|
|
|
Indian Pediatr 2009;46: 257-259 |
 |
Cardiac Mucormycosis with T-cell
Immunodeficiency |
|
S Shah, PV Suresh, S Maheshwari and *S Rao
From the Departments of Pediatric Cardiology and
Pediatric Cardiac Surgery*, Narayana Hrudayalaya, Bangalore, India.
Correspondence to: Dr Sejal Shah, Department of Pediatric
Cardiology, Narayana Hrudayalaya, No 258/A, Bommasandra Industrial Area,
Anekal Taluk, Bangalore 560 099, India.
E-mail:
[email protected]
Manuscript received: January 2, 2008;
Initial review completed: January 29, 2008;
Revision accepted: April 10, 2008.
|
|
Abstract
We present a case of a 2 year old apparently healthy
child who presented with fever and mass on the mitral valve. Excision
histopathology of the mass revealed mucormycosis. After 4 months, she
had CNS embolisation with recurrence of cardiac lesion when
investigations revealed associated T-cell immunodeficiency.
Keywords: Cardiac mucormycosis, Immunodeficiency,
Mitral valve, T-cell defect.
|
|
M
ucormycosis is a rare, progressive,
systemic necrotizing fungal infection rarely affecting a normal human
host. Most cases of cardiac mucormycosis described in literature have been
diagnosed on autopsies(1). We describe a case of cardiac mucormycosis in a
child with structurally normal heart who was also detected to have
immunodeficiency. This case illustrates the extensive nature of organ
involvement in mucormycosis and its resistance to available treatment.
Case Report
A 23-month old apparently healthy girl presented with a
one month history of high grade fever and one episode of abnormal
movements of left side of the body. On examination, she weighed 9.5kg, was
febrile and had tachycardia. All peripheral pulses were well felt.
Cardiovascular examination revealed normal heart sounds and a short
systolic murmur at the apex. Respiratory, abdominal and central nervous
system examination were normal. Hemoglobin was 10.4 g/dL, total count
7300/mm 3 (20% polymorphs and 76%
lymphocytes) and ESR 45mm/hour. Liver and renal function tests were
normal. Random blood sugar was 80 mg/dL and HIV serology was negative.
Urine routine microscopy revealed 6-8 RBCs/hpf. Chest X-ray and
electrocardiogram were normal. Echocardiogram revealed a large
peduncu-lated mass on the superior surface of anterior mitral leaflet with
an additional small mass on the superior surface of posterior mitral
leaflet and mild mitral regurgitation. Endocarditis and myxoma were
considered to be the likely possibilities. A day later, the child
underwent excision of the masses with mitral valve repair. During surgery,
small satellite lesions were noted on mitral valve chordae.
Histopatho-logical examination of the excised mass revealed it to be a
fungal vegetation consistent with mucormycosis. The blood and urine
cultures sent prior to surgery were negative. The child was treated with
parenteral amphotericin B (45 mg/kg cumulative dose) with close monitoring
of liver and renal function tests. She was discharged on oral fluconazole
(5 mg/kg/day) in an afebrile state. Echocardiogram at the time of
discharge did not reveal any vegetations.
The child was brought back four months later with
altered sensorium, generalized seizures, weakness of all four limbs and
inability to speak and swallow for 24 hours. On examination, she was
drowsy and had persistent focal seizures. The tone was increased in the
right lower limb with increased deep tendon reflexes. She had grade 2/5
power in left upper and lower limbs. Cardiovascular examination revealed a
systolic murmur at the apex with normal heart sounds. CT scan head showed
left basal ganglion and left parieto-occipital infarcts with old right
fronto-parietal infarcts. The right internal carotid artery was noted to
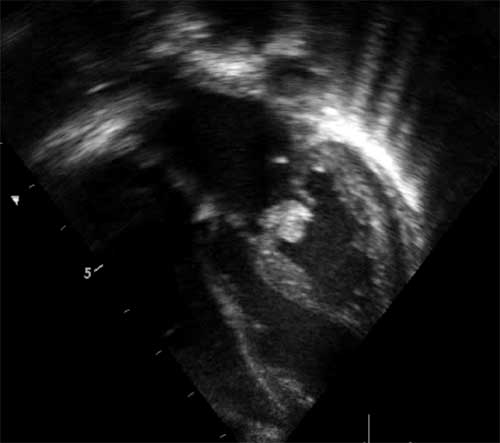
be blocked with thrombus on a CT angiogram. Echocardiography revealed
moderate mitral regurgitation with a 10 mm vegetation on the anterior
mitral leaflet (Fig. 1). Serial blood cultures grew
Candida–non albicans type. Lymphocyte enumeration study was done which
showed decreased CD3+/CD45+ (T-cells), CD3+/CD4+ (T-helper cells) and
absolute CD4+ lymphocyte count. Intravenous amphotericin B was restarted.
