|
|
|
Indian Pediatr 2010;47: 245-254 |
 |
Hemoptysis in Children |
|
G S Gaude
From Department of Pulmonary
Medicine, JN Medical College, Belgaum, Karnataka,
India.
Correspondence to: Dr G S Gaude,
Professor and Head, Department of Pulmonary
Medicine, J N Medical College, Belgaum 590 010,
Karnataka, India.
Email:
[email protected]
Received: November, 11, 2008;
Initial review: May, 8, 2009;
Accepted: July 27, 2009.
|
|
Abstract
Context: Pulmonary
hemorrhage and hemoptysis are uncommon in
childhood, and the frequency with which they are
encountered by the pediatrician depends largely on
the special interests of the center to which the
child is referred. Diagnosis and management of
hemoptysis in this age group requires knowledge
and skill in the causes and management of this
infrequently occurring potentially
life-threatening condition.
Evidence acquisition: We
reviewed the causes and treatment options for
hemoptysis in the pediatric patient using Medline
and Pubmed.
Results: A focused physical
examination can lead to the diagnosis of
hemoptysis in most of the cases. In children,
lower respiratory tract infection and foreign body
aspiration are common causes. Chest radiographs
often aid in diagnosis and assist in using two
complementary diagnostic procedures, fiberoptic
bronchoscopy and high-resolution computed
tomography. The goals of management are threefold:
bleeding cessation, aspiration prevention, and
treatment of the underlying cause. Mild hemoptysis
often is caused by an infection that can be
managed on an outpatient basis with close
monitoring. Massive hemoptysis may require
additional therapeutic options such as therapeutic
bronchoscopy, angiography with embolization, and
surgical intervention such as resection or
revascularization.
Conclusions: Hemoptysis in
the pediatric patient requires prompt and thorough
evaluation and treatment. An efficient systematic
evaluation is imperative in identifying the
underlying etiology and aggressive management is
important because of the potential severity of the
problem. This clinical review highlights the
various etiological factors, the diagnostic and
treatment strategies of hemoptysis in children.
Key words: Children, Hemoptysis,
Management, Pulmonary hemorrhage, Review.
|
|
Pulmonary hemorrhage
was not commonly described in children in the early
texts, although it was noted to occur. Hemoptysis is
defined as the expectoration of blood or
blood-tinged sputum from the lower respiratory
tract. Although common in adults, blood tinged
sputum is a rare presenting symptom in children. The
diagnosis of pediatric hemoptysis can be
challenging. Children tend to swallow their sputum;
therefore, hemoptysis may go unnoticed unless the
bleeding is sub-stantial(1). Coupled with this, the
inability to provide a complete history and to
cooperate with a thorough physical examination may
further compound the diagnostic dilemma. Thus,
hemoptysis can serve as a source of significant
anxiety for the patient, the family, and the
pediatrician.
Most important in children is to
first establish that the child is experiencing
hemoptysis. Extra-pulmonary bleeding, such as those
arising from the nose, or the gastrointestinal
tract, may be incorrectly attributed to hemoptysis.
This is known as pseudo-hemoptysis. As the
diagnostic and treatment strategies differ markedly,
the two sources must be differentiated. The blood in
hemoptysis is bright red in color and may be admixed
with sputum and frothy. The blood in hemetemesis is
dark red or brown and may be mixed with food
particles(2). One also has to differentiate
factitious hemoptysis from real hemoptysis. Once the
distinction is made, the physician can proceed to
uncover the underlying cause. Hemoptysis is
classified as non-massive or massive based on the
volume of blood loss; however, there are no uniform
definitions for these categories. Hemoptysis is
considered massive if blood loss is more than 200 mL
per day(3).
Pulmonary hemorrhage may even be
present in a previously healthy infant in whom
neonatal medical problems have been ruled out. This
pulmonary hemorrhage can appear as hemoptysis or
blood in the nose or airway with no evidence of
upper respiratory or gastrointestinal bleeding.
Patients have acute respiratory distress or failure,
requiring mechanical ventilation and chest
radiography, and usually demonstrate bilateral
infiltrates. Centers for Disease Control and
Prevention (CDC) has given criteria for a confirmed
case of pulmonary hemorrhage in a previously healthy
infant aged
£
1 years of age with gestational age of
³
32 weeks, with no history of neonatal medical
problems, and whose conditions meets all the
following three criteria(4):
(i) Abrupt or sudden
onset of overt bleeding or obvious evidence of
blood in the airway, including epistaxis,
hemoptysis or frank blood below the larynx at
visualization.
