|
|
|
Indian Pediatr 2014;51: 225 -226 |
 |
Disseminated Cryptococcosis
|
|
Meenakshi Bothra, Prakash Selvaperumal, Madhulika
Kabra and *Prashant Joshi
From the Departments of Pediatrics and *Pathology,
All India Institute of Medical Sciences, New Delhi, India.
Correspondence to: Dr Madhulika Kabra, Additional
Professor, Department of Pediatrics, All India Institute of Medical
Sciences, New Delhi, India.
Email:
[email protected]
Received: January 18, 2013;
Initial review; February 11, 2013;
Accepted; January 08, 2014.
|
|
Background: Fungal infections, especially in immunocompetent
children are uncommon causes of fever of unknown origin. Case
characteristics: A 5-year-old boy with prolonged fever and no
evidence of immunosuppression. Observation: Ultrasound-guided
retroperitoneal lymph node biopsy showed granulomas and intracytoplamic
fungal yeasts; staining charactristics were suggestive of cryptococci.
Clinical and radiological improvement was seen after treatment with
amphoterecin-B. Outcome: Disseminated fungal infection should be
suspected as a cause of pyrexia of unknown origin after ruling out the
commoner causes. Biopsy from enlarged lymph node or organomegaly may
yield the diagnosis when non-invasive tests fail.
Keywords: Cryptococcal infection, Fever of
unknown origin, Immunocompetent.
|
|
Pyrexia of unknown origin (PUO) is mostly due to
an infection, especially in developing countries [1]. We report
disseminated cryptococcosis in a 5-year-old immuno-competent child.
Case Report
A 5-year-old boy was admitted with complaints of
continuous high grade fever for one month along with abdominal
distension, fast breathing and constipation. There was history of
occasional blood in stools and recurrent oral ulcers. There was no
significant past history. On examination, child was conscious and
oriented, febrile with pulse rate of 108/min and respiratory rate of
35/min. There was no pallor, icterus, cyanosis, clubbing, edema,
wasting, stunting or any evidence of micronutrient deficiency. The
abdomen was soft on palpation with a firm, non-tender hepatomegaly
(liver span 13 cm) but no splenomegaly. The examination of chest,
cardiovascular system and central nervous system was normal.
Peripheral smear examination revealed leukocytosis
(Total leukocyte count, 50.2 ◊ 10 3/L)
with eosinophilia (66% eosinophils, 18% neutrophils, 15% lymphocytes and
1% monocytes) without anemia or thrombo-cytopenia. Mantoux test, X-ray
chest and gastric aspirates for Acid-fast bacilli were negative. Bone
marrow examination revealed increase in eosinophils and its precursors
but no abnormal cells. Serum RK-39 antibody detection test and aldehyde
test were negative. Blood culture was sterile. Contrast enhanced
computed tomography (CT) of chest and abdomen showed small focal areas
of consolidation and patchy ground glass opacities in posterior basal
segments of lower lobes, along with multiple centrilobular and
peribronchial tiny nodules in both lungs suggestive of infective
etiology. Enlarged, homogenous, hypodense lymphnodes in pretracheal,
subcarinal, hilar and axillary regions, largest measuring 1.5 cm and
periportal, peripancreatic and retroperitoneal region, largest measuring
3 cm were also reported. In view of lymphadenopathy, hepatomegaly and
pulmonary nodules on CT, differential diagnoses of disseminated fungal
or mycobacterial infections, metastasis, lymphoma, and sarcoidosis were
considered. Work up for the cell mediated, humoral and phagocytic
immunity did not show any evidence of an underlying immunodeficiency.
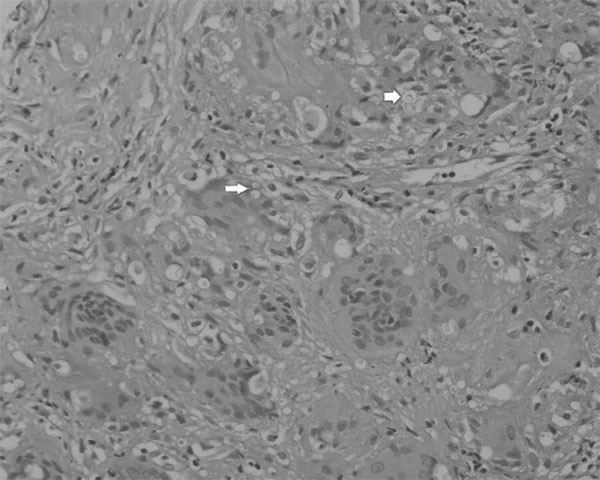
Ultrasound guided retroperitoneal lymph node biopsy showed granulomatous
inflammation with multinucleated giant cells and intracytoplasmic yeast
forms with narrow based budding (Fig. 1). Alcian
blue-periodic acid schiff (PAS) and mucicarmine stained the capsule of
the organisms, morphologically consistent with Cryptococcus. A
definite species categorization could not be done in absence of culture.
