December, 2015. The
invited experts included Pediatricians, Developmental Pediatricians,
Pediatric Neurologists, Psychiatrists, Remedial Educators and Clinical
Psychologists. The participants framed guidelines after extensive
discussions and review of literature. Thereafter, a committee was
established to review the points discussed in the meeting, and the
points of consensus on evaluation and management of ADHD are presented
herein.
Recommendations
ADHD is a disorder that manifests in early childhood.
The symptoms affect cognitive, academic, behavioral, emotional and
social functioning. ADHD is a chronic condition and children and
adolescents with ADHD are to be considered as children and youth with
special health care needs [5].
ADHD has a genetic and biochemical basis. Role of
environmental factors is uncertain; they may influence symptoms of ADHD
(sub-syndromic) rather than the syndrome of ADHD [5].
Developmental Screening
Parent and teacher-rated scales are recommended for
screening, which have been used globally as well as in studies conducted
in India to screen ADHD, followed by a formal diagnosis using the
Diagnostic and Statistical Manual of Mental Disorders (DSM). These
scales include the Conners Index Questionnaire, and the Vanderbilt ADHD
Diagnostic Teacher Rating Scale [6,7].
Core clinical features: Clinical sub-types
include: predominantly hyperactive-impulsive, predominantly inattentive
and combined ADHD.
Hyperactivity-Impulsivity (HI): Although
typically observed by 4 years of age, HI is increasingly being reported
in children with younger age of presentation of symptoms. HI increases
during the subsequent three to four years, peaks at seven to eight years
of age and declines thereafter. By adolescence, it is difficult to
identify HI, although the adolescent may feel restless or have
difficulties in settling down.
In contrast, impulsivity usually persists throughout
life and it is influenced by the child’s environment. Adolescents with
untreated ADHD and easy access to alcohol and substances of abuse are at
greater risk of substance abuse, than adolescents without ADHD [8].
Inattention: Children with predominantly
inattentive ADHD have limited ability to focus and they are slow in
cognitive processing and responding. Note that these symptoms are not
due to defiance or lack of comprehension [9]. Inattention is usually
identified late and not apparent until the child is 8-9 years of age.
Core symptoms must impair function in
academic, social, or occupational activities for a child to be diagnosed
with ADHD. Early diagnosis is essential to avoid further compromise of
functional achievement [5].
ADHD and Life-stage
Pre-school children: High activity level, poor
inhibitory control and short attention span are common even in typically
developing pre-school children. ADHD should be suspected in case of
increased precarious behaviors and physical injuries or unmanageable
behaviors across different settings. Combined type of ADHD is most
common in this group and persists in 60-80% of children in school-age.
Schoolchildren: School children have relatively
stable attention levels and experience decrease in hyperactivity.
However, 70% of these children have co- morbidities such as Oppositional
defiant disorder and Specific learning disorder. ADHD has a major impact
on peer and family interactions and academics, thereby influencing
parent’s reporting of presenting concerns.
Adults: At age 25 years; 15% individuals meet the
full criteria for ADHD and ~65% are in partial remission. Symptoms of
inattention persist more and show slower decline [14].
Co-morbidities: Following
co-morbidities have been identified with ADHD [5]: Oppositional Defiant
Disorder (ODD); Conduct disorders; Learning Disability; Anxiety
disorders; Intermittent explosive disorder; substance abuse disorder;
Antisocial disorder; obsessive compulsive disorder; tic disorder; Autism
spectrum disorder and major depressive disorder.
Diagnosis
The fifth edition of the Diagnostic and Statistical
Manual of Mental Disorders [5] is used to diagnose ADHD. It is to be
noted that diagnostic criteria (without subtyping) can be applied to
children as young as 4 years of age [11]. On the other hand, adolescents
may under-report core symptoms or functional impairment and may spend
too little time at home for parents to be accurate informants. Hence,
the pediatrician must obtain information from at least two
teachers and/or other adults with whom the adolescent interacts (e.g.,
counselor, coaches, etc) [11]. The diagnostic tools mentioned (i.e.
Child Behavior Check-List, Connors abbreviated rating scale and
Vanderbilt ADHD diagnostic parent rating scale) have not been validated
in the Indian population. The only freely available tool (based on
fourth edition of DSM) that can be used for diagnosis of ADHD in the
Indian context is the INCLEN Diagnostic Tool for ADHD (INDT-ADHD) [12].
The sensitivity, specificity, positive and negative predictive values
for the same are 87.7%, 97.2%, 98% and 83.3%, respectively. INDT-ADHD
has an internal consistency of 0.91 and a moderate convergent validity
with Conner’s Parents Rating Scale (r =0.73) [12]. The INCLEN tool is
available in English, Hindi, Odia, Konkani, Urdu, Khasi, Gujrati, Telgu
and Malayalam [12]. The time taken for its administration (excluding
scoring time), as observed in clinic-settings, is 15-30 minutes
(approx.).
Differential diagnosis: The symptoms of ADHD
overlap with a number of other conditions, including developmental
variations; neurologic or developmental conditions; emotional and
behavioral disorders; psychosocial or environmental factors, and medical
conditions [11,13-14]. Detailed history of the child and family,
examination, psychometric testing, laboratory investigations, and
genetic testing would help to establish the diagnosis. Few salient
conditions to be differentiated include hyperactive/inattentive
behaviors but within normal range for the child’s developmental level
and not impairing function, intellectual disability, learning
disability, autism, language or communication disorder, anxiety disorder
and motor incoordination disorder. Children with ADHD and with clinical
features of autism should also receive genetic testing to rule out
Fragile X syndrome. In areas that are known to be endemic for lead
toxicity, a blood lead examination is indicated. Children in cities are
at higher risk of lead toxicity due to vehicular traffic pollution and
in case of use of leaded petrol. An audiological examination should also
be conducted to rule out a hearing impairment.
