T
he limited access, insufficient availability,
sub-optimal or unknown quality of health services, and high
out-of-pocket expenditure (OOPE) are amongst the key health challenges
in India [1]. These challenges exist alongside a global discourse to
achieve universal health coverage (UHC) – increasing access to quality
healthcare services at affordable cost, by all people; and in times of
fast economic growth in India [2]. Though, India’s National health
policy-2017 (NHP-2017) is fully aligned with global discourse and has
the goal to achieve UHC, outside the policy discourses, health is often
not considered high on the priorities by political leadership and is
traditionally been underfunded [1,3,4]. The inappropriate mix of inputs
(infrastructure, human resources and supplies) results in a failure to
deliver the desired health services and public health system is grossly
underutilized by people. The elaborate government primary healthcare
system in rural India with nearly 185,000 facilities delivers only 8-10%
of total health services, availed by people. One-fourth of health
facilities in public sector deliver nearly three-fourths of total health
services delivered by entire public sector facilities. This means that
remaining 75% of health facilities are delivering much lower number of
services per facility than these are capable of [5]. People are either
compelled to, or prefer to, seek care from private providers, often at a
cost beyond their paying capacity. Health expenditure is estimated to
contribute to 3.6% and 2.9% of rural and urban poverty, respectively
[6]. Annually, an estimated 60 to 80 million people in India either
falls into poverty or get deeper into poverty (if already below poverty
line) due to health-related expenditures [1,7]. Clearly, the health
expenditures undermine poverty alleviation efforts by the union and
state governments in India (Box 1) [1,8-17]. India was
ranked at 154 of 195 countries on health service delivery index
published in mid-2017 in Lancet journal [18]. Though Indian healthcare
system has traditionally focused on delivery of maternal and child
health (MCH) services, and in spite of making rapid progress, the
country continues to have relatively high infant and maternal mortality
[19]. Access to even child health services is mostly through private
sector. Furthermore, people often have to spend from their pockets for
services such as child birth, even when availing services at public
health facilities [20,21].
|
Box 1 Key Health Challenges in India [1,8-17]
Health infrastructure and human resources:
There were 156,231 SHCs, 25,650 PHCs and 5,624 CHCs in India as
on 31st March 2017 [8]. However, most of these facilities suffer
from poor infrastructure, under-staffing and lack of equipment
and medicines. Only 11% of SHC, 16% of PHCs and 16% CHCs meet
the Indian Public Health Standards (IPHS) [5]. There is gross
shortage of specialists and general physicians in all levels of
system. More specifically, SHC, which are the first contact
point between community and government health system, one-fifth
were without regular water supply, one fourth without
electricity, one in every ten without all-weather road, and over
6,000 did not have an Auxiliary Nurse Midwife/health worker
(female) [8,10].
Health financing: The high out of pocket
expenditure (OOPE) on health at 62.6% of total health
expenditure is a major health challenge in India [11]. The OOPE
on health in India is one of the highest in the world and nearly
thrice of global average of 20.5% [8]. Part of the reason is
poor government spending on health, at 1.15% of gross domestic
product (GDP), which is one of the lowest in the world
[1,11,12].
Service Delivery and utilization: In
absence of well-functioning government facilities, people chose
private providers. Nearly 75% of all out-patient consultations
and 65% of all hospitalization in India happens in private
sector [13]. People in India are increasingly getting affected
by the health conditions which require regular visits to
out-patient consultation, preventive and promotive measures and
regular medications. The cost of such high volume and low-cost
interventions is major part of OOPE.
Quality of health services: There
is limited information available about quality of healthcare
services in India [14]. However, widespread presence of
unqualified providers, shortage of human resources, absentee
doctors, and studies on skills of qualified doctors indicates
toward poor quality of health services [14,15]. Regulation
is an approach to ensure quality; however, the clinical
establishment (registration and regulation) act 2010 has been
implemented by only a limited number of states in India [16].
Changing disease epidemiology: The
changing epidemiological profile of population is another
reality in India. In 2016, the non-communicable diseases were
major causes of morbidity and mortality in all Indian states
replacing the communicable diseases abundance [17].
|
In this background, when Ayushman Bharat
Program (ABP) was announced in India’s union budget 2018-19, it received
wide and unprecedented media, public and political attention [22-24].
This article reviews and documents the key health sector related
announcements in union budget 2018-19, critically analyzes the
components of the proposed program, and suggests a few strategies to
strengthen implementation and accelerate India’s journey towards UHC.
Health in Union Budget of India (2018-19)
The Government of India’s union budget, for the
financial year 2018-19, was presented to the parliament of India on 1st
February 2018 [22]. The Ministry of Health and Family Welfare received
an allocation of Rs. 54,800 Crore (approx. US $ 8.4 billion), an
increase of nearly 11.5 percent over the budget of last year. Though in
nominal terms, the budgetary allocation to health sector has trebled in
the last decade (Table I); as proportion of gross domestic
product (GDP), it has changed marginally from 1.1% to 1.3% [22-25].
TABLE I Budget Allocation to Health Sector in India 2008-09 to 2018-19 [22-24]
|
Financial |
Ministry/Department |
Total |
|
Year |
Health & |
Health
|
AYUSH* |
AIDS |
|
|
Family Welfare |
Research |
|
Control** |
|
|
2008-09 |
16968 |
531 |
623 |
- |
18123 |
|
2009-10 |
21113 |
606 |
922 |
- |
22641 |
|
2010-11 |
23530 |
660 |
964 |
- |
25154 |
|
2011-12 |
26897 |
771 |
1088 |
1700 |
30456 |
|
2012-13 |
30702 |
908 |
1178 |
1700 |
34488 |
|
2013-14 |
33278 |
1008 |
1259 |
1785 |
37330 |
|
2014-15 |
35163 |
1017 |
1272 |
1785 |
39237 |
|
2015-16 |
29653 |
1018 |
1214 |
1397 |
33282 |
|
2016-17 |
37061 |
1144 |
1326 |
- |
39533 |
|
2017-18 |
47352 |
1500 |
1428 |
- |
50281 |
|
2018-19 |
52800 |
1800 |
1626 |
- |
56226 |
All figures in Indian Rupee x Crores. The values are actuals
for 2008-09 till 2016-17 and budget estimates for year 2017-18
and 2018-19.