(ii)
Severe-appearing illness leading to acute
respiratory distress or respiratory failure
resulting in admission in PICU or NICU with
intubation and mechanical ventilation.
(iii) Diffuse
unilateral or bilateral pulmonary infiltrates
visible on chest X-ray or CT scan of thorax, and
these findings should be documented within 48
hours of examination of infant.
Criteria for probable case of
pulmonary hemorrhage in the infant include a
previously healthy infant aged
£
1 year with a gestational age of
³
32 weeks, with(4):
(i) Who has
sudden onset of bleeding from the airway, with or
without respiratory distress, with or without
intubation and with or without pulmonary
infiltrates on chest X-ray or CT scan;
(a) Who died and had
evidence of bleeding from the airway found on
autopsy or postmortem.
Etiology
The etiology of hemoptysis in
children is as varied as in adults. The various
causes of hemoptysis in children are summarized in
Table I. Important causes of massive
hemoptysis in children are: bronchiectasis,
pulmonary tuberculosis, CHD, bronchial AV
malformation, foreign body aspiration, cystic
fibrosis, bronchial adenomas, DIC and tracheostomy-related.
TABLE I
Causes of Hemoptysis in Children
| • Infections - pneumonia,
tracheobronchitis |
| • Cystic fibrosis |
• Congenital heart diseases - ASD, VSD,
complex cyanotic heart diseases, tetralogy of
fallot, truncus
arteriosus, transposition of the great arteries |
| • Tuberculosis |
| • Foreign body aspiration |
| • Nasopharyngeal bleeding |
| • Tracheostomy-related |
| • Bronchiectasis |
| • Pulmonary neoplasms |
| • Pulmonary hemosiderosis |
| • Factitious hemoptysis |
| • Miscellaneous – invasive aspergillosis,
pulmonary arteritis, catamenial
hemoptysis, hydatid cysts in lungs |
| • Unknown causes |
Acute lower respiratory tract
infection, either in the form of pneumonia or
tracheobronchitis, accounts for almost up to 40% of
the cases(5). In a 10 year retrospective study of
hemoptysis in children, Coss-Bu, et al.(6)
observed pneumonia to be the most frequent cause
accounting for 31% of the episodes of hemoptysis in
children. The presence of an infectious process
(e.g. necrotizing pneumonia, tuberculosis, lung
abscess, infected bronchiectasis) leads to
destruction of lung parenchyma and erosion of blood
vessels, resulting in hemoptysis. Infections have
been reported as the most common etiology of
hemoptysis in several studies in children(7,8).
Although tuberculosis used to be commonly
implicated, few cases have been reported in
pediatric literature(5,9). Only one study by Crocco,
et al.(10) reported high prevalence of
hemoptysis in tuberculosis (80%). In countries like
India where the prevalence of tuberculosis is high,
this infection should never be neglected and should
rank much higher. Another important cause of
hemoptysis in children is bronchiectasis, which can
be unilateral or bilateral. The bronchiectasis
occurs due the repeated respiratory tract infections
since childhood. Chronic bacterial endobronchial
infection and inflammation of the mucosa damage and
destroy mucociliary defences, and this leads to
secretion stasis, which in turn propagates further
bacterial infection, and increases airway
inflammation and bronchial dilatation(11). The
infection is usually bacterial in nature and
consists of Streptococcus pneumonie,
Staphylococcus aureus, M. catarrhalis, klebsiella
species, or Pseudomonas aeruginosa.
Aspergillus infection of the lungs either in the
form of allergic bronchopulmonary aspergillosis (ABPA)
or invasive aspergilliosis can occur in children and
some cases of hemoptysis have been reported(12).
Congenital heart disease can be a
source of profuse bleeding in a child. With the
advent of corrective cardiac surgery, the incidence
of hemoptysis in this setting has declined
significantly(5). Hemoptysis in CHD occurs most
frequently with pulmonary vascular obstructive
disease, but it can also occur in conjunction with
enlarged collateral bronchial circulation.
Hemoptysis in this condition is caused by erosion of
a tortuous dilated bronchial artery into a bronchus,
from rupture of an atherosclerotic bronchial artery
plaque, or from localized pulmonary infarction at
the bronchopulmonary anastomosis(13). Recently, life
threatening hemoptysis has been reported in a child
due to aortic pseudoaneurysm, which was proved by
the aortic biopsy showing neutrophilic infiltration
of the mucosa(14).
