|
|
|
Indian Pediatr 2017;54: 208-210 |
 |
Bedside Infant Manikins
for Teaching Newborn Examination to Medical Undergraduates
|
|
*Sheila Samanta Mathai, Deepak Joshi and Mrigank
Choubey
From The Department of Pediatrics, Armed Forces
Medical College, Wanowrie PO, Pune, Maharashtra, India.
Correspondence to: Dr Sheila Samanta Mathai,
Professor and Head of Department, Department of Pediatrics, Armed Forces
Medical College, Pune 411 040, India.
Email: [email protected]
Received: February 28, 2016;
Initial review: May 19, 2016;
Accepted: October 08, 2016.
Published online: November 05, 2016.
PII:S097475591600021
|
Objective: To study whether
using infant manikins during clinical posting could help in teaching
newborn examination to undergraduate medical students. Methods:
111 final MBBS students were taught newborn examination either by the
new method which included practice on infant manikins at the bedside
before examining babies (Group 1) or by the traditional method which
involved directly examining babies (Group 2). They were tested the next
day by validated OSCE stations on important aspects of the newborn
examination. Marking was done as 0 (completely incorrect), 1 (partially
correct) or 2 (completely correct). Student feedback was also taken.
Results: Scores were higher, with lesser variance, in Group
1. Student feedback was positive, favoring the new method. Conclusion:
Use of infant manikins at the bedside during clinical posting improves
the performance of undergraduate students in newborn examination.
Keywords: Competency-based medical education,
Simulation, Skill-teaching.
|
|
T
eaching large numbers of undergraduates how to
examine newborn babies in the limited time available is a challenging,
though mandatory, requirement of the undergraduate syllabus. However,
many fresh medical graduates remain diffident in actually examining
patients, specially newborns [2]. Traditional bedside demonstration of
the newborn examination by a faculty followed by supervision of students
while they examine babies themselves is tedious, and it is not always
possible to ensure that every student actually achieves the requisite
skills. We attempted to improve the traditional teaching method of
newborn examination by using an infant manikin. This study was
undertaken to determine if the use of manikin during clinics could
improve the teaching of newborn examination to undergraduate medical
students.
Methods
This was a prospective, observational study conducted
with final year MBBS students during their Pediatric rotation. After
taking the Institutional Ethics Committee clearance and informed consent
of the students, batches of students were designated as Group 1 or Test
Group (these students were exposed to the new method of teaching) and
Group 2 or Control Group (these students were subjected to the
traditional method of teaching) by draw of lots.
From a pilot study, it was calculated that a sample
size of 90 would be required to detect a 30% improvement in OSCE scores
in newborn examination in the Test group with an alpha error of 5% and
power of 80%. A convenience sample of 111 was taken to include all
medical students coming for their Pediatric posting in the final year.
53 students were assigned to the test group (2 batches) and 58 students
to the control group (2 batches) by draw of lots.
Group 1 was taught the newborn examination by the new
method wherein a faculty member first demonstrated signs on the baby
following which every student practiced on an infant manikin at the
bedside under supervision (with correction if necessary) before
examining babies themselves, in small groups, under supervision. Group 2
was taught by the traditional method wherein students observed faculty
demonstrating signs on the baby and they then performed the examination
on babies themselves, in groups, under supervision. Time allotted for
the teaching sessions was similar for both groups. Neonatal
resuscitation manikins (ResusciAnne by Laedral) were used for the study.
Students were tested by validated OSCE stations the
day after the teaching session. Assessment was done on important aspects
of the newborn examination requiring some maneuverability of the baby.
Station A consisted of aspects of the general examination (Feeling the
anterior fontanel, looking for jaundice on palms and soles, checking for
ear recoil, breast nodule and sole creases) and Station B consisted of
some aspects of the neurological examination (assessing muscle tone by
scarf sign, arm recoil, heel to ear and popliteal angle and eliciting
the neonatal reflexes namely palmar and plantar grasp reflexes and
Moro’s reflex). Adequate numbers of healthy neonates were available at
each OSCE station to ensure that no baby was examined by more than four
students, to avoid fatigue of the neonates. Consent of the mothers was
taken for the examination of the neonates. Complete asepsis and other
relevant precautions were observed during the conduct of the OSCE.
Marking was done by trained faculty on a nominal scale of 0 (completely
incorrect), 1 (partially correct) or 2 (completely correct). What
constituted 0, 1 and 2 was pre-determined and the scoring guide or
checklist was kept with the trained examiner during the session. Each
station was for 5 minutes. No student could see how others were
doing during the examination as the stations were in adjacent but
different rooms.
Scores were compared between groups using Moods
Median Test and variability in scores was compared by Levene Test. After
the study was over, students (Test group) were asked to give a feedback
on a Likert-scale on a validated questionnaire. After the end of the
study, Control group students were also given an opportunity to practice
on the infant manikins before the final examination.