Remark: Fourteenth Finance Commission recommended the devolution
of 42% of total central revenue resources, which was implemented
starting FY 2015-16. This artificially resulted in reduced
allocation to centrally sponsored schemes in union budget.
* Ministry of AYUSH was created in 2015-16. The budget of the
Department of AYUSH is shown prior to these years; **Department
of AIDS Control (i.e., NACO) had a separate Demand for Grant in
Union Budget in the specified years |
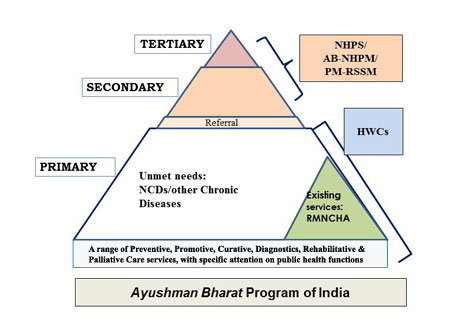
A key announcement in the union budget 2018-19 has
been the Ayushman Bharat Program (ABP). This program has two components:
(a) delivering comprehensive primary health care by establishing
150,000 health and wellness centers (HWCs) by year 2022, and (b)
Providing financial protection for secondary and tertiary level
hospitalization as part of National Health Protection Scheme (NHPS). The
ABP with two components intends to provide services with continuum
across three levels of care and brings back the attention on delivery of
entire range of preventive, promotive, curative, diagnostic,
rehabilitative and palliative care services (Fig. 1).
 |
|
NHPS: National Health protection Scheme;
AB-NHPM: Ayushman Bharat- National Health Protection Mission;
PM-RSSM: Pradhan Mantri- Rashtriya Swasthya Suraksha Mission;
HWCs: Health and Wellness Centres; RMNCHA: reproductive,
maternal, neonatal, child health and adolescent; NCDs: Non
communicable diseases
Fig. 1 Ayushman Bharat Program in
India.
|
One of the two initiatives in ABP is to upgrade
150,000 (of the existing 180,000) Sub health centers (SHCs) and Primary
health centers (PHCs) in India, to the HWCs by December 2022. The scope
of services from existing SHCs and PHCs is proposed to be broadened from
current range of services, and implements the national health programs
to a broad package of 12 services. This intends to make comprehensive
primary healthcare accessible by community within 30 min of walking
distance [1,5,22]. A total of 11,000 and 16,000 HWCs are proposed to be
made functional in financial years (FY) 2018-19 and 2019-20,
respectively [26]. This includes upgrading all 4,000 primary health
centers in urban area to the HWCs by March 2020.
The second initiative in ABP is NHPS (also known as
AB-NHPM or PM-RSSM), which has been referred as ‘the world’s largest
government-funded healthcare (insurance) program’ [22]. The NPHS aims to
provide a coverage of up to Indian Rs. 500,000 (or US$ 7,700) per family
per year for expenses related to secondary- and tertiary-level
hospitalization. The AB-NHPM, after the launch would subsume Rashtriya
Swasthya Bima Yojana (RSBY), and the Senior Citizen Health Insurance
Scheme (SCHIS) [27-29]. The RSBY was providing insurance coverage of Rs.
30,000 (US$ 470) for up to 5 members of a family per annum, for a target
beneficiary base of 60 million families. The target beneficiary in
AB-NHPM has increased to 107.4 million families, and estimated 535
million people, equivalent to ~40% of Indian population [22,27]. The key
health sector specific announcements in the union budget 2018-19 are
listed in Box 2. The key components and implementation
design of both HWCs and AB-NHPM/PM-RSSM are publically available and
summarized in Web Table I and
Web Fig. 1-3
[5,22,26,27]. The additional details on team at HWCs and on the
design structure of AB-NHPM/PM-RSSM are summarized in
Web Appendix
1 and 2, respectively [1,5, 22,26,27].
|
Box 2 Health in Union Budget 2018-19 of
India [22, 27]
• Ayushman Bharat Program received an
allocation of Rs 3,200 Crore (US$ 500 Million). This is for
union government share and state contributes remaining as per
agreed formula; therefore, total allocation would be in range of
Rs 5,000 Crore (US$ 770 Million) from state and union
government, combined.
• Cash assistance of Rs 500 (US$ 8) per
months for Tuberculosis patient for the duration of treatment
and this initiative has been allocated Rs 600 Crore (US$ 90
million).
• Twenty-four district hospitals to be
upgraded to medical colleges, to ensure at least 1 medical
college for every 3 parliamentary constituencies and at least 1
government medical college in each state of India.
• The existing 3% ‘education cess’ has been
changed to 4% ‘Health and education cess’. This would generate
additional revenue of Rs 11,000 crore (US$ 1.7 billion) during
the financial year.
• Initiative to control air pollution by
supporting the farmers in Haryana, Punjab, Uttar Pradesh and
National Capital region of Delhi for the in-situ disposal
of crop waste.
• Expansion of Ujjwala scheme (to provide
free ‘Liquefied Petroleum Gas’ connection to rural women) from
50 million to 80 million women in India. Allocation of Rs. 3,200
Crore (US$ 490 million).
• Continuation of Swachch Bharat Mission
(SBM) with target of building addition 20 million toilets.
Allocation to National Nutrition Mission has been doubled to Rs.
3,000 Crore (US$ 460 million).
• Increase of nearly 10% for Pradhan Mantri
Jan Aushadhi Yojana, Swachch Bharat Mission Rural and for
Anganwadi Services.
• The government’s proposal to private sector
and corporates to support the process of establishing HWCs could
be considered a far-reaching policy shift to engage and invite
private sector in strengthening primary healthcare in India.
• The social welfare surcharge of 10% to fund
social schemes and merger of three public sector insurance
companies would indirectly affect this program and health
sector.
• Higher Education Finance Agency (HEFA) to
be restructured to fund infrastructure and research in medical
institution as well. HEFA was announced in union budget 2017-18.
|
Prioritizing health and acknowledging linkage with
wealth
The union budget 2018-19 of India can be credited as
one of the most explicit political acknowledgement of linkage between
‘good health’ and ‘economic growth’. The Union Finance Minister in his
budget speech said: "Only ‘Swasth Bharat’ can be ‘Samridha Bharat’.
