
resultant collaborative practice and interpro-fessional care is proposed
to be a significant intervention to provide quality care; and an
efficient, cost-effective mode of healthcare [9-11].
Interdisciplinary integration has also been
documented as the tenth-level of integration in the 11-step ladder of
integrated teaching learning by Harden [12]. Interdisciplinary teaching
has been defined as ‘a study of a phenomenon that involves the use of
two or more academic disciplines simultaneously’ [13]. Evidently, as a
concept, IPE draws its basis from interdisciplinary integrated teaching,
thus bolstering the need of such an educational innovation in the arena
of medical education. Some of the benefits of IPE are detailed in
Box 2.
|
BOX 2 Benefits of Interprofessional
Education
Educational benefits
• Students will work in pragmatic conditions and
will encounter real world experiences
• Teaching faculty from different professions
will offer contributions for program development and implementation
bringing in wide range of experiences
• Will bolster mutual respect and trust among the
professionals involved
• Will give opportunities to develop competencies
to work as a team and develop leadership qualities
• Understanding of professional roles
• Enhanced communication and negotiation skills
and professionalism
• Students will learn about the modalities and
skills of other professional streams
Health policy benefits
• There will be improved workplace based
practices
• Improved patient/client-centered care and
quality enhancement
• Clinical and patient outcomes will be improved
• Staff confidence, self-esteem and morale will
be improved
• With collaborative and team based work culture,
patient safety will be improved
• Health care will be more cost-effective
• Access to health-care facilities will be
improved
• Emergency patient care and disaster management will be improved
|
Core Competencies in Interprofessional Education
The crux of an interprofessional curricular design
centers around the core interprofessional competencies viz.
values and ethics of interprofessional practice, agreed roles,
interprofessional communication, sound team work principles, and being
patient-centered [14].
IPE core competencies should be based upon some basic
principles, viz. they should be patient/family-centered;
community/population-oriented, relationship-focused and
process-oriented; should be aligned to teaching learning strategies and
assessment methods that are developmentally appropriate for the learner;
should be contextual and applicable across involved practice-settings;
should be applicable across all involved professions; must be stated in
language understood, common and meaningful across the professions; and
must be outcome driven [14].
Barr proposed three types of core competencies from
IPE perspective, viz. common, collaborative, and complementary
competencies [15]. Common compe-tencies are those which are expected to
be possessed by all health professionals. Complementary competencies
help other professions to improve the quality of patient care.
Collaborative competencies are the ones that each profession involved
needs to develop together with others, like other specialties within
their own profession, between different professions, with non-government
organizations and health volunteers, with patients, attendants and
families, within the community etc.
Values and ethics for interprofessional practice:
Ethical values hold the fort, not only for interprofessional working,
but for healthcare professional in general too; but with
interprofessional collaboration, holding high ethical virtues become
more important and become part of interprofessional professionalism.
Interprofessional Professionalism Collaborative has defined
interpro-fessional professionalism as ‘‘consistent demonstration of core
values evidenced by professionals working together, aspiring to and
wisely applying principles of altruism, excellence, caring, ethics,
respect, communi-cation, and accountability to achieve optimal health
and wellness in individuals and communities’’ [16]. Tavistock group
suggests ethical principles in interprofessional working as ‘ethical
principles for everybody in health care to hold in common, recognizing
the multidisci-plinary nature of health delivery systems’ [17]. An
expert panel has defined ten competency statements under values and
ethics for interprofessional practice core competency; some of them are
listed in Box 3 [14].
|
BOX 3 General Competency Statements for
Inter-Professional Core Competency
Value and ethics for interprofessional practice
• Interests of patients and populations are
placed at the center of interprofessional health care delivery while
maintaining privacy and confidentiality of the patients.
• Cultural diversity and individual differences
that characterize patients, populations, and the health care team
are respected.
• Work in cooperation with those who receive
care, those who provide care, and others who contribute to or
support the delivery of prevention and health services, in a
trusting relationship.
• Demonstrate high standards of ethical conduct
and quality of care in one’s contributions to team-based care and
manage ethical dilemmas specific to interprofessional patient/
population centered care situations while maintaining one’s own
professional competence.