Foreign body aspiration is always
considered in the differential diagnosis of
pediatric hemoptysis. The bleeding in this case
results from the mechanical trauma to the
respiratory epithelium or the ensuing inflammatory
reaction, especially to vegetable matter(15).
Tom, et al.(16) identified foreign bodies as
the second most common cause of hemoptysis. We have
observed four children with hemoptysis, who had
vegetable matter impacted in the bronchi, which were
successfully removed with bronchoscope.
In the Western countries,
hemoptysis is relatively common in patients with
cystic fibrosis (CF), especially with increased
survival into adulthood, and advances in medical
treatment. Approximately 5% of patients with CF may
present with massive hemoptysis due to
bronchiectasis. In one study(2), CF contributed to
65% of cases of pediatric hemoptysis in a 10-year
retrospective study. Also the Patients with CF also
had longer hospitalization compared to other causes
of hemoptysis, reflecting the chronic nature and the
multitude of problems associated with CF. There is
hyperplasia, tortuosity and dilatation of bronchial
arteries due to chronic inflammation, and hemorrhage
results from erosion of these dilated, thin walled
bronchial vessels after successive pulmonary
infections(5).
Neoplasms of the respiratory
tract are rare in children, but endobronchial or
pulmonary parenchymal tumors may cause significant
bleeding. Tumors that may cause hemoptysis include
bronchial carcinoid, bronchial adenoma,
endobron-chial metastasis, mediastinal teratomas,
tracheal tumours, or bronchial arteriovenous
malformations in children(17). Hemoptysis is a
well-recognized complication of long-term
tracheostomies. Wetmove, et al.(18) reported
that significant bleeding may occur in approximate
10% of the patients with long-term tracheostomy.
Fabian and Smitheringale(19) found tracheostomy
related hemoptysis to be second most common cause of
hemoptysis (15.5%). Typically, the bleeding is
described as pink or red–tinged secretions on
suctioning the tracheobronchial tree.
Idiopathic pulmonary
haemosiderosis is a rare cause of diffuse alveolar
hemorrhage of unknown etiology. It occurs most
frequently in children, has a variable natural
history with repetitive episodes of diffuse alveolar
hemorrhage, and has been reported to have a high
mortality. The recurrent episodes of diffuse
pulmonary hemorrhage may present as hemoptysis(20).
Many patients develop iron deficiency anemia
secondary to deposition of haemosiderin iron in the
alveoli. Recently, Kabra, et al.(21)
described hemoptysis in about 58% of children in
patients with pulmonary hemosiderosis. Most of these
patients had small and recurrent hemoptysis.
Examination of sputum and broncho-alveolar lavage
fluid can disclose hemosiderin-laden alveolar
macrophages (siderophages), and the lung biopsy
shows numerous siderophages in the alveoli, without
any evidence of pulmonary vasculitis, nonspecific/granulomatous
inflammation, or deposition of immunoglobulins. In
some of these patients normo-complement urticarial
vasculitis has been observed in children, and this
may predispose for the hemoptysis(22).
Other causes of hemoptysis are
far less common, such as bleeding from localized
lesions in upper airways or bleeding into the lungs
as like part of a systemic disease systemic lupus
erythematosis, Goodpasture’s syndrome, pulmonary
thromboembolism, hydatid cyst, and even duplication
cyst of the stomach can cause hemoptysis in
children(23-26). Isolated pulmonary arteritis can
lead to massive hemoptysis in children(27).
Recently, catamenial hemoptysis has been described
in a 12 year old child and fibreoptic bronchoscopy
revealed presence of endobronchial
endometriosis(28).
Factitious hemoptysis is
considered in the differential diagnosis if no
etiology is discernible after a thorough evaluation,
especially when the medical history or patient’s
behavior is unusual(29). Covert biting of the buccal
mucosa has been attributed to cause hemoptysis in
these children(30). Psychological counseling is
usually required in such children.
Diagnosis
Hemoptysis in children should be
evaluated systematically. The investigations begin
with a detailed medical history and physical
examination. First, the hemoptysis has to be
differentiated from hematemesis. Historic clues are
useful for differentiating hemoptysis from
hematemesis (Table II). Patient
history also can help identify the anatomic site of
bleeding, differentiate between hemoptysis and
pseudohemoptysis, and narrow the differential
diagnosis. Once true hemoptysis is suspected, the
investigations should focus on the respiratory
system.