India cannot realize its demographic dividends without its citizen being
healthy.’ and ‘Ayushman Bharat Program will build a New India
2022 and ensure enhanced productivity, well-being and avert wage loss
and impoverishment. These Schemes will also generate lakhs of jobs,
particularly for women" [22]. Soon after union budget, the
health needs of the people of India occupied center stage of discussion,
by political leaders, media and people, and terms such as ‘universal
health coverage’ and ‘Ayushman Bharat Program’ were introduced in
the functional dictionary of general public [25,30,31] – something,
which has a potential to place health higher in future public and
political discourses in India.
In a shift, AB-NHPM has the beneficiaries beyond
traditional approach of targeting ‘below poverty line’ (BPL) population.
Inclusion of ‘vulnerable and deprived population’ identified through
Socioeconomic and Caste Census (SECC) will nearly double the number of
people to be benefited [22,27,32]. The benefits of HWCs, when fully
functional, would be available to 100% of population of the country.
Discussion
This was the first union budget of India since the
release of NHP-2017 in March 2017. This budget follows upon a few
strategies proposed in the NHP-2017, including suggestions to invest
two-third or more of government funding on the health on primary
healthcare, establishing health and wellness centers and introducing
‘strategic purchasing’ in healthcare, among other [1,22].
The ABP combines two initiatives, announced in past
as a single program. The NHPS was first announced in union budget of
2016-17, though with a coverage of Rs. 100,000 (US$ 1550) per family per
annum [23,24] and the HWCs were proposed by the task force on
strengthening primary healthcare in India in 2016 and first announced in
the union budget 2017-18 [5,23]. The ABP has strengths and limitations (Table
II), and potential to address select but key health challenges in
the country. Two initiatives in ABP together will meet the range of
healthcare needs across primary, secondary and tertiary care, appears
synergistic, and may help in increasing accessibility, availability,
appropriate care and affordability. This can help India progress towards
UHC.
|
TABLE II Ayushman Bharat program: SWOT
Analysis
|
|
Strengths
- Apparent shift from ‘disease specific’ and
‘Reproductive and child health’ focus of government initiatives
to comprehensive Primary healthcare
- Shift in targeting of social sector program
from ‘poor only’ to expanded approach of vulnerable and deprived
population (increased target beneficiaries significantly)
- Seemingly high level of political
commitment
- Acknowledgement of linkage between better
health and economic growth of India
Opportunities
- Alignment with the NHP 2017 and NITI
Aayog’s three year Action Agenda 2017-20.
- Wide public and media attention on the
program can bring desired public accountability to expedite
implementation
- Implementation experience from RSBY and
other schemes such as free medicines could be utilized for rapid
scale up
- Global and national level focus on
universal health coverage
- Upcoming general elections and assembly
elections in a number of states.
- Potential to develop innovative models and
strategies for strengthening entire healthcare system in India.
SWOT: Strengths, Weaknesses, Opportunities, Threats
|
Weaknesses
- HWCs are only a part of primary healthcare
system, requires broader strengthening of entire health system
- Limited attention and focus on reform of
broader health system
- Out-patient department visits, which
constitute a large part of out of pocket expenditure, not part
of PM-RSSM.
Threats
- Change in the political leadership or the
priorities of the elected governments (before or after
elections)
- Limited buy-in and interest by the Indian
states in PM-RSSM (both political and other reasons)
- Challenge in availability of mid-level care
providers for Health and Wellness centres could delay the
setting up of 150,000 HWCs
- Focus on these components only and the
other broader health system needs ignored.
- Disproportionate focus on one of two initiatives in ABP
|
The ABP as a program could be termed bold and
ambitious for both the initiatives. The financial coverage in AB-NHPM is
around 17-times more generous than RSBY, and two- to four-times more
generous when compared with the other states’ government-funded health
insurance schemes in India. NHPS/PM-RSSM targets almost twice the target
beneficiaries and thrice of actual numbers enrolled under RSBY in year
2016-17. Understandably, NHPS has received a lot of attention in India
and across the developing part of the world. However, arguably, the
proposal to set up 150,000 HWCs by 2022 is even bigger and potentially
more impactful initiative for the reasons listed here. One, the
comprehensive primary healthcare delivered through HWCs would benefit
entire 1.3 billion people of India across rural and urban setting.
Second, it would strengthen government primary healthcare system, which
caters to only 10% health needs of the people at present while a
well-functioning primary healthcare system has potential to cater up to
80-90% of health needs [33,34]. Third, strengthening primary healthcare
through HWCs can bring efficiency in health services through increased
access, gate keeping and a functional two-way referral system. Fourth
and importantly, the extended services in HWCs would cover a number of
non-communicable diseases (NCDs), and can tackle the epidemiological
transition. In 2016, the NCDs contributed to nearly two-third of all
mortality and 56% of preventable mortality in India [17].
There is sufficient evidence available that
strengthening of primary healthcare is the most appropriate approach to
achieve UHC. Investment on comprehensive primary healthcare system is a
practical and affordable solution for India [1]. Health services are
human resource intensive, and India has plenty of potentially trainable
human resources available at a low cost. The successful engagement of
nearly 1 million Accredited Social Health Activists (ASHA) under
National Health Mission (NHM) in India is a proof of the potential and
effectiveness of community health workers [35,36]. More of appropriately
skilled workforce such as mid-level healthcare providers (MLHP) as part
of HWCs would be affordable, efficient and effective. In the process,
India might end up building a low cost, high impact model of primary
healthcare, for rest of the world. Many countries such as Chile, Costa
Rica and Thailand have succeeded through their own context-specific
model for primary healthcare at low cost, and achieved comparable health
outcomes as to high-income countries.
The global evidence on effectiveness of government
funded and social health insurance (SHI) in reducing OOPE is limited,
either side [37,38]. However, there is enough evidence to conclude that
if implemented well and at-scale, insurance schemes increase access to
health services, can save lives, and improve financial affordability. It
is this emerging evidence and intention to make health services
affordable to poor people, that many state governments in India launched
publically funded health insurance schemes, mostly in the last decade (Table
III). There is evidence that such schemes can prove an effective
tool to improved quality of health services through differentiated rates
and incentives if providers meet certain quality standards, and have
accreditation; increased adherence to Standard Treatment Guidelines
(STGs), and provider’s willingness to accept slightly higher regulation,
amongst other approaches [39-41].