Roles and responsibilities for collaborative
practice
• Communicate one’s roles and responsibilities
clearly to patients, families, and other professionals while
recognizing one’s professional limitations and is able to explain
the roles and responsibilities of other care providers and how the
team works together to provide care.
• Forge interdependent relationships with other
professions to improve care and advance learning, thus engaging in
continuous professional and interprofessional development to enhance
team performance
Interprofessional communication
• Choose effective communication tools and
techniques, including information systems and communication
technologies, to facilitate discussions and interactions that
enhance team function
• Organize and communicate information with
patients, families, and healthcare team members in a form that is
understandable, avoiding discipline-specific terminology when
possible
• Listen actively, and encourage ideas and
opinions of other team members while communicating consistently the
importance of teamwork in patient-centered and community-focused
care
Interprofessional team work and team-based practice
• Describe the process of team development and
the roles and practices of effective teams, while at the same time
engaging other health professionals - appropriate to the specific
care situation - in shared patient-centered problem-solving
• Apply leadership practices that support
collaborative practice and team effectiveness.
• Reflect on individual and team performance for
individual, as well as team, performance improvement with the use of
available evidence to inform effective teamwork and team-based
practices.
|
Roles and responsibilities for collaborative practice:
Learning and working as interprofessional requires understanding of the
role and duties of one as a member of the collaborative team, towards
team as well as to other professionals, towards patients and to
understand the roles and responsibilities of other members of the
interprofessional team. Nine competency statements for roles and
responsibilities for collaborative practice have been laid down (Box
3) [14].
Interprofessional communication practices:
Importance of effective communication lies in the way health
care professions communicate with patients, their attendants, other
members of health care team and authorities. Development of basic
communication skills is a common domain for health professions education
[18]. Moreover, effective interprofessional communication practices will
require the use of new communication technologies including informatics.
A committee of Institute of Medicine recommended that – ‘All
health professionals should be educated to deliver patient-centered care
as members of an interdisciplinary team, emphasizing evidence-based
practice, quality improvement approaches, and informatics’ [19].
Healthcare informatics not merely means information technology but
application of information technology systems to solve problems in
health care, research, and education, and the development of informatics
[20]. General competency statements for interprofessional communication
are summed-up in Box 3 [14].
Interprofessional teamwork and team-based practice:
Working in team is the motto of interprofessional education and
practice. Diverse competencies and cultural background of different
professionals working in a team can lead to multiple conflicts.
Resolving these conflicts and ability to continue to impart optimal
health care as a member of the interprofessional team is a competency to
be developed by an interprofessional health care provider. Open and
constructive approach to resolve these potential conflicts, team
leadership qualities and shared problem solving are some of the traits
that a good interprofessional health provider must imbibe. More detailed
general competency statements for interprofessional teamwork and
team-based practice are summed-up in Box 3 [14].
The list of interprofessional competencies is
considered comprehensive enough only when patient-centeredness and
collaborative leadership is considered along with these. Down syndrome
is one example of teaching-learning in an inter-professional scenario.
Table I depicts the errors in management and opportunities
provided by IPE and collaborative practice in managing this child with
Down syndrome.
|
Errors in management
|
Remedies as presented by
interprofessional education
|
|
Seemed as if the interests of the child were
put in the back-burner
No ethics were followed in the management of
the child’s condition
Child was never referred to pediatrician
before for confirmed diagnosis; No vaccination was provided to
the child; No cardiologist was consulted; in fact, child was
never referred to a specialist; Parents were never counseled
before, about providing care to the child; Services of
developmental pediatrician and psychologists were never asked
for.