TABLE II
Differentiating Features of Hemoptysis and Hematemesis
| Hemoptysis |
Hematemesis |
| History |
| Absence of nausea and vomiting |
Presence of nausea and vomiting |
| Lung disease |
Gastric or hepatic disease |
| Asphyxia possible |
Asphyxia unusual |
| After the episode, sputum is |
After the episode, sputum is always blood
tinged always clear |
| Sputum examination |
| Frothy |
Rarely frothy |
| Liquid or clotted appearance |
Coffee ground appearance |
| Bright red to pink |
Brown to black |
| Laboratory Parameters |
| Alkaline pH |
Acidic pH |
| Mixed with macrophages |
Mixed with food particles and neutrophils |
The physician should always
inquire about the possibility of foreign baby
aspiration, including choking or coughing episodes,
and new onset wheezing. A history of chronic lung
disease or CHD is also important. This is followed
by thorough examination of the neck and head.
Special attention should be given to the oral cavity
and nasopharynx as the potential sources of
bleeding. Lung examination may reveal localized
wheezing, suggesting foreign body, or rales or
decreased breath sounds, which may be associated
with an infectious process(5).
Routine blood test with complete
haemogram has to be done in all the children. This
is imperative because children generally tend to
swallow blood and the amount of bleeding is likely
to be underestimated. As an infectious etiology is
common, sputum is evaluated for bacterial, fungal
and mycobacterial organisms. Sputum culture will be
helpful for identifying the pathogens and
sensitivities to various antibiotics.
Chest radiography serves as a
valuable screening technique. Unilateral air
trapping with hyper-inflation may suggest the
diagnosis of foreign body aspiration(1). Focal or
interstitial infiltrates may help the diagnosis of
infection. Other helpful findings include pulmonary
nodules, hilar adeno-pathy, pleural effusion and
cardiomegaly. In approxi-mately one third of
children with hemoptysis, chest radiographs may be
normal. High Resolution Computed Tomography (HRCT)
can be useful in further delineation of chest
radiography findings. Contrast studies are helpful
to differentiate between vascular structures and
solid masses(2). In recent years, HRCT scan of
thorax has become the most accurate and sensitive
noninvasive diagnostic tool for the evaluation of
bronchiectasis(31).
If the etiology of hemoptysis is
not discovered after aforementioned workup, and if
the bleeding is recurrent, bronchoscopy which may be
rigid or fibreoptic, is indicated to identify source
of bleeding(9,10).
Fibreoptic bronchoscopy can be performed with
sedation and allows more detailed evaluation of
distal bronchial tree. However, it does not permit
effective ventilation and removal of blood clots. In
contrast, rigid bronchoscope offers ventilation and
helps localize site of bleeding. It is also ideal
for suctioning of clotted blood and is also more
effective for removal of airway foreign bodies(32).
In one study, rigid bronchoscopy was performed 24
times in 18 patients for diagnostic and therapeutic
reasons. The various findings included: blood,
mucosal inflammation, purulence, tracheal abrasions,
gradation tissue and bronchial mass. The diagnostic
yield was 61%(5). The diagnostic yield of
bronchoscopy in hemoptysis ranges from 40% to 100%
in various studies(1,9).
Cardiac evaluation should be
considered in patients with hemoptysis unexplained
by pulmonary causes, even in the absence of overt
cardiac symptoms(33). Echocardiography should be
performed for the evaluation of any suspected
congenital cardiac disease. Pulmonary
thromboem-bolism is a rare cause of hemoptysis in
children, and a combination of diagnostic procedures
must be used to identify a suspected or confirmed
case of pulmonary thromboembolism in children,
including ventilation perfusion studies(24). When no
other cause is found for pulmonary hemorrhage, the
presumed diagnosis is idiopathic pulmonary
hemosiderosis(21). In these patients, sputum and
bronchoalveolar lavage fluid can disclose
haemosiderin-laden alveolar macrophages (siderophages).