TABLE III Evolution of Health Insurance Schemes at National and State Levels in India
|
Year (of start/ launch) |
Name of the scheme
|
Scope
(National or state specific) |
|
1948 |
Employees’ State Insurance Scheme |
National |
|
1954 |
Central Government Health Scheme |
National |
|
1986 |
Private Insurance- Mediclaim |
National |
|
2003 |
Ex Servicemen Contributory Health Scheme |
National |
|
2003 |
Universal Health Insurance scheme (UHIS) |
National |
|
2003 |
Yeshasvini Cooperative Farmers Health Insurance, Vajpayee
Arogyashree Scheme (2010) , |
Karnataka |
|
Rajiv Arogya Bhagya (2013) |
|
|
2005 |
Health Insurance Scheme for handloom weavers |
National |
|
2006 |
Shilpi Swasthya Yojana for handicrafts artisan |
National |
|
2007 |
Aarogyasri scheme (continued as Dr NTR Vaidya Seva (2015)
Aarogya Raksha scheme, 2017 |
Andhra Pradesh
|
|
2007 |
Aarogyasri Health Scheme (Continuation in 2015) |
Telangana |
|
2008 |
Rashtriya Swasthya Bima Yojana (RSBY) |
National
|
|
2008 |
Comprehensive Health Insurance Scheme (CHIS) and CHIS Plus |
Kerala |
|
2008 |
Mizoram State Health Care Scheme |
Mizoram |
|
2009 |
Niramaya Health insurance schemeContinued as Swablamban Health
insurance schemes in 2016 |
National
|
|
2010 |
Rajiv Gandhi Jeevandayee Aarogya Yojana, Mahatma Jyotiba Phule
Jan Aarogya Yojana (2017) |
Maharashtra |
|
2012 |
Mukhya Mantri Amrutam YojanaMukhya Mantri Amtritam Vatsalya
(2014) |
Gujarat |
|
2012 |
Chief Minister’s Comprehensive Health Insurance Scheme |
Tamil Nadu |
|
2012 |
Megha Health Insurance Scheme, |
Meghalaya |
|
2012 |
Mukhyamantri Swasthya Bima Yojana |
Chhattisgarh |
|
2013 |
Biju Krushak Kalyan Yojana, |
Odisha
|
|
2013 |
Sanjeevani Swasthya Bima Yojana |
Dadra and Nagar Haveli, and Daman and Diu |
|
2014 |
The Arunachal Pradesh Chief Minister’s Universal Health
Insurance Scheme |
Arunachal Pradesh |
|
2015 |
Andaman and Nicobar Island Scheme for Health Insurance |
Andaman and Nicobar Island |
|
2015 |
Bhagat Puran Singh Health Insurance Scheme,Bhai Ghanhya Sehat
Sewa Scheme (BGSSS) |
Punjab |
|
2015 |
Bhamashah Health Insurance Scheme |
Rajasthan |
|
2016 |
Din Dayal Swasthya Seva Yojana
|
Goa |
|
2016 |
Senior Citizen Health Insurance Scheme (SCHIS) within RSBY |
National |
|
2016 |
Mukhya Mantri State Health Care Scheme (MMSHC) |
Himachal Pradesh
|
|
2016 |
Puducherry Medical Relief Society
|
Puducherry
|
|
2016 |
Mukhyamantri Swasthya Bima Yojana |
Uttarakhand |
|
2016 |
Atal Amrit Abhiyan |
Assam |
|
2016 |
Swasthya Sathi |
West Bengal |
|
2018 |
NHPS/AB- NHPM/PM-RSSM |
National |
|
This is an indicative list. For every state,
the year of start of first health insurance schemes has been
listed. A number of these schemes are for specific target
population groups. A number of Indian states have more than one
scheme; however, only a few key schemes are listed. There are a
few Indian states, with no insurance scheme. Most of the states
in India, in addition, have schemes with provision of
re-imbursement for medical expenses for selected health
condition and those schemes are not listed.
|
The insurance schemes in India have had low
population coverage (against the target beneficiaries) and limited
impact on OOPE. The coverage with insurance schemes in surveys have
ranged from 11-12% families in India [42] or that at least one member in
around 28% of Indian families [43]. Considering most of the insurance
schemes cover a narrow range of secondary- and tertiary-care procedures,
and exclude outpatient services; there seems to be a long way in
reducing OOPE in India. The cost of consultations in outpatient
department, along with cost of medicines and diagnostics are the major
contributor to the OOPE in India, which were not covered in either RSBY
earlier or PM-RSSM now. Understandably, health insurance schemes,
focused only on secondary and tertiary level hospitalization, do not
always lead to reduced OOPE. Rather in some cases, OOPE increases as the
awareness about schemes can lead to utilization of health services (by
the people who were not accessing services) and people have to pay for
additional services not covered [38,39,44]. The budgetary allocation to
RSBY during the years of implementation was less than one percent of
total annual government spending on health in India. Clearly, the impact
on OOPE could not have been much different. In the similar vein,
considering that total OOPE in India in 2014-15 was Rs 302,425 Crore
(Approx. US$ 46.5 billion) and a scheme such as PM-RSSM with an annual
budget of around Rs 12,000 Crore (or US$ 1.8 billion), even with full
scale implementation would have only marginal impact on reducing OOPE.
Though, it may prevent catastrophic health expenditures for the families
covered.
For health insurance schemes being effective and
efficient, a common and bigger pool, administered through a single
agency is considered the best approach. India has multiple schemes with
their independent and almost parallel administration, management and
beneficiaries. Even within a state, there are multiple scheme running
parallel, targeted at different beneficiaries. If PM-RSSM can initiate
the process of merger of multiple schemes in a single pool over period
of time and where non-poor join by paying the premium, that would make
it truly a ‘game changer’. In this context, the initiative by the
government of Karnataka to combine 7 ongoing and existing schemes in a
single pool, to be administered by a common agency, could be studied for
probable learnings [45]. At national level, a few schemes for financial
assistance to patients have been harmonized by union government by the
abolition of autonomous bodies and transfer to Ministry of Health &
Family Welfare [46]. Alongside, a road-map for the extension of benefit
of PM-RSSM to additional population, with graded subsidy, should be
actively considered and strategy outlined.
Many countries have included health as a basic right
in their constitution [47]. Evidence indicates that inclusion of health
as basic right help in increasing access to services and holding the
governments accountable. While India has adopted a number of right based
initiatives, including the ‘right to education’ legislation, the health
has not been mentioned as a right in the constitution of India, though
often interpreted in context of Article 21 on right to life [48].