There was total lack of cooperation among
different health care providers. No communication among required
health care providers was witnessed
|
Interests of the patient would have been at
the center in an IPE and collaborative practice set up
Ethical cooperation among other health
professionals - appropriate to the specific care situation would
have been possible
One professional would have been aware of his
competencies and limitations resulting in timely reference to
another specialist member of the team
Use of full scope of knowledge, skills, and
abilities of available health professionals would have been
possible resulting in better patient care
Communication among different members of team
would have been swift, enhancing team functioning
Overall, clinical outcomes would have been better
|
If one were to design an IPE curriculum for Down
syndrome, we would start by listing the learning objectives for Down
syndrome with respect to the level of the medical student viz
year 1,2 etc., followed by a written statement of the roles of teachers
of various specialties. For example, a geneticist, a pediatrician, a
pediatric surgeon, a pediatric cardiologist, a rehabilitation
specialist, etc. Each of the specialists must be part of a team that
collaboratively contributes to the inter-professional curriculum clearly
identifying the ‘must know’ and ‘nice to know’ areas for various level
of students. The curriculum should incorporate role-assignment, a
discussion on effective teaching learning strategies, and student
assessment. The inter-professional curriculum must necessarily include a
discussion on communication, ethics, and professionalism.
Teaching and Learning Approaches in IPE
Physician shadowing, team-based learning, and
community-based learning are some of the proposed strategies for
teaching learning in an IPE setting [6,21,22]. In shadowing, the student
learns by observing a physician in the real-life setting. Team-based
learning involves use of interactivity, roleplays, problem based
learning etc. which helps the learner learn the importance and attitudes
of being part of an interprofessional team [23-25]. Community-based
learning strategy, proposed in 1902, revolves around experiential
learning in the community [26]. Being situated in the real-life scenario
of the community, this strategy empowers the students to be better
adjusted in an interprofessional practice [27].
For the illustrative example in this article, Down
syndrome – students can experience observational learning in the
clinical setting of management of a child along with a physician and
surgeon and team based case discussion about how multidisciplinary care
of a child with Down syndrome can be organized and how the child should
be followed up with various specialists to not miss care of vital
issues, can be organized. Family study of how the family of a child with
Down syndrome copes with interprofessional referrals, their reactions
and attitudes to advices given, antenatal/genetic advice received,
access to rehabilitation services is an example of community based
learning strategy.
In addition, we need to acknowledge the role of
informal learning opportunities as an approach in IPE. It is an
unplanned offshoot of a planned interprofessional initiative. There are
instances when learners meet and discuss aspects of their formal
education allowing them to exchange ideas about their professions and
acquire direction from their peers and colleagues. Such informal
learning activities can be explicitly built into an interprofessional
program. For example, it can be used to provide opportunities during
breaks to informally discuss and share educational experiences. Studies
show that learners used bars and cafes to casually discuss and reflect
upon their interprofessional experience. These students have opined the
utility of this type of learning as valuable [28].
No single method is complete to deliver IPE.
Including learning experiences from different sources through varied
methods is also important to keep students interested and engaged.
Whichever methods are selected they should be experiential, interactive,
reflective and patient centered thus providing learning opportunities to
evaluate and compare roles, responsibilities, needs, ethics and
attitudes of practice, knowledge and skills of different professions
involved, leading to effective relationship building between the
professionals involved.
Assessment
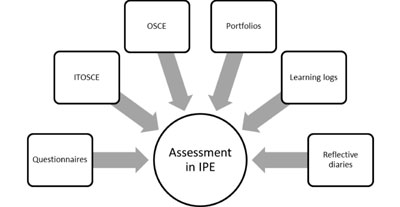
IPE is a new concept and measuring competencies for
IPE and collaborative practice is a complex phenomenon [29]. Moreover,
the tools to assess collaborative competencies are also limited [30].
Assessment of IPE may be formative or summative. Reflective diaries,
learning logs, portfolios and Objective structured clinical examinations
(OSCEs) are some of the prevalent assessment methods used [8].