Results
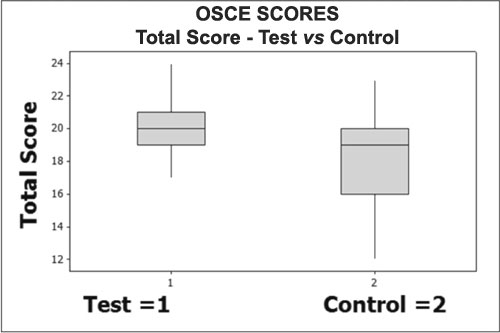
OSCE scores were statistically better in Group 1
(Test) as compared to Group 2 (Control), both in the general examination
and neurological examination stations. In addition, the variance in the
scores was significantly less in Group 1 (Fig. 1). In the
student feedback, majority felt that practice on the manikin had helped
them in performing specific aspects of the newborn examination at the
OSCE stations (Table I).
 |
|
Fig. 1 Box-plot chart showing
difference in OSCE scores between group taught with a manikin
(Test group) versus group taught by traditional method (Control
Group).
|
TABLE I Feedback of Medical Undergraduates Regarding Practice in a Manikin (N=53)
|
Helped me in |
Agree (%) |
Not sure (%) |
Disagree (%) |
|
examining for |
|
|
|
|
Ear recoil |
63 |
6 |
31 |
|
Breast nodule |
67 |
8 |
25 |
|
Plantar creases |
65 |
3 |
32 |
|
Palmar reflex |
58 |
10 |
32 |
|
Plantar reflex |
62 |
5 |
30 |
|
Moro’s reflex |
54 |
5 |
26 |
|
Tone of the baby |
71 |
5 |
24 |
|
Anterior fontanel |
60 |
18 |
22 |
|
Jaundice |
67 |
11 |
22 |
|
Overall |
63 |
10 |
27 |
Discussion
This observational study looked at using a simple
manikin to improve the skills of undergraduate medical students in
examining newborns. In our study the students showed significantly
better OSCE scores when manikins were used during teaching, in addition
to the majority agreeing to the benefit of the training.
The main limitation of our study was that only one
assessment was done, and that too the day after the training session.
Hence the long-term effects of this change in training methodology
cannot be commented upon. Moreover, we did not look at the mother’s
response to this method of teaching. Medical educators realize how
anxious mothers get when young medical students handle their babies and
this method of teaching could actually alleviate this anxiety.
Although there is ample evidence that simulation in
training in critical care procedures is effective [5], its use for
teaching clinical skills in neonatology has been infrequently addressed.
Nurses and paramedics still use simple, non-computerized task-trainer
manikins for teaching nursing procedures and breast feeding [6]. Bath,
et al. [7] made an attempt to improve baby ‘handling skills’ of
medical students with mechanized dolls. Most students felt that it
helped them understand better the caretaking issues related to real
babies.
There is a felt need to embrace simulation in
pediatric teaching [8]. ‘Skills laboratory’ is now a mandatory
requirement in medical colleges as per the latest MCI guidelines [9]. We
feel that this study will add to the body of evidence on the use of
manikins in undergraduate medical education, especially at the bedside
for on examination skill.
Our study suggests that the using infant manikins at
the bedside can improve skills of undergraduates in examining newborn
babies. This method may be adopted in medical colleges during pediatric
clinical postings.
Acknowledgements: GSMC Faimer Regional Centre
Mumbai for support during planning as the project was part of the first
author’s FAIMER project and Mr Ranjan Samanta, BSc (Statistics) for
statistical advice and analysis.
Contributors: SSM: conceived the study,
supervised and participated in training, conducted the OSCE and wrote
the paper; DJ: helped in training and conduct of the OSCE and also in
editing the draft of the paper; MC: helped in conduct of the OSCE and
the questionnaire, and in editing the paper. All authors approved the
final manuscript.
Funding: None; Competing interests: None
stated.
|
What This Study Adds?
• Additional practice on manikin at the
bedside during clinical posting improves students’ performance
in examination of the newborn.
|
References
1. Srivastava RN, Mittal SK, Paul VK, Ramji S; for
Indian Academy of Pediatrics. IAP Guidelines for Graduate Medical
Education in Pediatrics. Indian Pediatr. 2001;38:605-18.
2. Supe A, Burdick WP. Challenges and issues in
medical education in India. Acad Med. 2006;81:1076-80.
3. Okuda Y, Bryson EO, Demaria S, Jacobson L,
Quinines J, Shen B, et al. The utility of simulation in medical
education: what is the evidence? Mt Sinai J Med. 2009; 76:330-43.
4. Halamek LP, Kaegi DM, Gaba DM, Sowb YA, Smith
BC, Smith BE, et al. Time for a new paradigm in pediatric medical
education: teaching neonatal resuscitation in a simulated delivery room
environment. Pediatrics. 2000;106:E45.
5. Weinberg ER, Auerbach MA, Shah NB. The use of
simulation in pediatric training and assessment. Curr Opin Pediatr.
2009;21:282-7.
6. Aebersold M, Tschannen D. Simulation in nursing
practice: the impact on patient care. Online J Issues Nurs.
2013;31;18:6.
7. Bath LE, Cunningham S, McIntosh N. Medical
students’ attitudes to caring for a young infant-can parenting a doll
influence these beliefs? Arch Dis Child. 2000; 83:521-3.
8. Kalaniti K, Compbell DM. Simulation-based medical
education – time for a pedagogical shift. Indian Pediatr. 2015;52:41-5.
9. Minimum Standard Requirements for Medical Colleges. Available
from: http:// www.mciindia.org. Accessed June 15, 2016.
|
|
|
 |
|