Serum and CSF cryptococcal titers were negative.
 |
|
Fig. 1 Hematoxylin and eosin stained
tissue showing multinucleated giant cells with intracytoplasmic
yeast forms with narrow based budding.
|
The child was initially started on broad spectrum
intravenous antibiotics and was given albendazole in view of
eosinophilia. After lymph node biopsy report, he was started on
intravenous amphotericin B (1 mg/kg/d) which was continued for 6 weeks.
The child passed multiple round worms in stool and gradually, the
leukocytosis and eosinophilia also settled. Ultrasono-graphy of abdomen
done at the end of 6 weeks showed some reduction in the size of
retroperitoneal lymph nodes. Child was discharged on 6 mg/kg/d of oral
fluconazole with a plan to continue it for 8 weeks, and then to reassess
the size of lymph nodes on CT abdomen [2]. On follow up, the size of
retroperitoneal lymph nodes decreased further and the child remained
afebrile and asymptomatic.
Discussion
Disseminated cryptococcosis is a systemic fungal
infection generally seen in immunocompromised individuals. Recently,
there have been reports of cryptococcosis in immunocompetent patients
[3]. It usually presents with respiratory tract, central nervous system
and skin involvement. Hepatic, lymph node and bone marrow involvement in
immunocompetent people has been occasionally reported [4,5].
Cryptococcal infection is difficult to diagnose because of the
non-specific signs and symptoms, the insidiousness of the course and the
coexistence with other diseases [3]. The report of retroperitoneal lymph
node biopsy helped us clinch the diagnosis of disseminated
cryptococcosis, after commoner causes like disseminated tuberculosis and
lymphoreticular malignancy were ruled out. Diagnosis of cryptococcal
infection depends upon demonstration of growth of organisms on
Saboraudís media with characteristic biochemical reactions (urease,
phenyloxidase) or demonstration of encapsulated yeast like organisms on
India ink or PAS staining followed by positive mucicarmine or Masson
Fontana staining. Demonstration of cryptococcal capsular polysaccharide
antigen in titers more than 1:8 in serum or CSF is also diagnostic [4].
Amphotericin B (0.7 to 1.0 mg/kg/d, intravenously)
plus flucytosine (100 mg/kg/d, orally, in four divided doses) is
recommended for at least four weeks for initial therapy [6].
Consolidation therapy should then be initiated with fluconazole (6
mg/kg/d) for eight weeks, and 3 mg/kg/d for six to twelve months [2].
We conclude that systemic fungal infections including
disseminated Cryptococcosis is possible even in immunocompetent children
and should be considered as cause of PUO after commoner causes have been
ruled out.
Contributors: MB: compiled clinical details and
investigations and drafted the manuscript; PS: work up of the patient
and drafting the manuscript; MK: supervised the management of child and
revised the manuscript and PJ: pathological diagnosis and drafting the
manuscript.
Funding: none; Competing interests: None
stated.
References
1. Kejariwal D, Sarkar N, Chakraborti SK, Agarwal
V, Roy S. Pyrexia of unknown origin: a prospective study of 100 cases. J
Postgrad Med. 2001;47:104-7.
2. Chen SC, Playford EG, Sorrell TC. Antifungal
therapy in invasive fungal infections. Curr Opin Pharmacol. 2010;10:1-9.
3. Paranada KS, Victorio-Navarra ST, Dy EE.
Disseminated cryptococcosis in two Filipino patients. Phil J Microbiol
Infect Dis. 1999;28:109-16.
4. Agarwal V, Sachdev A, Agarwal G, Mohan H, Anjali.
Disseminated cryptococcosis mimicking lymphoreticular malignancy in
a HIV negative patient. JK Science. 2004;6:93-5.
5. Lee HS, Park HB, Kim KW, Sohn MH, Kim KE, Kim MJ,
et al. A case of mediastinal and pulmonary cryptococcosis in a
3-year-old immunocompetent girl. Pediatr Allergy Respir Dis (Korea).
2011;21:350-5.
6. Saag MS, Graybill RJ, Larsen RA, Pappas PG,
Perfect JR, Powderly WG, et al. Practice guidelines for the
management of cryptococcal disease. Clin Infect Dis. 2000;30:710-8.
|
|
|
 |
|