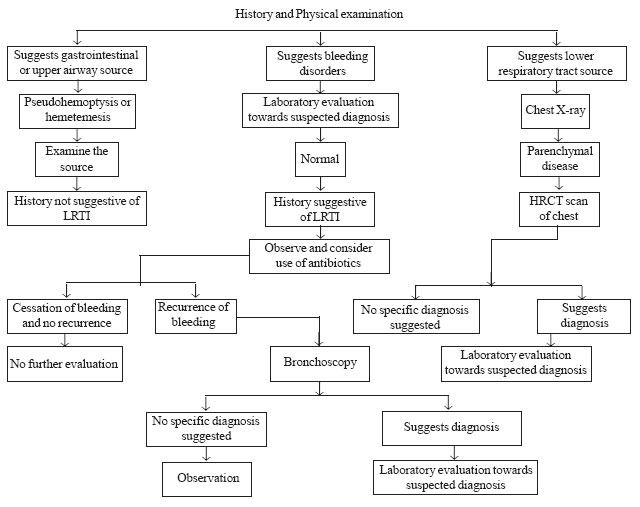
Figure 1 provides an
algorithm for the evaluation of hemoptysis in
children.
 |
|
F IG.
1
Algorithm for diagnosing hemoptysis in
children. |
Treatment
Management of the child with
hemoptysis depends on two important issues – the
underlying causes and the severity of the bleeding.
The three goals of therapy are: to prevent
asphyxiation, stop the bleeding, and treat the
primary cause. Most of the cases are self-limited
and will resolve spontaneously.
Minor hemoptysis
Minor hemoptysis is managed
symptomatically, by giving cough suppressants like
dextromethorphan and oral/parental haemostatic
agents like ethymsylate or Botropase, reassurance of
the patient and parents, and the treatment of the
underlying cause. If a specific etiology is
identified, appropriate therapy of the underlying
disease should be initiated. Pulmonary infections
are treated with appropriate antibiotics. Cystic
fibrosis exacerbations are managed with antibiotics
and corticosteroids. Tracheostomy-related trauma is
managed by modifying the suctioning technique, using
soft red rubber catheters, and humidification.
Pulmonary tuberculosis should be treated with
anti-tubercular therapy. Idiopathic pulmonary
hemosiderosis is treated with prednisolone. Kabra,
et al.(21) recently treated children with
pulmonary hemosiderosis with prednisolone and
hydroxychloroquin followed by inhaled
corticosteroids, and found favorable response in
majority of the patients.
Massive hemoptysis
In small number of cases, the
child may present with life-threatening hemorrhage
(>8 mL/kg every 24 hours or 200 mL every 24 hrs).
Massive hemoptysis can quickly progress to acute
respiratory distress in a child. These children
require multiple procedures to stabilize the airways
and to control blood loss(34). Intravenous fluids
and blood products are given to prevent
cardiovascular collapse from the exsanguination of
blood. Reversal of any coagulation disorder and
protecting the non-bleeding lung from aspiration by
placing the bleeding side down and selectively
intubating the good lung, in cases of massive
hemoptysis, should be undertaken(35). The use of
cough suppressants containing codeine has been
controversial as they have the potential to alter
the level of consciousness and hence lead to the
risk of aspiration. However, judicious use and
careful titration should avoid this problem(36). The
various options available for massive hemoptysis
are: endoscopic balloon occlusion of a lobe or main
bronchus, topical airway vasoconstrictors, use of
Nd-YAG laser, CO 2
laser bronchoscopy, endoscopic tumor excision,
transcatheter embolisation of bronchial vessels and
lobectomy. The foremost objectives in management of
massive hemoptysis are to protect the airways,
maintain oxygenation, stop the bleeding and maintain
sufficient blood volume. This is critical because
most of the deaths occur due to asphyxiation, not
exsanguination. The airway should be kept patent
with an endotracheal tube or rigid bronchoscope in
cases of severe respiratory distress. The bleeding
should be localized without delay. Although there is
debate regarding timing of bronchoscopy, most of the
authors favor early bronchoscopy(35). This approach
is associated with the best success of identifying
the bleeding site. In most cases, fibreoptic
bronchoscopy via an existing endotracheal tube is
the easiest and safest approach. If fibreoptic
bronchoscopy fails to identify the bleeding site, an
experienced endoscopist can perform rigid
bronchoscopy if time permits. Rigid bronchoscopy
protects the airways and helps in localization of
bleeding site. Topical vasoconstrictors, such as
oxymetazoline or epinephrine (1:20000), iced 0.9%
saline, fibrinogen-thrombin glues or Botropase are
applied through the bronchoscope to curtail the
bleeding. In addition, endoscopic tamponade can be
performed by balloon catheter or with bronchoscopic
pressure(2). Patients with alveolar hemorrhage
syndromes, blood dyscrasias, or those on
anticoagulant or antiplatelet therapy should receive
appropriate medical therapy rather than invasive
interventions.
