|
|
|
Indian Pediatr 2015;52: 220 -222 |
 |
Serum IgG and IgA Levels in Polio and
Non-polio Acute Flaccid Paralysis Cases in
Western Uttar Pradesh, India
|
|
Madhu C Mohanty, Uma P Nalavade and Jagadish M
Deshpande
From Enterovirus Research Center, Indian Council of
Medical Research, Haffkine Institute Campus, Acharya Donde Marg, Parel,
Mumbai, India.
Correspondence to: Dr Jagadish Mohanrao Deshpande,
Director, Enterovirus Reseach Center, Indian Council of Medical
Research, Haffkine Institute Campus, Acharya Donde Marg, Parel, Mumbai
400 012, India.
Email: deshpandejm@gmail.com
Received: May 30, 2014;
Initial review: August 04, 2014;
Accepted: December 20, 2014.
|
Objective: IgG and IgA immunocompetence of
children with wild poliovirus poliomyelitis and non-polio acute flaccid
paralysis.
Methods: 932 cases of acute flaccid
paralysis, reported in 2008-2009, were tested for presence of polio and
non-polio enteroviruses according to the WHO standards. Serum IgA and
IgG levels were determined by sandwich ELISA.
Results: Mean (SD) IgA levels [0.87 (0.62)g/L;
n=28] of virologically confirmed poliomyelitis cases were lower than
those of virus negative [1.21 (0.83)g/L; n=612] and non-polio
Enterovirus positive [1.22 (0.79)g/L; n=240] cases of acute
flaccid paralysis. No significant difference was observed in the
concentration of IgG among these groups.
Conclusion: IgA plays an important role in
protection against poliomyelitis.
Keywords: Acute flaccid paralysis, Poliovirus, Poliomyelitis,
Serum immunoglobulins
|
|
Since 2007, polio antibody sero-prevalence studies
were undertaken in Bihar and Uttar Pradesh, to understand why polio
eradication faced challenges in these two states. A sero-survey of acute
flaccid paralysis (AFP) cases for polio antibody prevalence in 25
districts in Western Uttar Pradesh was conducted in 2008-09. We reported
that there was no abnormal prevalence of immunodeficiency in children in
Western Uttar Pradesh that could have delayed achieving zero-polio [1].
Success of polio eradication initiative depends on
breaking all chains of wild poliovirus transmission. Neutralization of
virus infectivity by the serum antibody, mostly IgG, is the main
modality of protection against invasion of poliovirus into the central
nervous system, whereas IgA antibody is the most important defense at
the mucosal surfaces of the nasopharynx and gastrointestinal tract [2].
Recent studies provide evidence that poliovirus specific IgA intestinal
antibody is a determinant of virus excretion and that IgA functions
through neutralization of the virus infectivity [3]. Circulating
phagocytes may also play a role in the defense against poliovirus,
mediated through serum IgA [4]. We compared serum IgG and IgA levels of
children with paralytic poliomyelitis and non-polio AFP with the
objective to explore any correlation of these immunoglobulins with the
susceptibility to paralytic poliomyelitis.
Methods
Stool samples of AFP cases were collected as per the
AFP surveillance guidelines [5]. Venous blood samples (1 to 2 mL) were
collected from AFP cases up to 5 years of age at the time of clinical
examination by the surveillance medical officers of the National Polio
Surveillance Unit (NPSU). Polio and non-polio Enterovirus (NPEV)
isolation and identification were carried out as per the standard WHO
protocol for virological investigations of AFP cases [6]. IgG and IgA
concentrations of the serum samples were estimated by sandwich ELISA, as
described earlier [1].
Student’s t test was used for comparing the mean
immunoglobulin values between different groups of AFP children. Sigma
Plot was used for statistical analysis.
Results
Stool and serum samples of 932 AFP cases reported in
25 districts in Western Uttar Pradesh in 2008-2009 were investigated.