India’s NHP-2017 takes a stride and proposes ‘progressively incremental
assurance’ towards health, though it falls short of ‘right to health’
[1]. The sustainability of select SHI in India over other schemes has
partially been attributed to legislative provisions [49]. A scheme of
magnitude of PM-RSSM might benefit from legislative backing as has been
case with Employee State Health Insurance Scheme (ESIS) and Central
Government Health Schemes (CGHS) [50, 51].
The National Health Services (NHS) of United Kingdom
is said have emerged from political commitment in aftermath of
post-World War II [52]. With ABP in India, there appears a political
will and commitment. The community and civil society plays a crucial
role in ensuring that political promises and commitments sustained in
changing political environment [52,53]. An institutional and legally
backed-up mechanism to engage communities and civil societies, such as
national health assembly in Thailand [54] may help India as well, though
the modus operandi could be home-grown.
In implementation of HWCs, caution has to be
exercised and an overzealous attempt to expand package of services
should not results in reduced attention on maternal and child health
(MCH) services. Rather, the MCH service platform should be used to build
upon expanded package of services. In addition, HWCs and financial
affordability offered through PM-RSSM would further increase
accessibility, affordability to all populations including mothers and
children and bring hitherto uncovered populations to the public health
system. HWCs can help in addressing different types of inequities in
health services, as identified by multiple surveys. There is evidence
that when geographical and financial access to services is increased, it
is poor and women who are more commonly benefited.
The people have to be at the center of health
services and in scale-up and reform of health services, attention should
not be on supply-side interventions only; people’s perspective should
get due consideration. Mechanisms for satisfaction survey and feedback
assessment should be strengthened, and the data used for regular actions
and initiatives.
Finally, there is a strong economic case for
accelerated implementation of ABP in India. Healthier population means
enhanced overall productivity, reduced wage loss and less
impoverishment. In Germany, domestic health economy contributes to 12%
of gross value added and 8% of Germany’s export [55]. The rapid
implementation of ABP in India has potential to generate employment
through recruitment of additional workforce such as MLHPs.
Implementation challenges in ABP and possible
solutions
The initiative under ABP can be called ambitious and
bold; however, would be operationally challenging for a health system,
not known to deliver. The sub-optimal implementation and partial
scale-up has been the case with a number of initiatives in the past
[27,56-60]. This includes initiatives started a few years ago (i.e.,
a number of free treatment and diagnostics schemes by union and state
governments) as well as NHPS announced in 2016 and the proposed
universalization of maternity benefit scheme, announced in December 2016
[61,62]. Clearly, in health sector, more need to be done for translating
policies and intentions into practice.
Health sector is a specialized field where successful
outcome requires getting both design and implementation right. In
setting up HWCs, a ‘rate limiting factor’ could be recruiting MLHPs or
Community Health Officer (CHO), one each would be required for 150,000
HWCs. This is an opportunity to innovate and explore solutions for
recruitment of additional cadre of providers on priority basis.
Alongside, the quality of services delivered through these facilities
needs to be assured by achieving Indian Public Health Standards (IPHS).
There is limited capacity amongst Indian states in
identification and enrolment of beneficiaries, designing the benefit
package, fixing the package rate, empanelment of facilities, monitoring
and regulation and fraud detection. Many of these are ‘sine qua non’ for
success of a health insurance scheme. The insurance schemes require a
state level authority with sufficiently trained staff, and a
well-functioning Information technology (IT) system to implement the
program. In India, the capacity of the states to run insurance schemes
is lowest where these are needed most. The success of PM-RSSM would also
be dependent upon how the supply-deficient Indian states such as Uttar
Pradesh, Bihar and the North-eastern states take up and implement the
scheme. A well-functioning IT platform would be essential to meet
diverse needs of different stakeholders including patients, service
providers and program managers [26,27]. The significance of IT
platform cannot be over-emphasized and it would be very crucial in
strategic purchase of services, provider payments, fraud detection and
monitoring of the scheme. India to utilize the opportunity provided by
PM-RSSM to build a strong IT platform not only for this scheme but also
to develop an integrated health information platform to bring multiple
IT systems on a single platform. The implementation would benefit from
generating real time data and then use of data for action. As a first
step, the data generated from RSBY should be analyzed and learnings used
for designing and scaling-up of PM-RSSM.
The ABP success on advancing health and achieving UHC
in India would be dependent upon the response and leadership of Indian
state. The states may require different model and design to address both
supply deficiency and capacity. A few additional suggestions to improve
implementation effectiveness of ABP are provided in Box 3.
|
Box 3 Actionable Steps for Improving
Implementation Effectiveness of Ayushman Bharat Program
For HWCs
• Conduct detailed costing exercise, agree on
roadmap, and allocate commensurate financial resources.
• Aggressive scale-up and not incremental
approach.
• Give attention to urban primary healthcare
and think of additional and innovative approaches with capital
investment in urban areas.
• Establish autonomous authority/corporations
to provide technical support for setting up HWCs.
• Information technology back-bone, and other
areas for intervention.
For AB-NHPM/ PM-RSSM
• Make insurance scheme easy to use for
people so that poor are able to use the services.
• Communicate the benefit plan and scheme to
target beneficiaries to ensure enrolment.
• A national level IT platform, to facilitate
beneficiary identification, portability, the payment and detect
fraud.
• Linkage of out-patient care with
specialized care to ensure efficiency and effectiveness in
health services.
• Strengthening of supply side is as important as demand
based financing schemes.
|
The way forward to strengthen health systems in India
As health seems to have received priority in India,
the opportunity should be used as a catalyst for decisive and broader
health system re-designing and strengthening. A few steps can contribute
to the implementation effectiveness:
1. Retain focus on increasing government
investment on health: In the years ahead, the universal
implementation of two components of ‘Ayushman Bharat Program’ would
require approx. Rs. 70-100 thousand Crore (US$ 11.5 - 15.5 billion)
per annum [63]. This increased investment in health would be in
alignment with NHP-2017 target of government spending 2.5% of GDP on
health by year 2025 [1]. This would require an annual increase of
20-25% in budgetary allocation by both national and state
governments. Not allocating enough funds to already underfunded
health sector, and only promise of providing funds as per the need,
can be taken as ‘perverse incentive’ by fiscally deficit governments
as a reason not to ramp-up implemen-tation. Measuring the government
investment on health as percentage of GDP is a better approach than
comparison by the nominal values or budget to budget estimates. The
ABP should not result in reduced attention from the targets of
NHP-2017. The UHC is about everyone, everywhere [64], and the
mechanisms for financial protection beyond targeted 40% families as
in PM-RSSM, should be explored and linkage between primary and
secondary/tertiary care strengthened. This should be part of
mid-term roadmap and ‘progressive universalization’ of financial
protection in India. Over the period of time, non-poor should be a
part of a government scheme. While premium for poor can be borne by
government, the non-poor can subscribe to an insurance scheme
(preferably, mandatory contribution).