If the hemorrhage continues
despite endoscopic measures, or if the bleeding site
cannot be localized, emergency arteriography is
carried out(5). Selective bronchial artery
embolisation (BAE) is effective in the emergency
management of life-threatening hemoptysis(37).
Bronchial arteriography identifies the bleeding
vessel and selective embolisation with absorbable
gelatin sponge, steel or platinum coils, or
polyvinyl alcohol particles controls the hemorrhage.
In one study(34), there was immediate cessation of
hemorrhage in 77% of the cases; while long term
control beyond 3 months was achieved in 45% of
patients. Another study(37) found bronchial
embolisation to be superior to medical management
for resolution of life threatening bleeding. BAE is
effective in controlling hemoptysis in most of the
cases although recurrent bleeding is not uncommon.
BAE is technically challenging and requires
angiographic skills that are not always available in
pediatric hospitals(38). Complications are not
uncommon and may be severe or even fatal. The most
serious complication of embolisation therapy is
neurological damage due to embolisation of the
spinal arteries(5). Recently, del Gregorio, et al.(39)
have reported their experience with bronchial artery
embolisation in patients with hemoptysis; about 31%
of these patients were having bronchiectasis. In
this study, clinically successful outcome with BAE
was observed in 91.1% of the cases, and repeat
embolisation was required in 6.7% of the cases.
Recurrence of hemoptysis was observed in 22.3% of
cases, but only 10.4% of patients required repeat
embolisation. Minor complications that did not
require treatment were observed in 28% of cases.
Thus, BAE is a nonsurgical treatment that is safe
and effective in patients with massive
hemoptysis(39).
If bronchial artery embolisation
fails to control hemoptysis, surgical management
should be considered. Massive hemoptysis carries
greater than 50% mortality without surgical
intervention. Surgery is offered to patients who can
withstand general anesthesia and pulmonary
resection. Immediate identification of the bleeding
site by bronchoscope is followed by resection of the
bleeding source(40). Segmentectomy or lobectomy is
preferred to pneumonectomy, as the latter carries a
much higher mortality rate. One study(41) reported
83% survival in 65 resections performed for massive
hemoptysis in this setting. Simrali, et al.(42)
recently published their experience with surgery for
bronchiectasis in 176 children of less than 16 years
with hemoptysis. They performed various procedures
including segmental resection, lobectomy,
pneumonectomy and bilateral resection in patients
with bronchiectasis. Complete resection was
performed in almost 94% of the cases. The patients
were followed for a mean period of 4.3 years.
Successful outcome was observed in 73% of cases,
while improved outcome was seen in another 23% of
the cases. It was observed that there was good
improvement in the quality of life even after
pneumonectomy and bilateral resection of the lungs.
Hemoptysis could be controlled in all of these
cases. It was concluded that with acceptable
mortality and morbidity rates and high chances of
cure after complete resection, surgical treatment is
a successful and reliable method of treatment in
childhood bronchiectasis that yield marked
improvement in the quality of life(42). Chan, et
al.(27) has also treated isolated pulmonary
arteritis with lobectomy, as the hemoptysis could
not be controlled with the medical measures alone.
Hence, surgical options have to be considered if
massive hemoptysis remains uncontrolled in spite of
medical therapy.
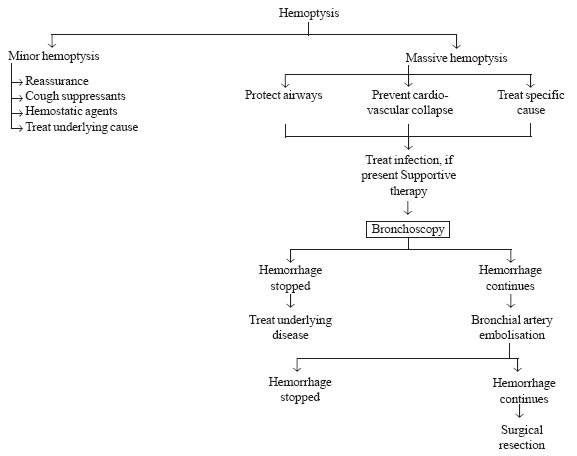
Figure 2 provides
an algorithm for the management of hemoptysis in
children.
 |
|
F IG.