Wild poliovirus (WPV) was isolated from stools of 28 (3.0%) cases of
which 11 were WPV1 and 17 were WPV3. Sabin OPV strains were isolated
from 46 (5%) cases and NPEV from 240 (25.7%) cases. No enterovirus was
detected in stools of 618 (66.2%) cases. AFP cases were thus divided
into four groups (WPV, NPEV, Sabin PV, EV negative) on the basis of
virological test results. Median (range) age of the AFP cases were 12 (1
to 46), 18 (0 to 60), 23 (0 to 58) and 20 (0 to 59) months in WPV, NPEV,
Sabin PV and EV negative groups, respectively.
Mean (SD) serum immunoglobulin concentrations of the
932 AFP cases were IgG 9.62 (3.47) g/L and IgA 1.2 (0.82) g/L. There
were 5 AFP cases with IgG level less than 2 g/L and four AFP cases with
IgA level below 0.07 g/L, all in the virus negative group.
TABLE I Mean (SD) IgG and IgA Concentration According to Results of Virus
Isolation From Stool Sample of AFP Cases
|
Virus Isolation |
No. |
IgG (g/L) |
IgA (g/L) |
|
WPV |
28 |
8.71 (3.66) |
0.87 (0.62) |
|
Sabin PV |
46 |
9.51 (4.14) |
1.19 (0.88) |
|
NPEV |
240 |
9.70 (3.45) |
*1.22 (0.79) |
|
EV Negative |
618 |
9.65 (3.42) |
*1.21 (0.83) |
|
P <0.05 for comparison with WPV. |
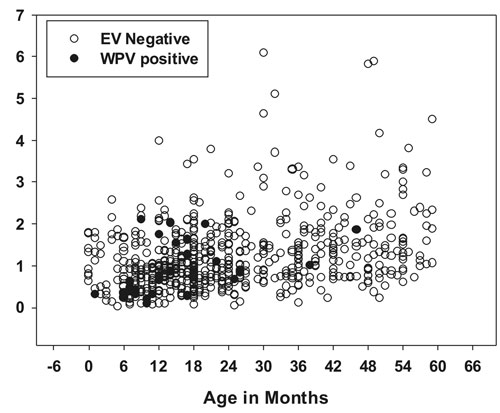
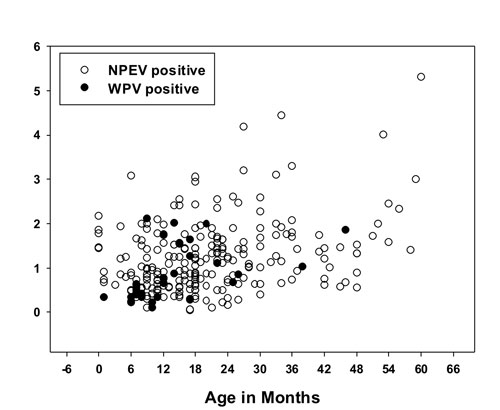
Comparison of serum IgG and IgA levels in the four
groups of AFP cases is presented in the Table 1. Serum IgG
concentrations were not significantly different between any of the four
groups. However serum IgA levels of wild poliovirus cases were
significantly lower than the IgA levels in AFP cases with either NPEV
(n=240, P<0.025) or no enterovirus in the stools (n=618,
P<0.03). (Fig. 1).
(a) |
| |
(b) |
|
Fig. 1 Scatter Plots of serum IgA
levels in (a) WPV vs. EV negative cases; (b) WPV vs. NPEV
cases, plotted against the age at onset of paralysis.
|
We also compared the IgA levels by stratifying the
data using 6-month intervals. IgA levels of WPV cases up to the age of
12 month were significantly lower than NPEV and virus negative AFP cases
(Table II). The values could not be confidently evaluated
for the higher age groups because of the small number of WPV cases.