Reflective diaries and portfolios will give opportunities for
self-assessment and learning. A modified form of OSCE -
interprofessional team objective structured clinical examination
(ITOSCE) has been described by Symonds, et al. [31]. Whatever
program of assessment is chosen, the criteria and credits should be
reliable, valid, and consistent across professions. Some common
assessment methods for assessing learning in IPE
(Fig. 2) are:
 |
|
Fig. 2 Assessment tools used
for assessing competencies for interprofessional education.
|
Reflective diaries: Reflective writing is by far
the most commonly used tool to assess IPE. It helps in self-assessment
as well as in learning too. It has been recommended that such reflective
writings should include – reflection before action, reflection in action
and reflection on action [32]. Reflective diaries help to assess if the
learners understand the roles, responsibilities and inter-personal
relationships in IPE. This tool has the inherent limitation that
learners may both underestimate or overestimate learning on
self-assessment. Reflective diaries are handy tools to assess knowledge,
skills, attitudes, and behaviors of learners for IPE and collaborative
practice.
Interprofessional team objective structured clinical
examination: As IPE involves team-work, it has been proposed that
team-assessment should be part of any assessment system for IPE.
However, the expectation that all will enter the team-environment with
same level of competency may hamper team-assessment. ITOSCE is a
formative assessment tool for assessing team-collaboration and
team-work. Learners, while working in team for ITOSCE, will move through
all five stages of Tuckman of group dynamics also and as such will take
time to learn and perform as a team. Though ITOSCE has been documented
to be logistically demanding, its educational impact is well established
[31].
Questionnaire: Standardized
questionnaires and checklists have been structured for assessing
attitudes and perceptions of learners about IPE, and can be good tools
for IPE program evaluation. Readiness for Interprofessional Learning
Scale (RIPLS) is the standardized tool most frequently used in IPE [33].
Other such questionnaire-based tools include - the Interdisciplinary
Education Perception Scale [34], the Interprofessional Attitudes
Questionnaire [35], and the Attitudes to Health Professionals
Questionnaire [36]. As stated, questionnaire-based tools can assess only
attitudes and perceptions of learners about IPE, and are not good
indicator of learning.
Assessment of learning based on IPE is an
interprofessional exercise too. It should be aligned with the learning
objectives for the area of concern. Various conventionally used tools of
assessment for different domains viz. application based multiple
choice questions, short answer questions, simulated patients, directly
observed procedural skills etc can be used to assess the
interprofessional learning.
Challenges in Adopting Interprofessional Education
Following are some of the challenges that
implementation of IPE faces in the current medical education scenario in
India.
Faculty development concerns: Content and tools
for training learning in IPE are different from usual health
professional education contents. So, faculty training and development in
IPE will be the first challenge in implementing IPE in health
institutes. Faculty needs to sensitize and train in various aspects of
IPE before taking-up the implementation part.
Development of curricula for IPE: Designing
common curricula for IPE for all professions involved, after considering
competency levels and expectations of all professions is next big
challenge. Curriculum development itself will involve collaboration of
different professional experts. Moreover, the curricula will vary from
institute to institute, from one encounter to other, depending upon the
type of professions involved and thus must be suitably amended and
adopted for every IPE team separately.
Logistic issues: Designing a common schedule and
adjust the timings to bring all learners together across many
professions will be logistically challenging. Similarly, it will be
problematic to bring all faculty/professionals required for teaching,
together at one common time. Moreover, all health profession institutes
may not have learners from different professions so as to make
collaborative-learning possible. This challenging situation can be
overcome by roping-in nearby located institutes imparting training in
other professions and with cooperation among administrative of these
institutes.
Assessment issues: Assessment in IPE is still in
its infancy, as stated above. There is urgent need to develop suitable
instruments to assess interprofessional-competencies so as to boost the
idea of competency-based interprofessional education.
Convincing learners: Convincing the learners –
the major stakeholders – for undergoing training in IPE will be a big
challenge. They need to be shown applicability and utilization of such
training. For this, collaborative practice in health care needs to be
made mandatory. Learners need to be ensured that there are enough
avenues for their placement after such training.
Lack of regulatory support: There are hardly any
regulations pertaining to IPE. Accreditation of IPE by accrediting
bodies across different professions is unheard-of. Bringing these
regulatory bodies on board and having common regulations across all
health professions involved in IPE is going to be the biggest challenge.
Policy decision at the national level can only change the perspectives.
