|
|
|
Indian Pediatr 2016;53:
253-255 |
 |
Gastrointestinal Fistulization in Amebic
Liver Abscess
|
|
KP Srikanth, BR Thapa and Sadhna B Lal
From Division of Pediatric Gastroenterology,
Department of Gastroenterology, PGIMER, Chandigarh, India.
Correspondence to: Dr KP Srikant, Senior Resident,
Division of Pediatric Gastroenterology, Department of
Gastroenterology, PGIMER, Chandigarh, India.
Email: [email protected]
Received: August 05, 2015;
Initial review: October 20, 2015;
Accepted: November 28, 2015.
|
Background: Liver abscess is a common deep seated
abscess in children; amebic liver abscess is associated with more local
complications. Case characteristics: We report two preschool
children presenting with short history of pain, fever and right upper
quadrant pain. The abscess communicated with gastro-intestinal tract
(ascending colon in case 1 and duodenum in case 2), and diagnosis of
amebic liver abscess was confirmed by DNA PCR. Outcome: Both
children were successfully managed with intravenous antibiotics and
catheter drainage. Message: Gastrointestinal fistulization may be
rarely seen in amebic liver abscess. Conservative management with
antibiotics, catheter drainage and supportive care may suffice.
Keywords: Complication, E.histolytica, Hepatic abscess.
|
|
Pyogenic liver abscess accounts for nearly 80% of
all liver abscesses in children; amebic etiology may be frequently
encountered in children from tropical developing nations [1,2]. Amebic
liver abscess is uncommon in children, but it poses higher risk of local
complications, and often proves to be a challenge in management. We
report two preschool children with fistulizing amebic liver abscess, who
were managed conservatively.
Case Reports
Case 1: A 3-year-old girl, presented
with intermittent high grade fever with chills for 2 days, which
subsided with antipyretics. Subsequently she developed periumbical pain,
which shifted to right upper abdomen. There was no abdominal distension,
vomiting or diarrhea. A transabdominal sonography (USG) on day 7 of
illness revealed an abscess in right lobe (Segment V), after which she
was referred to our center for management. On admission, child was
hemodynamically stable, and had mild pallor. Abdominal examination
revealed tender hepatomegaly. There was no free fluid or any sign of
peritonitis. Systemic examination was normal. Repeat USG revealed
abscess in the right lobe of the liver measuring 3.5 × 2.8 cm with
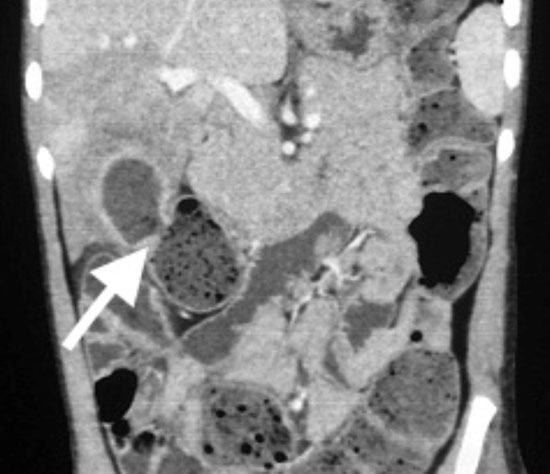
probable communication with ascending colon. Contrast enhanced computed
tomography (CECT) of abdomen showed air fluid level in the abscess and
communication with colon (Fig. 1). Blood investigations
revealed anemia (Hb 8.1 g/dL), thromobocytosis (Platelet count
650,000/µL), microcytic hypochromic anemia and hypoalbuminemia (serum
albumin 2.7 g/dL). Qualitative amebic serology (RIDASCREEN, Germany) was
positive. Bacterial culture from blood and aspirates were sterile.
Aspirate from abscess revealed a positive result for amebic DNA by
polymerase chain reaction (PCR). Child was treated with metronidazole
for 14 days. USG done after 7 days revealed decrease in size of the
abscess with disappearance of air fluid level. Child clinically improved
and was discharged from the hospital after 10 days of stay. After 3
months, USG showed complete disappearance of cavity and the
communication.
 |
|
Fig.1 Coronal CECT abdomen showing
abscess communicating with the ascending colon.
|
Case 2: A 2-year-old girl, presented with
high grade intermittent fever for 7 days, watery diarrhea for initial
four days, along with pain and fullness in the right upper abdomen.