2. Strengthen and scale up ongoing initiatives:
Strengthening a number of ongoing initiatives, i.e., free
medicines and diagnostics schemes, scaling up services in urban
areas, expansion of services for non-communicable diseases and
strengthening of the referral linkages at all levels of facilities,
are complementary and should continue to receive attention. Health
outcomes in selected urban areas are often worse than rural areas
and urban population faces additional challenges such as limited
public space for physical activities, air pollution, over-crowding
and migratory populations, which pose additional health risks
[59,65]. In urban set-up, converting the existing urban PHCs into
HWCs would not be enough and capital investment to expand PHC
infrastructure is also needed. A PHC and government medical officer
for every 50,000 population would not be able to cater the health
needs of urban population. An UPHC should be available for every
10-20,000 population. The initiatives such as ‘Mohalla Clinics and ‘Basthi
Devakhana’ should be actively considered for expansion in other
urban settings of India [66,67].
3. Establish institutional mechanism to bring
stakeholders together: Engagement with the community and
civil society organization will play a crucial role. This can bring
accountability and ensure continuity, rapid scale-up of the
initiatives, and can place health in electoral agenda. The academic
and research institutions as knowledge partners can help in
designing local solutions, while continue to derive learnings from
international experience and good practices in due course. The
success of ABP would also be dependent upon how best the proposed
initiatives in ABP are anchored on other flagship initiatives and
priority programs of government, such as Aspirational District
Program (ADP) and Gram Swaraj Abhiyan (GSA), launched around same
time [68,69]. In India, while there are a few mechanisms, i.e.,
Central Council of Health and Family Welfare, for limited
stakeholder of non governmental stakeholders. However, there is need
for more inclusive, dedicated and sustained institutional approach
are possible learnings from experience of national health assemblies
in Thailand [54].
4. State Government to take lead for advancing
UHC and explore the legal framework for PM-RSSM Achieving UHC in
India can be supported by examination of existing legislative
provisions and exploring additional ones to achieve stated policy
intentions. Sustainability and long-term continuity of social health
insurance schemes in India has been partially attributed to
legislative back up [48-51]. Similarly, hospitals and public health
is a state responsibility as per constitution of India. Therefore,
uptake of ABP is a lot dependent upon interest and leadership of
Indian states. In the long run, it might be helpful to explore the
pros and cons of bringing health in concurrent list of constitution
of India.
5. Use ABP as platform to bigger health system
reforms in India: The success of ABP would be in bringing
the shift from the traditional approach of disease specific and
targeted initiatives to focus on people-centered integrated services
and financial protection. One of the strengths and success factors
of National Health Mission (NHM) in India was attempt to strengthen
health system. The health system strengthening does not appear to be
an explicit focus in ABP in India. In due course, it would be
beneficial to converge the ABP and NHM to improve both supply- and
demand-side issues and achieve a stronger health system in all
states of country.
Conclusion
India has committed to achieve UHC as a signatory to
the globally agreed Sustainable Development Goals as well as through the
NHP 2017. For countries aiming to march towards UHC, there is no ‘one
size fit all’ solution, and the strategies have to be locally developed
and implemented. Every strategy/program would have to build upon
strengths and attempt to minimize limitations. Ayushman Bharat Program
appears to be a balanced approach, which combines provision of
comprehensive primary healthcare (through HWCs) and secondary and
tertiary care hospitalization (through PM-RSSM). While ABP would help
India make progress towards UHC, this program alone would not be enough
and needs to be supplemented by rapid scale-up and convergence of
ongoing schemes and programs, and taking a few additional measures. The
ABP can prove an initiative bigger than simply delivering health
services and rather a platform to prepare India for making health
coverage universal.
Funding: None; Competing interests: None
stated.
Disclaimer: Author is a staff member of World
Health Organization. The views and opinion expressed in this article are
personal and should and cannot be attributed to WHO or any other
organizations he has been affiliated in past or at present.
References
1. Government of India. National Health Policy 2017.
Ministry of Health and Family Welfare, Nirman Bhawan, New Delhi, 2017. p.
1-32.
2. World Health Organization. World Health Report
2010: Health Financing for Universal Coverage. Geneva: WHO, 2010.
3. [No author listed]. Health in India, 2017. Lancet.
2017;389:127.
4. Shiva Kumar AK, Chen LC, Choudhury M, Ganju S,
Mahajan V, Sinha A, et al. Financing health care for all:
challenges and opportunities. Lancet. 2011; 377:668-79.
5. Government of India. Report of the Task force on
Primary Health Care in India. Ministry of Health and Family Welfare,
Nirman Bhawan, New Delhi, 2017. p. 1-60.
6. Gupta I. Out of Pocket Expenditure and Poverty:
Estimates from 61 Rounds of NSS. Expert Group on Poverty. Planning
Commission, New Delhi; 2009. Available from:
http://planningcommission.gov.in/reports/genrep/indrani.pdf.
Accessed February 15, 2018.
7. World Health Organization and International Bank
for Reconstruction and Development / The World Bank. Tracking Universal
Health Coverage: 2017 Global Monito-ring Report. Available from:
http://www.who.int/health info/universal_health_coverage/report/2017_global_
monitoring_report.pdf. Accessed February 15, 2018.
8. Government of India. Rural Health Statistics 2017.
Ministry of Health and Family Welfare, Nirman Bhawan, New Delhi, 2017.
9. Government of India. Rural Health Statistics 2016.
Ministry of Health and Family Welfare, Nirman Bhawan, New Delhi, 2016.
