Coronavirus disease (COVID-19) pandemic has
resulted in severe infection with thousands of deaths among the
elderly; however, very few pediatric cases need hospitalization
and/or intensive care.
A 7-year-old female (weight 17 kg), who was under
our follow-up for the last one year with a diagnosis of
cardiomyopathy and chronic lung disease (CLD), was admitted to
the emergency unit with the complaints of chest pain, dyspnea
and fatigue. She had
no fever, cough, vomiting, myalgia or gastrointestinal symptoms.
There was no exposure to a person infected with COVID-19 in her
family. The body temperature was 36.5 °C, heart rate was 110
beats/minute, respiration rate was 24/minute and blood pressure
was 90/60 mm/Hg on admission. She had bilateral rales, more
prominent on the right side, and grade II systolic murmur on
auscultation. The liver was 3-4 cm palpable below the right
lower costal margin. She had no peripheric edema and her
cutaneous oxygen saturation was 85%. The chest X-ray
showed infiltrations on the right middle and lower pulmonary
zones and massive cardiomegaly (Fig. 1).
Electrocardiogram showed sinus tachycardia and tall and wide P
waves, suggesting bi-atrial dilatation. Laboratory results were
normal except for raised white blood cell count (15500/mm3
with 80% neutrophils) and blood urea of 55 mg/dL. D-dimer
and troponin levels were slightly increased (0.85 mg/L and 0.3
ng/mL, respectively). The erytrocyte sedimantation rate and
C-reactive protein levels were normal.
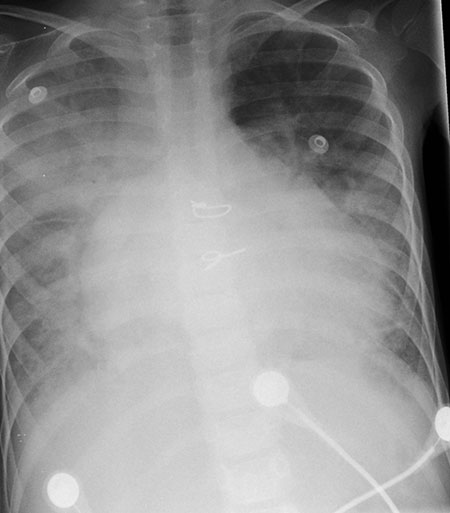 |
| Fig. 1 Chest X-ray
findings in a girl with COVID-19 infection and
pre-existing restrictive cardiomyopathy and chronic lung
disease. |
Echocardiography demonstrated restrictive
cardio-myopathy, mitral and tricuspid insufficiency and left
ventricular dysfunction (ejection fraction of 40%).
She had a history of using nasal continuous positive
airway pressure (CPAP) and oxygen concentrator due to the CLD
and oxygen desaturations (SpO2:80-85%). Her computed tomography (CT)
of the chest, performed two months ago, was compatible with the
pulmonary infiltration and CLD in the right lower and middle
lobes. The patient was hospitalized and treatment started with
inotropic support (milrinone, dopamine, furosemide infusion) and
nasal CPAP. Her fever spikes increased further and CRP and
neutrophil counts were also increased on the second day of
admission. After the blood, sputum and urine cultures were
obtained and the respiratory pathogen panel (RPP) was sent to
the laboratory, antibiotic therapy was initiated with vancomycin
and meropenem.
As COVID-19 infection was suspected due to her
progressive deterioration, a nasopharyngeal swab test was
obtained. The RPP and culture results were negative. The patient
showed rapid deterioration within a few hours on the third day.
Due to the acidosis, high lactate levels and hypercarbia on her
blood gase analysis, she was intubated and ventilated, but she
had a cardiac arrest. There was no response to the
cardiopulmonary resuscitation. The swab test result was positive
for COVID-19.
The common symptoms of COVID-19 reported in pediatric patients
can easily be misdiagnosed as the upper/lower respiratory tract
infections of pediatric age group [1,2]. In a series of 2135
children from China, 728 of which were positive for COVID-19,
55% were mild or asymptomatic, 40% were moderate (clinical or
radiographic evidence of pneumonia without hypoxemia), and 5%
were severe (dyspnea, central cyanosis) and <1% were critical
[3].
Diagnosis of COVID-19 have been based on the presence of at
least two symptoms (fever, cough, respiratory or
gastrointestinal findings or fatigue), combined with laboratory
tests (normal or low wbc count, low absolute lymphocyte count
and increased CRP) and an abnormal chest X-ray [4]. The
most commonly reported radiologic finding is bilateral
ground-glass opacity (32.7%) [5]. However, unlike adults, there
are no typical radiological findings for definitive diagnosis of
COVID-19 in children.
In one series, 23% of 345 children with laboratory-confirmed
COVID-19 one or more comorbidity. The most commonly reported
comorbid conditions were chronic pulmonary disease (including
moderate to severe asthma), cardiovascular disease and
immunosuppression [6]. Lu, et al. [5] reported that 3 out
of 171 pediatric patients with COVID-19 required intensive care
support and invasive mechanical ventilation; all with some
underlying conditions, and only a 10-month-old child with
intussuception died after 4 weeks of hospitalization [5].
Our case had no fever, no exposure to an infected person, but
had restrictive cardiomyopathy and chronic lung disease that
would suggest an exacerbation of her disease on admission.
COVID-19 infection was suspected due to her progressive
deterioration. We want to draw attention to such sub-acute
clinical presentations of COVID-19 in the pediatric population
with underlying comorbidities.
Published online:
April 30, 2020; PII: S09745591600170
Contributors:
AY: conception, design, drafting the manuscript; ATK:
final drafting and preparing the version of the manuscript to be
published.
Funding:
None; Competing interest: None stated.
REFERENCES
1.
Wang D, Hu B, Hu C, Zhu F,
Liu X, Zhang J, et al. Clinical characteristics of
138 hospitalized patients with 2019 novel coronavirus infected
pneumonia in Wuhan, China. JAMA. 2020; 323:1061-9.
2.
Qiu H, Wu J, Liang H, Yunling L, Song Q, Chen D. Clinical
and epidemiological features of 36 children with coronavirus
disease 2019 (COVID-19) in Zhejiang, China: An observational
cohort study. Lancet Infect Dis. 2020. Available from:
https://doi.org/10.1016/S1473-3099 (20)30198-5. Accessed
April 22, 2020.
3.
Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology
of COVID-19 among children in China. Pediatrics.
2020;145:e20200702.
4.
Ludvigsson JF. Systematic review of COVID-19 in children
shows milder cases and a beter prognosis than adults. Acta
Paediatrica. 2020. Available from:
https://doi.org/10.1111/apa.15270. Accessed April 22, 2020.
5.
Lu X, Zhang L, Du H, Zhang J, Li YY,
Qu J, et al. SARS-CoV-2 infection in children. N
Engl J Med. 2020;382:1663-5.
6.
Bialek S, Gierke R, Hughes M, McNamara LA, Pilishvili T,
Skoff T. Coronavirus disease 2019 in children- United States,
February 12–April 2, 2020. MMWR Morb Mortal Wkly
Rep. 2020;69:422-6.