In a nutshell, major barriers for IPE in the Indian
context are likely to be more systemic involving curricular and
accreditation issues. Handling of methodological barriers in terms of
faculty development, student diversity, communication issues and lack of
leadership can be challenging too. Behavioral barriers that relate to
stereotypes, mindset and resistance to change also need to be addressed.
Conclusion
The main utility of IPE is to produce
health-workforce ready to work in collaborative practice and thus
contributing to better health outcomes, thus improving both patients’
and health professionals’ satisfaction. Though being a relative
innovation, challenges are plenty, but with collaboration at different
levels and with right mind-set and approach these challenges can be
overcome easily. IPE is the next big thing, and for the better clinical
outcomes, for better health facilities and for better learners’ training
it should be adopted in the regular curricula urgently.
1. World Health Organization (WHO). Framework for
action on interprofessional education & collaborative practice. Geneva:
World Health Organization; 2010. Available from:
http://apps.who.int/iris/bitstream/10665/70185/1/
WHO_HRH_HPN_10.3_eng.pdf?ua=1. Accessed January 10, 2017.
2. CAIPE. 2002. What is CAIPE [homepage on internet].
Available from: https://www.caipe.org/. Accessed January 10,
2017.
3. Barr H. Interprofessional education: Today,
yesterday and tomorrow. Available from:
http://www.unmc.edu/bhecn/_documents/ipe-today-yesterday-tmmw-barr.pdf.
Accessed January 10, 2017.
4. Kohn LT, Corrigan JM, Donaldson MS. To Err is
Human: Building a Safer Health System. Washington, DC: National Academy
Press; 2000.
5. Reeves S, Fletcher S, Barr H, Birch I, Boet S,
Davies N, et al. A BEME systematic review of the effects of
interprofessional education: BEME Guide No. 39. Med Teach.
2016;38:656-68.
6. Nelson S, White CF, Hodges BD, Tassone M.
Interprofessional team training at the prelicensure level: a review of
the literature. Acad Med. 2017;92:709-16.
7. D’Amour D, Oandasan L. Interprofessionality as the
field of interprofessional practice and interprofessional education: an
emerging concept. J Interprof Care. 2005;19:8-20.
8. Barr H, Gray R, Helme M, Low H, Reeves S. In:
Interprofessional Education Guidelines 2016. London: Centre for
Advancement of Interprofessional Education; 2016. p. 5. Available from:
https://www.caipe.org/resources/publications/barr-h-grayr-helmem-low-h-reeves-2016-interprofessional-education-guidelines.
Accessed January 12, 2017.
9. Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N,
Evans T, et al. Health professionals for a new century:
Transforming education to strengthen health systems in an interdependent
world. Lancet. 2010;376:1923-58.
10. Baker DP, Gustafson S, Beaubien J. Medical
Teamwork and Patient Safety: The Evidence-Based Relation. Rockville, MD:
Agency for Healthcare Research and Quality; 2004. Available from:
https://archive.ahrq.gov/research/findings/final-reports/medteam/medteamwork.pdf.
Accessed January 10, 2017.
11. Nelson S, Turnbull J. Optimizing Scopes of
Practice: New Models for a New Health Care System: Report of the Expert
Panel Appointed by the Canadian Academy of Health Sciences. Ottawa,
Ontario, Canada: Canadian Academy of Health Sciences; 2014. Available
from:
http://www.cahs-acss.ca/wp-content/uploads/2014/08/Optimizing-Scopes-of-Practice_REPORT-English.pdf.
Accessed January 12, 2017.
12. Harden RM. The integration ladder: a tool for
curriculum planning and evaluation. Med Edu. 2000;34:551-7.
13. Jarvis P. In An International Dictionary of Adult
and Continuing Education. 2nd ed. London and New York: Routledge; 1990.
14. Interprofessional Education Collaborative Expert
Panel. Core competencies for interprofessional collaborative practice:
Report of an expert panel. Washington, DC.: Interprofessional Education
Collaborative; 2011. Available from:
https://www.aamc.org/download/186750/data/core_competencies.pdf.
Accessed January 10, 2017.
15. Barr H. Competent to collaborate: Towards a
competency-based model for interprofessional education. J Interprof
Care. 1998;12:181-7.