2
Algorithm for management of hemoptysis in
children. |
Hemoptysis in children is rare,
but if occurs, it is a frightening symptom for the
parents. The patient’s history should help determine
the amount of blood and differentiate between
hemoptysis, pseudo-hemoptysis, and hematemesis. A
focused physical examination can lead to the
diagnosis in most cases. Mild hemoptysis often is
caused by an infection and can be managed on an
outpatient basis with close monitoring. Massive
hemoptysis requires immediate hospitalization and
proper therapeutic interventions have to be
initiated at the earliest to stop the bleeding and
to prevent its recurrence.
Funding: None.
Competing interests: None
stated.
References
1. Pianosi P, Al Sadoon H.
Hemoptysis in children. Pediatric Rev 1996; 19:
344-348.
2. Turcios NL, Vega M. The child
with hemoptysis. Hosp Pract 1987; 22: 217-218.
3. Knott-Craig CJ, Oostuizen JG,
Rossouw G, Joubert JR, Barnard PM. Management and
prognosis of massive hemoptysis. Recent experience
with 120 patients. J Thorac Cardiovasc Surg 1993;
105: 394-397.
4. CDC. Acute idiopathic
pulmonary hemorrhage among infants – Recommendations
from the working group for investigation and
surveillance. MMWR, 2004; 53(RR02): 1-12.
5. Batra PS, Holinger LD.
Etiology and management of pediatric hemoptysis.
Arch Otolaryngol Head Neck Surg 2001; 127: 377-382.
6. Coss-Bu JA, Sachdera RC,
Bricker JJ, Harrison GM, Jeferson LS. Hemoptysis – a
10-year retrospective study. Pediatrics 1997; 100:
e7.
7. Tom LWC, Weisman RA, Haneller
S.D. Hemoptysis in children. Ann Otol Rhinol
Laryngol 1980; 89: 419-424.
8. Thompson JW, Nguyen CD, Lazar
RH. Evalution and management of hemoptysis in
infants and children Ann Otol Rhinol Laryngol 1996;
105: 516-520.
9. Ulong KS, Wang CR, Lim TY.
Hemoptysis in children. Chang Gung Med J 1998; 21:
57-62.
10. Corey R, Hal KM. Major and
massive hemoptysis: reassessment of conservative
management. Am J Med Sci 1987; 294: 301-309.
11. Barker AF, Ahmed SY.
Bronchiectasis. In: Fishman AP, Elias JA,
Fishman JA, Grippi MA, Senior RM, Pack AI, editors.
Fishman’s Pulmonary Diseases and Disorders. 4 th
Edition, New York: McGraw Hill Medical Publishers;
2008. p. 2183-2192.
12. Crassad N, Halden H, Piens
MA, Pondarre C, Hadden R, Galambrum C, et al.
Invasive aspergillosis in a pediatric hematologic
department: a 15 year review. Mycosis 2008; 51:
109-116.
13. Haroutunian LM, Neill CA.
Pulmonary complications of congenital heart disease:
hemoptysis. Am Heart J 1972; 84: 540-549.
14. Shrivastva V, Vaideeswar P,
Jana S, Patwardhan A, Sathe P, Khandekar J, et al.
Aortic pseudoaneurysm: cause of life threatening
hemoptysis in a 13 month old child. J Card Surg
2008; 23: 553-555.
15. Dore ND, Landar LI, Hallam L.
Hemoptysis in healthy children due to unsuspected
foreign body. J Pediatric Child Health 1997; 33:
448-450.
16. Tom LW, Weisman RA, Handler
SD. Hemoptysis in children. Ann Otol Rhinol Laryngol
1980; 89: 419-424.
17. Hancock BJ, Dilorenzo M,
Youssef S, Yazbeck S, Marcotte JE, Collin I.
Childhood primary pulmonary neoplasms. J Pediatric
Surg 1993; 28: 1133-1136.
18. Wetmore RF, Handler SD,
Patsic WP. Pediatric tracheostomy: experience during
the past decade. Ann Otol Rhinol Laryngol 1982; 91:
628-632.
19. Fabian MC, Smitheringale A.
Hemoptysis in children: the hospital for sick
children experience. J Otolaryngol 1996; 25: 44-45.