TABLE II Age-stratified Serum IgA Levels of EV Negative, NPEV and WPV AFP Cases
|
Age (mo) |
Serum IgA Levels, Mean ± SD (n), g/L |
|
EV Negative |
NPEV |
WPV |
|
0-6 |
1.04+ 0.61 (46) |
1.14+ 0.7(21) |
0.30+ 0.050 (3) |
|
7-12 |
0.86 +0.62 (96) |
0.92+ 0.53 (52) |
0.65±0.61 (13) |
|
13-18 |
1.02 +0.60 (49) |
1.05 + 0.67 (61) |
1.20+ 0.61 (6) |
|
19-24 |
1.14 + 0.64 (87) |
1.18+ 0.59 (39) |
1.54+ 0.63 (2) |
|
25-30 |
1.39 + 1.08 (52) |
1.51 +0.92 (26) |
0.77+ 0.12 (2) |
|
31-36 |
1.41 + 1.00 (50) |
1.91+ 1.01 (15) |
Nil |
|
37-42 |
1.53 + 0.71(45) |
1.18 +0.38 (8) |
1.02 (1) |
|
43-48 |
1.48 + 1.04 (32) |
1.03+ 0.38 (9) |
1.86(1) |
|
49-54 |
1.70 + 1.09 (44) |
2.34 +0.98 (5) |
|
|
55-60 |
1.98+ 1.056 (17) |
3.01 +1.66 (4) |
|
Discussion
Humoral antibodies of IgG type play important role in
protection against paralytic disease whereas the IgA antibodies
(especially secretory IgA) may be critical to stop poliovirus infection
and replication at the primary sites [7]. We compared the immunoglobulin
levels in AFP children grouped on the basis of virological results, and
found that patients with WPV paralysis had significantly lower IgA
levels than NPEV positive and enterovirus negative cases.
There were a few limitations in our study. We
quantified total serum IgA because poliovirus-specific IgA antibody
assays were not readily available. As the study was done in the late
stage of polio eradication initiative, the number of WPV cases were
fewer than before.
Our observation that lower levels of serum IgA in AFP
classified as WPV poliomyelitis than non-polio AFP suggests that
poliovirus replication/excretion is dependent mainly on IgA response.
Contributors: JMD: conceived the study, helped in
designing the study, revised and approved the manuscript for important
intellectual content; MCM: designed the study, conducted the laboratory
tests, collected and analyzed the data and drafted the paper; UPN:
conducted virus isolation work, collected and analyzed the data. The
final manuscript was approved by all authors.
Funding: Indian Council of Medical Research
(ICMR); Competing interest: None stated.
|
What This Study Adds?
•
Paralytic poliomyelitis cases
have lower levels of serum IgA than non-polio AFP cases.
|
References
1. Mohanty MC, Deshpande JM. Investigation of the
prevalence of antibody immunodeficiency in a polio endemic area in
India. Trans R Soc Trop Med Hyg. 2014;108:258-63.
2. Medical Microbiology, Chapter 1, Immunology
overview by Armond S Glodman and Bellur S Prabhakar, 4th edition,
Edited by Samuel Baron. University of Texas Medical Branch at
Galveston; 1996. Available from:
www.ncbi.nlm.nih.gov/books/NBK7795/#A201. Accessed September 9,
2014.
3. Wright PF, Wieland-Alter W, Ilyushina NA, Hoen AG,
Arita M, Boesch AW, et al. Intestinal immunity is a determinant
of clearance of poliovirus after oral vaccination. J Infect Dis.
2014;209:1628-34.
4. Buisman AM, Abbink F, Schepp RM, Sonsma JA, Herremans
T, Kimman TG. Preexisting poliovirus-specific IgA in the circulation
correlates with protection against virus excretion in the elderly. J
Infect Dis. 2008;197:698-706.
5. Field Guide: Surveillance of Acute Flaccid
Paralysis, Third Edition, September 2005, Available from:
www.searo.who.int/india/.../poliomyelitis/Field_guide_
for_Surveillance_of_Acute_Flaccid_ Paralysis_ 3rd_ edition.pdf.
Accessed September 9, 2014.
6. WHO Polio Laboratory Manual, 4th edition, November
2004. Available from:
www.who.int/vaccines/en/poliolab/WHO-Polio-Manual-9.pdf. Accessed
September 9, 2014.
7. Grassly NC, Jafari H, Bahl S, Sethi R, Deshpande
JM, Wolff C, et al. Waning intestinal immunity after vaccination
with oral poliovirus vaccines in India. J Infect Dis. 2012;205:1554-61.
|
|
|
 |
|

