R
eversible posterior
leucoencephalopathy (RPLS) is a clinico-radiological syndrome, manifesting
with headache, confusion, seizures, visual disturbances and radiological
findings of bilateral grey and white matter abnormalities suggestive of
edema in the posterior regions of cerebral hemispheres(1). Described
mainly in adults, it has also been reported in children(2,3,4). We report
a rare case of post streptococcal glomerulonephritis manifesting as
reversible posterior leucoencephalopathy syndrome.
Case Report
A 12 year female presented to us with complaints of
headache, vomiting for two days and loss of vision for 1 day. Headache was
mild, bi-frontal, continuous, not interrupting sleep pattern,
non-radiating and relieved with vomiting, which was non projectile and non
bilious. There was no past or family history of headache. There was no
history of fever, altered urine color, decreased urine output, any
preceding skin or upper respiratory infection. On examination, patient was
conscious, afebrile, with a pulse rate of 120/min regular, respiratory
rate 24/min regular, BP 160/130 mmHg and no edema. On CNS examination,
fundus was normal and pupils were bilateral central, circular, reacting to
light, but perception to light was absent, bilateral deep tendon reflexes
were brisk and plantars were extensor. Rest of the systemic examination
was normal.
The blood counts, serum electrolytes, and liver
function tests were normal. Blood urea was 54 mg/dL, serum creatinine 1.31
mg/dL and serum uric acid 7.04 mg/dL. Urine examination was normal on the
first two days of hospitalization: however, on the third day of
hospitalization, urine examination showed 6-8 pus cells/ hpf and plenty of
RBCs. Urine culture was sterile. Ultrasound examination showed bilateral
loss of cortico-medullary differentiation with normal sized kidneys. ASO
titer was raised i.e. 800 U/L. Antinuclear antibody and antineutrophil
antibody titers were negative. No pathogenic bacteria were grown in throat
culture. Complement C 3 level was 9 mg/dL (normal: 90-180 mg/dL).
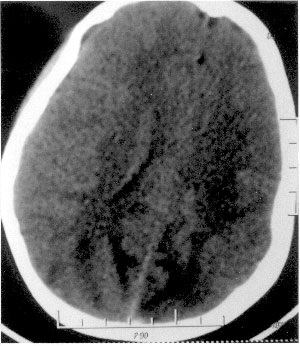
CECT brain showed bilateral extensive ill defined
symmetrical hypodensities involving the white matter of high parietal and
occipital lobes. (Fig. 1) Patient was started on furosemide
and sodium nitroprusside, the blood pressure was gradually reduced. She
regained vision on third day of hospitalization and by the seventh day of
illness, her abnormal neurological findings and vision was normal. She was
discharged on nifedipine. On follow-up after 2 weeks, serum complement
(C3) level, electroencephalogram, ultrasound and CT head were normal.
 |
|
Fig. 1 Symmetrical hypodensities involving
the posterior regions of cerebral hemispheres. |
Discussion
Reversible posterior leucoencephalopathy syndrome in
children has been shown to be associated with ganglioneuroma,
Henoch-Schönlein purpura, acute lymphoblastic leukemia, steroids,
hemolytic uremic syndrome, Addison’s disease, hypertension, intrabdominal
neurogenic tumors, porphyria and bone marrow transplant(2-6). In our
patient, headache was the main presenting complaint, followed by nausea,
vomiting, and visual disturbance in the form of loss of vision. An almost
similar clinical picture was reported earlier(1,3). Other reported
clinical symptoms and signs include altered alertness and behavior,
seizures, altered speech and visual perception like blurred vision,
hemianopsia, and visual neglect(5). In patients of RPLS, seizures
(frequently new onset, secondary generalized occipital lobe seizure)
almost always occurs during the course of illness(7). Our case did not
present with disturbance in consciousness or seizures. Prolonged seizures,
hypertension or both may result in permanent neurological deficits and
cerebral infarctions, if not treated properly(5). A few of them may not
recover completely and develop neurodevelopmental sequelae(2).
The diagnosis of RPLS was established due to the
presence of hypertension, typical bilateral CT findings, and reversibility
of the lesions. The most common abnormality on neuroimaging is edema
involving the white matter in the posterior portions of cerebral
hemispheres, especially in the parieto-occipital regions(3). Our case also
had the same findings. Kwon, et al.(2), in their study of 12
children with RPLS, found that cortical grey matter was predominantly
involved in four patients and in two patients, only grey matter was
involved. Since it involves both grey and white matter, some authors have
suggested that it should be renamed as occipital parietal encephalopathy
syndrome(8). Involvement of brain stem, cerebellum, basal ganglion, and
frontal lobes has also been reported(3,9). The calcarine and paramedian
occipital lobe structures are usually spared and that distinguishes RPLS
from bilateral infarction of the posterior cerebral artery territory(5).
An important characteristics of RPLS is reversibility of the imaging
abnormalities, as seen in our case.
The pathophysiology of RPLS is complex. It is probably
a brain capillary leak syndrome related to hypertension, fluid retention
and possibly the cytotoxic effects of immunosuppressive agents on the
vascular endothelium(5). The relative paucity of sympathetic innervation
in the posterior brain leads to susceptibility to hyperperfusion and
vasogenic edema during acute blood pressure elevations which may explain
the presence of majority of the lesions in the vascular territory of
posterior circulation(6). Children develop RPLS at a lower absolute
pressures than adults owing to the relative "left shift" of their range of
cerebral blood flow autoregulation(6)
Contributors: SG and BT were involved in diagnosis
and case management. VKG reviewed the literature and prepared the initial
draft. SG and BT prepared the final version of the paper.
Funding: None.
Competing interests: None stated.
References
1. Hinchey J, Chaves C, Appignani B, Breen J, Pao L,
Wang A, et al. A reversible posterior leucoencephalopathy syndrome.
N Engl J Med 1996; 334: 494-500.
2. Kwon S, Koo J, Lee S. Clinical spectrum of
reversible posterior leucoencephalopathy syndrome. Pediatr Neurol 2001;
24: 361-364.
3. Prasad N, Gulati S, Gupta RK, Sharma K,
Gulati K, Sharma RK, et al. Spectrum of radiological changes in
hypertensive children with reversible posterior leukoencephalopathy. Br J
Radiol 2007; 80: 422-429.
4. Singhi P, Subramanian C, Jain V, Singhi S, Ray M.
Reversible brain lesions in childhood hypertension. Acta Paediatr 2002;
91: 1005-1007.
5. Özcakar ZB, Ekim M, Fitoz S, Teber S, Hizel S, Acar
B, et al. Hypertension induced reversible posterior
leukoencephalopathy syndrome: a report of two cases. Eur J Pediatr 2004;
163: 728-730.
6. Jones BV, Egelhoff JC, Patterson RJ. Hypertensive
encephalopathy in children. Am J Neuroradiol 1997;18: 101-106.
7. Garg RK. Posterior leucoencephalopathy syndrome.
Postgrad Med J 2001; 77: 24-28.
8. Pavlakis SG, Frank Y, Kalina P, Chandra M, Lu D.
Occipital- parietal encephalopathy: A new name for an old syndrome.
Pediatr Neurol 1997; 16: 145-148.
9. Schwartz RB, Jones KM, Kalina P, Bajakian RL,
Mantello MT, Garada B, et al. Hypertensive encephalopathy: findings
on CT, MR imaging, SPECT imaging in 14 cases. Am J Roentgenol 1992; 159:
379-383.