Child was evaluated at another hospital, where she was diagnosed to have
abscess in the segment VI and VII of the liver (Fig. 2a),
that was communicating with second part of the duodenum. At admission to
our center, she was hemodynamically stable, and had severe wasting
(weight for length <-3 SD) and mild pallor. Abdominal examination
revealed mild hepatomegaly; there were no local signs. She received
intravenous ceftriaxone, cloxacillin and metronidazole. Pigtail catheter
was inserted under USG guidance. The pus culture revealed growth of
E.coli, sensitive to amikacin and imipenem, and antibiotics were
changed as per the sensitivity. Aspirate was also positive for amebic
DNA PCR. Blood investigations revealed microscopic hypochromic anemia (Hb
7.4 g/dL), thromobocytosis (platelet counts 744,000/µL), and
hypoalbuminemia (S. albumin 2.2 g/dL). Amebic serology was also
positive. After initial stabilization, she was started on liquid diet,
but most of the feed drained through the inserted catheter. Duodenoscopy
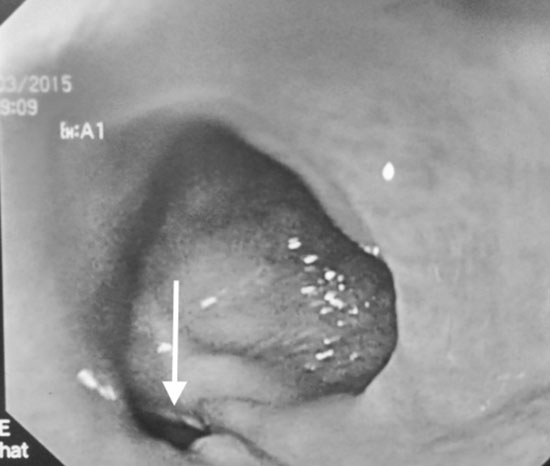
showed an opening at junction of first and second part of the duodenum (Fig.
2b). For next 48 hours, she was managed on intravenous fluids. Oral
feeds were started gradually, and patient tolerated well, probably due
to spontaneous closure of fistulous tract. She was discharged after
one-week stay. Intravenous antibiotics were continued for 2 weeks,
followed by oral antibiotics for a total of 4 weeks.
 |
| (a) |
(b) |
|
Fig. 2 Coronal CECT abdomen showing
large abscess communicating with second part of duodenum (a);
Duodenoscopy showing opening at the junction of the D1 and D2
(b).
|
Stool microscopy was normal. The acquired and
preliminary primary immune deficiency work up like Nitroblue tetrozolum
test, immunoglobulin levels and flow cytometry for T and B cell
fractions were within normal reference range in both the patients.
Discussion
In liver abscess caused by Entamoeba histiolytica,
various virulence factors like cystinease, amebapore and Gal/GalNAc
lectin binding protein cause tissue invasion and lead to local
perforating complications [1]. Clinical distinction between amebic and
pyogenic liver abscess is at times challenging and warrants empirical
dual therapy. Amebic serology is nearly 95% sensitive and specific, but
in areas of high prevalence false positivity is a problem. DNA PCR from
the aspirate is nearly 100% sensitive and specific, but lacks widespread
availability [3]. Antigen detection from abscess aspirates hold similar
sensitivity and specificity. Size larger than 50 mm, location in left
lobe, liver failure or severe sepsis, warrants immediate drainage;
continuous catheter drainage is better than single time aspiration [4].
Metronidazole for 10 days is optimum for treatment of amebic liver
abscess [2]. Amebic liver abscess is more likely to be associated with
local complications like bronchopleural, pericardial, peritoneal and
even subcutaneous fistulizations [5]. Hepatico-gastrointestinal lumen
perforations are very rare in children; only a few cases are reported
[6]. Various treatment modalities are suggested, including major
surgeries [7]. Ideal approach would be to individualize the therapeutic
options depending upon the physiological status of the patient and
expertise of treating center.
To summarize, amebic liver abscess causing
gastrointestinal fistulization is rare in children posing diagnostic and
therapeutic challenges. Careful clinical and radiological monitoring,
and conservative management can be effective.
Contributors: SKP: prepared the manuscript and
helped in managing the cases; TBR and SBL: managed the cases and
finalized the manuscript.
Funding: None;
Competing interest: None stated.
References
1. Mishra K, Basu S, Roychoudhury S, Kumar P. Liver
abscess in children: an overview. World J Pediatr. 2010;6:210-6.
2. Haque R, Huston CD, Hughes M, Houpt E, Petri WA,
Jr. Amebiasis. N Engl J Med. 2003;348:1565-73.
3. Tanyuksel M, Petri WA, Jr. Laboratory diagnosis of
amebiasis. Clin Microbiol Rev. 2003;16:713-29.
4. Singh S, Chaudhary P, Saxena N, Khandelwal S,
Poddar DD, Biswal UC. Treatment of liver abscess: Prospective randomized
comparison of catheter drainage and needle aspiration. Ann Gastroenterol.
2013;26:332-9.
5. Meng XY, Wu JX. Perforated amoebic liver abscess:
Clinical analysis of 110 cases. South Med J. 1994;87: 985-90.
6. Angel C, Chand N, Sankar A, Rowen J, Murillo C.
Gastric wall erosion by an amoebic liver abscess in a 3-year-old girl.
Pediatr Surg Int. 2000;16:429-30.
7. Singh M, Kumar L, Kumar L, Prashanth U, Gupta A, Rao ASN.
Hepatogastric fistula following amoebic liver abscess: An extremely rare
and difficult situation. OA Case Reports. 2013;2:38.
|
|
|
 |
|