10. Central Bureau of Health Intelligence. National
Health Profile 2017. Ministry of Health and Family Welfare, Nirman
Bhawan, New Delhi, 2017. p. 1-270.
11. National Health Systems Resource Centre. National
Health Accounts 2014-15. Ministry of Health and Family Welfare, Nirman
Bhawan, New Delhi, 2017. p 1-74.
12. World Health Organization. World Health
Statistics 2017: Geneva: WHO. 2017. Available from:
http://www.who.int/gho/publications/world_health_statistics/2017/en/.
Accessed Febuary 04, 2018.
13. National Sample Survey Organization. Report of
71st round of National Sample Survey 2014. Ministry of Planning,
statistic and implementation, New Delhi, 2017. Available from:
http://mospiold.nic.in/national_data_ bank/ndb-rpts-71.htm. Accessed
February 10, 2018.
14. Planning Commission, Government of India. Twelfth
Five Year Plan of India: Health Chapter. New Delhi, 2017. p. 1-60.
15. Das J, Holla A, Das V, Mohanan M, Tabak D, Chan
B. In urban and rural India, a standardized patient study showed low
levels of provider training and huge quality gaps. Health Aff
(Millwood). 2012;31:2774-84.
16. Government of India. The Clinical Establishment
(registration and regulation) Act, 2010. Ministry of Health and Family
Welfare, Nirman Bhawan, New Delhi. 2010.
17. Indian Council of Medical Research and Public
Health Foundation of India. State of Health in India, Nov 2017. Ministry
of Health and Family Welfare, Nirman Bhawan, New Delhi, 2017, p:1-32.
18. 2015 Healthcare Access and Quality Collaborators.
Healthcare Access and Quality Index based on mortality from causes
amenable to personal health care in 195 countries and territories,
1990-2015: A novel analysis from the Global Burden of Disease Study
2015. Lancet. 2017;390:231-66.
19. Government of India. Millennium development
Goals, India Country Report 2015. Minsitry of Statistics, Planning and
Implementation. Govt of India, New Delhi. 2016. Available from:
http://mospi.nic.in/sites/default/files/publication_reports/mdg_2july15_1.pdf.
Accessed March 03, 2018.
20. Deshmukh V, Lahariya C, Krishnamurthy S, Das MK,
Pandey RM, Arora NK. Taken to health care provider or not, under-five
children die of preventable causes: findings from cross-sectional survey
and social autopsy in rural India. Indian J Community Med.
2016;41:108-19.
21. Lahariya C, Dhawan J, Pandey RM, Chaturvedi S,
Deshmukh V, Dasgupta R, et al.; for INCLEN Program Evaluation
Network. Inter district variations in child health status and health
services delivery: lessons for health sector priority setting and
planning from a cross-sectional survey in rural India. Natl Med J India.
2012;25:137-41.
22. Government of India. India Budget 2018-19 and
Budget Speech. Ministry of Finance, New Delhi. Available from:
http://www.indiabudget.gov.in/. Accessed Febuary 12, 2018.
23. Government of India. Union Budget website for
previous years. Ministry of Finance, New Delhi. Available from:
http://www.indiabudget.gov.in/. Accessed February 12, 2018.
24. Lahariya C. Budget India 2008: What is new for
health sector. Indian Pediatr. 2008; 45:399-400.
25. BBC News. India unveils ‘world’s largest’ public
healthcare scheme. 1 February 2018. Available from:
http://www.bbc.com/news/world-asia-india-42899402. Accessed February
15, 2018.
26. Government of India. National Consultation on
Ayushman Bharat: Operationalizing Health and Wellness Centres to deliver
Comprehensive Primary Health Care. 1-2 May 2018; New Delhi.
27. Press Information Bureau. Cabinet approves
Ayushman Bharat – National Health Protection Mission. 21 March 2018; New
Delhi. Available from: http://pib.nic.in/newsite/PrintRelease.aspx?relid=177816.
Accessed February 15, 2018
28. Government of India. Rashtiya Swasthya Bima
Yojana. Ministry of Health and Family Welfare, Nirman Bhawan, New Delhi.
2014.
29. Highlights of union budget 2016-17. The Hindu,
New Delhi; 29 March 2016.
30. NITI Aayog comes to the Rescue as Health Ministry
Clueless on ‘World’s Largest Healthcare Programme. The Wire, 2018, Feb
03. New Delhi. Available from: https://thewire.in/220634/health-budget-2018-niti-aayog/.
Accessed February 15, 2018.
31. Through the looking glasses: The Readers’ Editor
writes: Scroll.in should take the lead in advocating primary healthcare
overhaul. Scroll; New Delhi;2018, Feb 26. Available from: https://scroll.in/article/869658/the-readers-editor-writes-scroll-in-should-take-lead-in-advocating-a-primary-healthcare-overhaul.
Accessed February 27, 2018.
32. Government of India. Socioeconomic and Caste
Census (SECC). Registrar General of Census Operations, New Delhi. 2012.
33. World Bank. Investing in Health: World
Development Report 1993. New York: Oxford University Press,1993.
34. Save the children. Primary Healthcare first.
London: Save The children Fund 2017; p. 1-4. Available from:
https://www.savethechildren.org.uk/what-we-do/policy-and-practice/our-featured-reports/primary-health-care-first
Accessed February 12, 2018.
35. Press Information Bureau. Evaluation of
Accredited Social Health Activist (ASHA). Government of India, 2015.
Available from: http://pib.nic.in/newsite/PrintRelease. aspx?relid=116029.
Accessed February 12, 2018.
36. Government of India. National Health Mission.
Ministry of Health and Family Welfare, Nirman Bhawan, New Delhi. 2005.
37. Karan A, Yip W, Mahal A. Extending health
insurance to the poor in India: An impact evaluation of Rashtriya
Swasthya Bima Yojana on out of pocket spending for healthcare. Soc Sci
Med. 2017;181:83-92.
38. Ghosh S, Gupta ND. Targeting and Effects of
Rashtriya Swasthya Bima Yojana on Access to Care and Financial
Protection. Econ Pol Weekly. 2017;52:32-40.
39. Sood N, Bendavid E, Mukherji A, Wagner Z, Nagpal
S, Mullen P. Government health insurance for people below poverty line
in India: Quasi-experimental evaluation of insurance and health
outcomes. BMJ. 2014;349:g5114.
40. Is National Health Protection scheme good public
policy? Mint (newspaper); New Delhi; March 12, 2018; p.12.