Oral fluconazole was continued. After four weeks of therapy the neurologic
status gradually improved, however left sided hemiplegia persisted. The
mitral regurgitation had worsened on echocardiography. After 12 weeks of
parenteral treatment, the child was discharged on oral antifungals.
 |
|
Fig.1 2D echocardiogram performed 4 months
after surgery showing a mass attached to anterior mitral leaflet
with respective chordae thickened in apical four chamber view. |
Discussion
Mucormycosis is an inclusive term for progressive
disseminated infections caused by phycomycetes, which are usually limited
in their virulence but can be highly invasive in certain conditions. The
most often affected sites are lungs, heart, liver, spleen and kidneys.
Dissemination has been most extensive in cases with endocardial
involvement(2). It can occur de novo(1,3,4)
or in association with cardiovascular surgery(5). Mucormycosis involving
native hearts have usually occurred in immunodeficient patients with few
exceptions(4). Hence, in this case, we were prompted to evaluate for
immunodeficiency. Our case is extremely rare as affliction by mucormycosis
of native heart valve in a two year old remains undescribed(3-7).
The major controversial issue in cardiac muco-mycosis
is treatment. Surgical excision followed by amphotericin appears to be the
most accepted strategy as described by Sanchez-Recalde, et al.(5).
Administration of antifungal therapy for atleast one week before surgery
is recommended to reduce the fungal burden whenever feasible. This is
followed by 5 weeks course of parenteral antifungals. Amphotericin B can
be ineffective in patients whose disease is detected late or who have
disseminated disease(8). Liposomal amphotericin B is considered as the
drug of choice as it allows high intra-macrophage concentration allowing
high concen-tration of the drug within the vegetation(9). Combination
therapy using lipid based amphotericin with an echinocandin or with an
azole (largely itraconazole or posaconazole) or with all three is
preferred(10). In our case, on
initial presentation, chances of embolisation from a pedunculated mass
prompted us for direct surgical intervention and the child did not receive
any preoperative antifungal coverage. Combined approach of surgical and 12
weeks of post operative amphotericin was not sufficient. On readmission,
medical treatment was thought to be the best possible therapy in view of
the disseminated nature and difficulty in demarcating the extent of
cardiac involvement.
Contributors: All authors were involved in patient
management. SS prepared the manuscript and reviewed the literature. PVS
and SM revised the article. SS will act as a guarantor.
Funding: None.
Competing interests: None stated.
References
1. Basti A, Taylor S, Tschopp M, Sztajzel J. Fatal
fulminant myocarditis caused by disseminated mucormycosis. Heart 2004; 90:
e60.
2. Scully RE, Mark EJ, McNeely WF, Ebelling SH, Philips
LD, Ellender SM. Weekly cliniciopatho-logical exercises. NEJM 1999; 341:
265-273.
3. Mehta NN, Romanelli J, St. John Sutton MG. Native
aortic valve vegetative endocarditis with cunninghamella. Eur J
Echocardiogr 2004; 5: 156-158.
4. Chandrasekar P, Rao SR, Raman ML, Vaidyanathan PR,
Muralidharan S. Mucormycosis of the heart presenting as paraparesis.
Indian Heart J 1998; 50: 75-76.
5. Sanchez-Recalde A, Merino JL, Dominquez F, Mate I,
Larrea JL, Sobrino JA. Successful treatment of prosthetic aortic valve
mucormysosis. Chest 1999; 116: 1818-1820.
6. Choudhry R, Venugopal P, Chopra P. Prosthetic mitral
valve mucormycosis caused by mucor species. Int J Cardiol 1987; 17;
333-335.
7. Callard GM, Wright CB, Wray RC, Minor GR. False
aneurysm due to mucor following repair of a coarctation with a dacron
prosthesis. J Thorac Cardiovasc Surg 1971; 61: 181-185.
8. Sugar AM. Agents of mucormycosis and related
species. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas
and Bennett’s Principles and Practice of Infectious Diseases. 5th ed.
Philadelphia: Churchill Livingstone; 2000. p. 2685-2695.
9. Ellis M. Amphotericin B preparations: a maximum
tolerated dose in severe fungal infections? Transpl Infect Dis 2000; 2:
51-61.
10. Spellberg B, Edwards J, Ibrahim A. Novel perspectives on
mucormycosis: Pathophysiology , presentation and management. Clin
Microbiol Rev 2005; 18: 556-569. |
|
|
 |
|

