lash glucose monitoring system (FGM), a method of
glucose testing, is seen as hybrid between glucometers and continuous
glucose monitoring systems (CGMS) [1]. Consensus recommen-dations for
use of ambulatory glucose profile (AGP) in clinical practice have been
proposed [2]. The utility of FGM in children with poor glycemic control
and practical issues associated with FGM were analyzed in this study.
This observational study was done at the diabetic
clinic of Institute of Child Health and Hospital for Children from
October 2015 to June 2016. With ethical clearance and informed parental
consent, fifteen children aged 10-15 years with type 1 diabetes mellitus
of more than 2 years duration and with glycated hemoglobin (HbA1c) >10%
were included. Free Style Libre Pro (FSLP) FGM equipment was used. The
sensor was fitted in the posterior aspect of left arm and data was
captured at the end of 2 weeks. Finger prick blood glucose was performed
four times a day (thrice pre-meal and at 2 am). Sensor insertion,
glycemic variability, time in target range (TIR) and hypoglycaemia and
blood HbA1c were the study parameters.
Of the 15 sensors inserted, one got displaced on day
1 and one got stuck to the applicator. Insertion was successful in 13
(87%) children. Sensor was secured with additional plaster in all
children, yet 3 (20%) got displaced. Complete data were available in 10
(67%) children at the end of 2 weeks.
Mean (SD) age of children was 11.8 (1.14) years. The
median (IQR) of diabetes duration was 3 (2.75-5.75) years. The mean (SD)
of HbA1c was 11.14 (1.54%) and insulin requirement was 1.4 (0.38)
units/kg/day. The mean (SD) coefficient of variation as a measure of
glycemic variability was 46.29 (10). The mean (SD) inter quartile range
of glucose values was 161.3 (48.3) mg/dL. Average TIR was 27% while
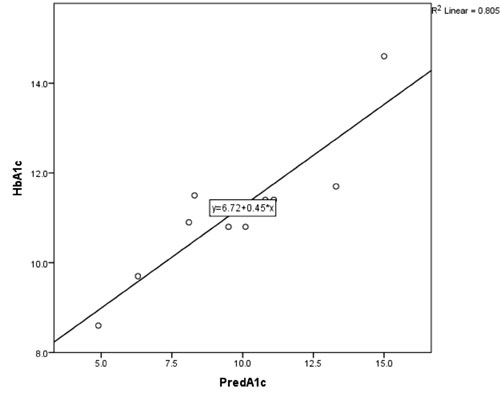
nearly 12% of time was spent in hypoglycemia. A good correlation between
HbA1c measured in blood and that predicted by FGM was observed
(correlation coefficient (r) = 0.81) as shown in Fig. 1.
 |
|
Fig. 1 Correlation between HbA1c
measured in blood (HbA1c) with predicted HbA1c (PredA1c) by
flash glucose monitor.
|
The study group showed high glycemic variability as
evidenced by high coefficient of variation and interquartile range [3].
Mean TIR was 27% which was similar to a previous study [4]. The goal of
70% of glucose values in target range which is termed as optimal
glycemic control is difficult to achieve even in those with lower HbA1c
as seen in that study. In addition, on an average 12% of time was spent
in hypoglycemia which is much higher than the desirable level of 5% [5].
Most of the hypoglycemia were nocturnal and asymptomatic. FGM is useful
in picking up asymptomatic nocturnal hypoglycemia.
The FSLP FGM sensor is small, light, painless to
insert and does not need recalibration [6]. Sensor insertion and
retention problems are common. Data on glycaemic variability, TIR, and
asymptomatic hypoglycaemia are useful for day to day management of
children with type I DM. Evidence shows that low cost, accurate data,
and data on demand are advantages of FGM, with lower mean absolute
difference throughout 14 days [7,8]. Diabetes management in children
involves glycemic variability, time in target range and other metrics,
beyond HbA1c, blood glucose and hypoglycaemia for a better control [9].
Contributors: SAN, PV, SS: conceptualized and
designed the study; SAN, RC: reviewed the literature; SAN, RVD, RC: data
acquisition: SAN: data analysis and manuscript preparation. All authors
were involved in revising it critically for intellectual content and
reviewing the manuscript version submitted.
Funding: The sensors and reader used in this
study, HbA1c measurements and glucometer strips for self-Monitoring of
blood glucose were funded by PUNCH (Pediatricians United for Child
Health) CHARITY, India.
Competing interests: None stated.
References
1. diaTribe. Making sense of Diabetes. The diaTribe
Foundation 2016. Available from: https://diatribe.org. Accessed
June 29, 2017.
2. Matthaei S. Assessing the value of ambulatory
glucose profile in clinical practice. Br J Diabetes Vasc Dis. 2014;
14:148-52.
3. Rodbard D. Continuous glucose monitoring: A review
of successes, challenges, and opportunities. Diabetes Technol Ther.
2016;18 (suppl 2):S3-13.
4. Distiller LA, Cranston I, Mazze R. First clinical
experience with freestyle libre pro flash glucose monitoring (FGM):
characterizing glycemic control with ambulatory glucose profile (AGP)
analysis in South Africa. J Diabetes Sci Technol. 2016;10:1294-1302.
5. Scheiner G. CGM retrospective data analysis.
Diabetes Technol Ther. 2016;18:14-22.
6. Garg SK, Akturk HK. Flash glucose monitoring: The
future Is here. Diabetes TechnoTher. 2017;19 (suppl 2):S1 -3.
7. Ólafsdóttir AF, Attvall S, Sandgren U, Dahlqvist
S, Pivodic A, Skrtic S, et al. A clinical trial of the accuracy
and treatment experience of the flash glucose monitor FreeStyle Libre in
adults with type 1 diabetes. Diabetes Technol Ther. 2017;19:164-72.
8. Hoss U, Budiman ES, Liu H, Christiansen
MP. Continuous glucose monitoring in the subcutaneous tissue over a
14-day sensor wear period. J Diabetes Sci Technol. 2013;7:1210-9.
9. Wright LAC, Hirsch IB. Metrics beyond hemoglobin A1c in diabetes
management: Time in range, hypoglycemia, and other parameters. Diabetes
Technol Ther. 2017;19 (suppl 2): S16-26.