20. Dearborn DG. Pulmonary
hemorrhage in infants and children. Curr Opin
Pediatric 1997; 9: 219-224.
21. Kabra SK, Bhargava S, Lodha
S, Satyavani A, Walia M. Idiopathic pulmonary
hemosiderosis: clinical profile and follow up of 26
children. Indian Pediatr 2007; 44: 333-338.
22. Yukset H, Yilmaz O, Saras R,
Kirmaz C, Sogut A, Ozalp S. Pulmonary hemosiderosis
with normocomplentemic urticarial vasculitis in a
child. Monaldi Arch Chest Dis 2007; 67: 63-67.
23. Godfrey S. Pulmonary
hemorrhage/ hemoptysis in children. Pediatric
Pulmonol 2004; 37: 476-484.
24. Baby NPS, Gahunia HK,
Massicotte P. Pulmonary thromboembolism in children.
Pediatric Radiol 2005; 35: 258-274.
25. Bousseta K, Siala N, Brini I,
Aloui N, Sammoud A, Hammou A, et al. The
hydatid of lung in children:54 cases. Tunis Med
2005; 83: 24-27.
26. Menon P, Rao KL, Saxena AK.
Duplication cyst of the stomach presenting as
hemoptysis. Eur J Pediatric Surg 2004; 14: 429-431.
27. Chan EY, Avcin T, Manson D,
Cutz E, Scneider R, Ratjen E. Massive hemoptysis in
a 11 year old girl with isolated pulmonary arteritis.
Pediatr Pulmonol 2007; 42: 177-180.
28. Martire B, Loizzi M, Cimmino
A, Perazzi S, De Mattin D, Giordano P. Catamenial
hemoptysis from endobronchial endometriosis in a
child with type I von Willebrand disease. Pediatr
Pulmonol 2007; 42: 386-388.
29. Baktari JB, Tashkin DP, Small
GW. Factitious hemoptysis: adding to the
differential diagnosis. Chest 1994; 105: 943-945.
30. Sood M, Clarke JR, Murphy MS.
Covert biting of buccal mucosa masquerading as
haemetemesis or hemoptysis in children. Acta
Paediatr 1999; 88: 1038-1040.
31. Tsao PC, Lin CY. Clinical
spectrum of bronchiectasis in children. Acta
Paediatr Taiwan 2002; 43: 271-275.
32. Miller JI. Rigid bronchoscopy.
Chest Surg Clin N Am 1996; 6: 161-167.
33. Sritippayawan S, Margetis MF,
Machaughlin EF, Achermann R, Wells WS, Davidson WSL.
Cor triatriatum: A cause of hemoptysis. Pediatr
Pulmonol 2002; 34: 405-408.
34. Sidman JD, Wheeler WB,
Cabalka AK, Soumekh B, Brovn CA, Wright GB.
Management of acute pulmonary hemorrhage in
children. Laryngoscope 2001; 111: 33-35.
35. Devine ST, Lippmann M.
Management of massive hemoptysis. In: Fein
AM, Kamholz S, Ost D, editors. Respiratory
Emengencies (Vol 2). London: Edward Arnold Publ;
2006. p. 325-338.
36. Bidwell JB, Pachner RW.
Hemoptysis: diagnosis and management. Am Fam
Physician 2005; 72: 1253-1260.
37. Mal H, Rullon I, Mellot F.
Immediate and long term results of bronchial artery
embolisation for life threatening hemoptysis. Chest
1999; 115: 996-1001.
38. Roebuck DJ, Barnacle AM.
Hemoptysis and bronchial artery embolisation in
children. Pediatr Resp Rev 2008; 9: 95-104.
39. del Gregario MA, Medrano J,
Mainar A, Alfonso ER, Rengol M. Endovascular
treatment of massive hemoptysis by bronchial artery
embolisation: Short-term and long-term follow up
over a 15 year period. Arch Bronchopneumol 2006; 42:
49-56.
40. Stebbings AE, Lim TK. Cause,
treatment and outcome of patients with life
threatening hemoptysis. Singapore Med J 1999; 40:
67-69.
41. Garzon AA, Gourin A. Surgical
management of massive hemoptysis. Ann Surg 1978;
187: 267-271.
42. Simrali M, Karasu S, Turut M, Gezer S, Kaya
S, Tastepe I, et al. Surgical management of
bronchiectasis in childhood. Eur J Cardiothorac Surg
2007; 31: 120-123.
|
|
|
 |
|