16. Interprofessional Professionalism Collaborative.
Definition of Interprofessional Professionalism. Available from:
http://www.interprofessionalprofessionalism.org/index.html. Accessed
January 10, 2017.
17. Berwick D, Davidoff, F, Hiatt H, Smith R.
Refining and implementing the Tavistock principles for everybody in
health care. BMJ. 2001;323:616-20.
18. Association of American Medical Colleges. Report
III: Contemporary issues in medicine - Communication in medicine.
Medical School Objectives Project. Washington, DC; 1999. Available from:
https://members.aamc.org/eweb/upload/Contemporary%20Issues%20In%20Med%
20Commun%20in%20Medicine%20Report%20III%20. pdf. Accessed January
10, 2017.
19. Institute of Medicine. Crossing the Quality
Chasm: A New Health System for the 21st Century. Washington, DC:
National Academy Press; 2001. Available from:
https://www.nap.edu/html/quality_chasm/reportbrief.pdf. Accessed
January 12, 2017.
20. Masys DR, Brennan PF, Ozbolt JG, Corn M,
Shortliffe EH. Are medical informatics and nursing informatics distinct
disciplines? The 1999 ACMI debate. J Am Med Information
Assoc. 2000;7:304-12.
21. Kusnoor AV, Stelljes LA. Interprofessional
learning through shadowing: Insights and lessons learned. Med
Teach. 2016;38:1278-84.
22. Hosny S, Kamel MH, El-Wazir Y, Gilbert J.
Integrating interprofessional education in community-based learning
activities: case study. Med Teach. 2013;Suppl 1:S68-73.
23. Kesten KS. Role-play using SBAR technique to
improve observed communication skills in senior nursing students. J Nurs
Educ. 2011;50:79-87.
24. Aebersold M, Tschannen D, Sculli G. Improving
nursing students’ communication skills using crew resource management
strategies. J Nurs Educ. 2013;52:125-30.
25. Garbee DD, Paige JT, Bonanno LS, Rusnak VV,
Barrier KM, Kozmenko LS, et al. Effectiveness of teamwork and
communication education using an interprofessional high-fidelity human
patient simulation critical care code. J Nurs Educ Pract. 2013;3:1-12.
26. Progressive education. Wikipedia. Available from:
https://en.wikipedia.org/wiki/Progressive_ education. Accessed
January 7, 2017.
27. Shumer R. Community-based learning: humanizing
education. J Adolescence. 1994;17:357-67.
28. Reeves S. Community-based interprofessional
education for medical, nursing and dental students. Health Soc Care
Commun. 2000;8:269-76.
29. Centre for the Advancement of Interprofessional
Education (CAIPE). Principles of Interprofessional Education. London,
United Kingdom: CAIPE: 2001.
30. Morison S, Stewart M. Developing
interprofessional assessment. Learn Health Social Care. 2005;4:192-202.
31. Symonds I, Cullen L, Fraser D. Evaluation of a
formative interprofessional team objective structured clinical
examination (ITOSCE): A method of shared learning in maternity
education. Med Teach. 2003;25:38-41.
32. Simmons B, Wagner S. Assessment of continuing
interprofessional education: Lessons learned. J Contin Educ Health Prof.
2009;29:168-71.
33. Parsell G, Bligh J. The development of a
questionnaire to assess the readiness for health care students for
interprofessional learning (RIPLS). Med Educ. 1999;33:95-100.
34. Slack MK, Coyle RA, Draugalis JR. An evaluation
of instruments used to assess the impact of interdisciplinary training.
Issues in Interdisciplinary Care. 2001;3:59-67.
35. Carpenter J. Doctors and nurses: Stereotypes and
stereotype change in interprofessional education. J Interprof Care.
1995;9:151-61.
36. Lindqvist S, Duncan A, Shepstone L, Watts F, Pearce S.
Development of the ‘Attitudes to Health Professionals Questionnaire’
(AHPQ): A measure to assess inter-professional attitudes. J Interprof
Care. 2005;19:269-79.

