|
|
|
Indian Pediatr 2016;53: 263 |
 |
Pulsus Paradoxus in a Neonate with Interrupted
Aortic Arch
|
|
*Shiv Sajan Saini and Vinay Vamdev Kulkarni
Neonatal Unit, Department of Pediatrics, Post Graduate
Institute of Medical Education and Research, Chandigarh, India. Email:
[email protected]
|
|
Pulsus paradoxus is an exaggerated inspiratory fall (>10 mmHg) of
systolic blood pressure (BP). It has been reported with cardiac
tamponade, asthma, pericarditis, croup, hemorrhagic shock and
cardiomyopathy [1-3]. We report a novel association with interrupted
aortic arch [left ventricular outflow tract (LVOT) obstruction].
A full-term, 2.8 kg, 8-day-old male neonate presented
with congestive cardiac failure and shock (heart rate- 152/min,
respiratory rate 80/min, cold/pale extremities, right upper limb BP
31/12 mmHg, chest retractions, and hepatomegaly). His femoral pulses
were feeble and were disappearing during inspiration. His right brachial
pulse was constant throughout respiratory cycle. His lower limb BP was
unrecordable. The respiratory variation in pulses was also appreciated
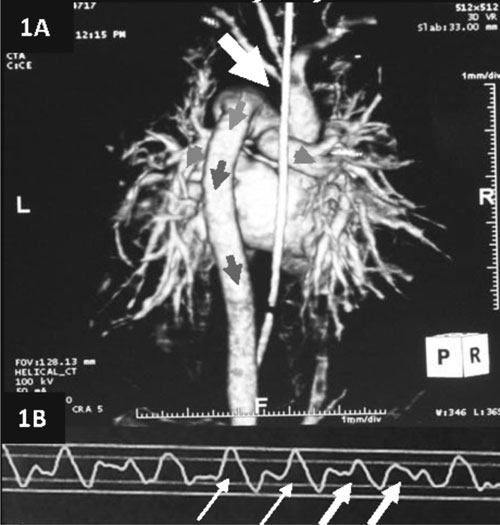
on pulseoximetry (Fig. 1a). His cardiac examination was
unremarkable except increased precordial activity. Echocardiography and
computed tomography angiography (Fig. 1b) confirmed
interrupted aortic arch. With Prostaglandin E 1
(PGE1) infusion and
supportive care, his lower limb pulses and BP improved [45/28 mmHg (mean
34)]. The respiratory variation in pulseoximetry gradually disappeared.
Disappearance of pulses during inspiration and respiratory variation in
pulse waveforms was consistent with pulsus paradoxus [4,5].
 |
|
Fig. 1 (a) Pulse oximetry tracing
showing normal amplitude pulse waveform during expiration (thin
arrows), and low amplitude pulse wave form during inspiration
(thick arrows); (b) Computed tomography angiography image
showing interrupted aortic arch (arrow).
|
The possible explanation of pulsus paradoxus in our
neonate is as follows. Blood flow in descending aorta is compromised in
LVOT obstruction. With onset of PDA closure, congestive cardiac failure
develops and hence aortic blood flow gets further compromised. Such
neonates develop respiratory distress and thus generate ‘strong
negative’ intrathoracic pressure. As a result, LV diastolic filling is
compromised and right ventricular (RV) filling is relatively increased.
This differential ventricular filling results in increased RV end
diastolic volume, which augments LV transmural pressure (LV wall stress)
and further decreases LV diastolic filling [4]. Due to these reasons,
aortic blood flow can decrease markedly during inspiration leading to
manifestation of pulsus paradoxus. Additionally, blood is likely to
shunt from left to right ventricle across VSD, which could have also
contributed to development of pulsus paradoxus. Pulsus paradoxus in LVOT
obstruction is likely to manifest in post-ductal circulation during
impending PDA closure. Our hypothesis is strengthened by disappearance
of pulsus paradoxus after PGE1
infusion. We postulate that pulsus paradoxus in
postductal circulation can detect impending ductal closure, in LVOT
obstruction. Whereas, differential pulses suggest LVOT obstruction,
pulsus paradoxus in such setting might indicate impending ductal closure
and is thus an ominous sign. This case underscores the importance of
thorough clinical examination of pulses and pulse waveforms in any
neonate with suspected LVOT obstruction.
References
1. O’Gara PT, Loscalzo J. Physical Examination of the
Cardiovascular System. In: Fauci AS, Braunwald E, Kasper DL,
Hauser SL, Longo DL, Jameson JL, et al., eds. Harrison’s
principles of internal medicine. 18th ed. New York: McGraw Hill; 2012.
p.1821-30.
2. Frey B, Freezer N. Diagnostic Value and
pathophysiologic basis of pulsus paradoxus in infants and children with
respiratory disease. Pediatr Pulmonol. 2001;31:138-43.
3. Khasnis A, Lokhandwala Y. Clinical signs in
medicine: Pulsus paradoxus. J Postgrad Med. 2002;48:46-9.
4. Amoozgar H, Ghodsi H, Borzoee M, Amirghofran AA,
Ajami G, Serati Z. Detection of pulsus paradoxus by pulse oximetry in
pediatric patients after cardiac surgery. Pediatr Cardiol. 2009;30:41-5.
5. McGregor M. Current concepts: Pulsus paradoxus. N Engl J Med.
1979;301:480-2.
|
|
|
 |
|