41. Morton M, Nagpal S, Sadanandan R, Bauhoff S.
India’s largest hospital insurance program faces challenges in using
claims data to measure quality. Health Aff (Millwood). 2016;35:1792-9.
42. Salve P, Yadavar S. Why India’s National Health
Insurance Scheme Has Failed Its Poor. India Spend, Mumbai; 17 October
2017. Available from:
http://www.indiaspend.com/cover-story/why-indias-national-health-insurance-scheme-has-failed-its-poor-49124.
Accessed February 15, 2018.
43. International Institute of Population Sciences.
National Family Health Survey - 4. National report. IIPS, Mumbai and ORC
Macro, 2017.
44. National Health Protection Scheme will not help
its intended beneficiaries. Mint; 2018, Feb 15; New Delhi. Available
from:
http://www.livemint.com/Opinion/k80NvWWKvFGwHptVIDIqNJ/National-Health-Protection-Scheme-will-not-help-its-intended.html.
Accessed February 15, 2018.
45. Karnataka to roll out Aadhaar-linked universal
health coverage on November 1. The New Indian Express; Bengaluru; 28
August 2017.
46. Press Information Bureau. Cabinet approves
rationalization of Autonomous Bodies under Department of Health & Family
Welfare. Government of India; New Delhi; 7 February 2018. Available
from: http://pib.nic.in/PressReleaseIframePage.aspx?PRID=1519860.
Accessed February 12, 2018.
47. Kurian OC. Financing public healthcare in India:
towards a common goal. Oxfam India: New Delhi, 2015. P. 1-18.
48. Reddy KS, Patel V, Jha P, Paul VK, Kumar AK,
Dandona L; Lancet India Group for Universal Healthcare. Towards
achievement of universal health care in India by 2020: A call to action.
Lancet. 2011;377:760-8.
49. Kaur H. Why Modi Must Seek Legal Backing for His
Ambitious Healthcare Project. Swarajya magazine; 27 April 2018.
Available from: Available from:
https://swarajyamag.com/ideas/what-are-the-arguments-for-having-a-modicare-law.
Accessed February 12, 2018.
50. Government of India. Employee State Health
Insurances Act, 1948.
51. Government of India. Central Government health
Insurance scheme, 1954
52. Webster C. The National Health Services: a
political history. Second edition. Oxford University Press. Oxford;
2002.
53. Hughes D, Leethongdee S. Universal coverage in
the land of smiles: Lessons from Thailand’s 30 Baht health reforms.
Health Aff (Millwood). 2007;26:999-1008.
54. Rasanathan K, Posayanonda T, Birmingham M,
Tangcharoensathien V. Innovation and participation for healthy public
policy: the first National Health Assembly in Thailand. Health
Expectations. 2012;15:87-96.
55. Kickbusch I, Franz C, Holzscheiter A, Hunger I,
Jahn A, Köhler C, et al. Germany’s expanding role in global
health. Lancet. 2017;390:898-912.
56. Press Information Bureau. Universal Health
Insurance Scheme (2003). PIB, Government of India. New Delhi. 2011.
Available from: http://pib.nic.in/newsite/Print Release.aspx?relid=78863.
Accessed February 12, 2018.
57. National Institute of Public Finance and Policy.
Report on Utilisation, Fund Flows and Public Financial Management under
the National Health Mission: A Study of Selected States, NIPFP; 2017.
58. Kapur A. Baisnab P. Budget brief: National health
Mission; Government of India, 2018-19. Accountability Initiative; Center
for Policy research, New Delhi. p. 1-8. Available from: http://accountabilityindia.in/budget/briefs/download/1814.
59. Lahariya C, Bhagwat S, Saksena P, Samuel R.
Strengthening urban health for advancing universal health coverage in
India. J Health Management. 2016;18:361-6.
60. Press Information Bureau. A new health protection
scheme to provide health cover up to Rs.1 lakh per family announced.
PIB, Government of India. New Delhi. Press release on 29 Feb 2016.
Available from: http://pib.nic.in/newsite/PrintRelease.aspx?relid=136989.
Accessed February 15, 2018.
61. Press Information Bureau. Cabinet approves pan-india
implementation of maternity benefit program. PIB, New Delhi, 17 March
2017. Available from: http://pib.nic.in/newsite/PrintRelease.aspx?relid=161857.
Accessed February 15, 2018.
62. Press Trust of India. Maternity benefit scheme
unlikely to get boost in Budget 2018. Times of India; New Delhi; 30 Jan
2018. Available from: https://timesofindia. indiatimes.com/business/india-business/maternity-benefit-scheme-unlikely-to-get-boost-in-budget-2018/articleshow/62712742.cms
Accessed February 15, 2018.
63. Lahariya C. Strengthening primary healthcare:
From promises to reality. Ideas for India; 27 March 2018. Available
from:
http://www.ideasforindia.in/topics/human-development/strengthening-primary-healthcare-from-promises-to-reality.html
. Accessed February 12, 2018.
64. World Health Organization. World Health Day 2018:
Universal health coverage: everyone, everywhere. Geneva: WHO; 2018.
Available from: http://www.who.int/campaigns/world-health-day/en/.
Accessed February 18, 2018.
65. Government of India. National Urban Health
Mission (NUHM): Framework for Implementation. Ministry of Health and
Family Welfare, Nirman Bhawan, New Delhi. 2013.
66. Lahariya C. Mohalla Clinics of Delhi, India:
Could these become platform to strengthen primary healthcare? J Family
Med Prim Care. 2017;6:1-10.
67. Lahariya C. Decongest hospitals with Mohalla
clinics. Deccan Herald; Bengaluru; 27 May 2017; Available from:
https://www.deccanherald.com/content/613762/decongest
-hospitals-mohalla-clinics.html. Accessed February 12, 2018.
68. Press Information Bureau. Transforming 115
backward districts across the country. Government of India. 23 Nov 2017;
New Delhi. Available from: http://pib.nic.in/newsite/PrintRelease.aspx?relid=173788.
Accessed February 12, 2018.
69. Press Information Bureau. Gram Swaraj Abhiyan
on Ambedkar Jayanti. Government of India. 6 April 2018; New Delhi.
Available from: http://pib.nic.in/newsite/PrintRelease.aspx?relid=178495.
Accessed February 12, 2018.