Evaluation and Assessments
Any child 4 through 18 years of age, who presents
with academic or behavioral problems and symptoms of inattention,
hyperactivity, or impulsivity, should be evaluated [11]. Information
should be obtained from parents or guardians, teachers, and other school
and mental health clinicians involved in the child’s care. Comprehensive
evaluation for ADHD includes: a) Confirmation of core symptoms
for presence, persistence, pervasiveness and functional complications;
b) Exclusion of differential diagnoses; and, c) Identification of
co-existing emotional, behavioral and/ or medical disorders. Such a
comprehensive evaluation requires review of medical, social, and family
histories, clinical interviews with the parent and patient, and
information on functioning in school or day-care [11,15,16].
Medical evaluation: Important aspects of medical
history include prenatal exposures (tobacco, drugs, alcohol), perinatal
complications or infections, head trauma, central nervous system
infection, recurrent otitis media, history of sleep disturbances,
medications, family history of similar behaviors, and detailed child and
family cardiac history before initiating medications [11,16,17].
Physical examination: Physical examination is
normal in most children with ADHD. Vision and hearing assessments are
mandatory. It is essential to rule out differential diagnoses. Equally
important is to document the following at each visit: height, weight,
head circumference, and vital signs, assessment of dysmorphic features
and neuro-cutaneous abnormalities, a complete neurologic examination,
and observation of the child’s behavior in the clinic [18].
Developmental and behavioral evaluation: This
includes age of onset of core symptoms, their duration, settings in
which the symptoms occur, and degree of functional impairment or
functional impact of ADHD symptoms. Further information needed is
developmental milestones, especially language milestones, school
absences, psychosocial stressors, emotional, medical, and developmental
events that may provide an alternative explanation for the symptoms (i.e.,
different diagnostic conditions). Observation of parent-child
interactions in the office is an important component of assessment.
Information about core symptoms can be obtained
through open-ended questions or from ADHD-specific rating scales. The
pediatrician must document the presence of relevant behaviors from DSM-5
[16].
Educational evaluation: This includes completion
of an ADHD-specific rating scale; a detailed summary of classroom
behavior and interventions, learning patterns, and functional impairment
at school; evaluation of copies of report cards and samples of
schoolwork; and a review of school-based multidisciplinary evaluations
(if performed).
The teachers who provide the information should have
regular contact with the child for a minimum of four to six months, if
they are to comment reliably on the persistence of symptoms. If there
are discrepancies between parent and teacher reports, then information
should be obtained from professionals working in after-school programs
or other structured settings. Environmental factors (e.g., different
expectations, levels of structure, or behavior management strategies)
may be contributing to these symptoms [11].
Management
Children with ADHD, 4 to 18 years of age, without
co-morbid conditions can usually be managed by the primary pediatrician.
Completion of ADHD rating scales by parents and teachers during the
diagnostic evaluation helps to establish the presence of core symptoms
in multiple settings [19]. Modalities of management of ADHD include
behavioral interventions, medication and educational interventions
(alone or in combination). Since children with ADHD or its symptoms are
at an increased risk of intentional and unintentional injury, safety and
injury prevention should be discussed during each visit [5,11].
Table I summarizes behavioral and educational interventions.
TABLE I Behavioral and Educational Interventions
|
Type of intervention |
Components |
Age group |
|
Behavioral intervention |
a)Positive reinforcement; |
For children 4-6 years of age as
|
|
b)Time-out;
|
primary therapy and |
|
c)Response cost (withdrawing rewards/privileges
|
Children >6 years of age and
|
|
when problem behavior occurs) and
|
adolescents, as therapy in addition
|
|
d)Token economy (combination of positive reinforcement
|
to medication
|
|
and response cost) |
|
|
Educational intervention |
The classroom modifications and accommodations include |
Children 5 years and above;
|
|
1. Having assignments written on the board |
depends on the child’s capacity |
|
2. Sitting near the teacher |
|
|
3. Having extended time to complete tasks |
|
|
4. Being allowed to take tests in a less distracting environment |
|
|
5. Receiving a private signal from the teacher when the child
|
|
|
is ‘off-task’ |
|
|
6.Being assigned a ‘Study Buddy’ |
|
|
7.Being assigned a ‘Shadow Teacher’ |
|
The teacher may submit a report card at regular
intervals, which helps to monitor symptoms and the need for changes in
the treatment plan [24].
Age and choice of intervention
For children 4-6 years of age:
• Behavioral Intervention (BI), rather than
medication, is the initial therapy.
• Addition of medication is indicated if target
behaviors do not improve with BI and the child’s functioning
continues to be impaired.
• Methylphenidate is preferred rather than
amphetamines or Atomoxetine.
For children >6 years of age and adolescents [11,25]:
• Treatment with medication rather than BI alone
or no intervention.
• Stimulant drugs are the first line agents.
Non-stimulants are second line agents.
• BI should be added to medication therapy.
Adding behavioral/ psychological therapy to stimulant
therapy in school-aged children and adolescents does not provide
additional benefit for core symptoms of ADHD, but has an impact on:
• Symptoms of coexisting conditions (e.g.,
oppositional/ aggressive behavior)
• Educational performance
• Dose of stimulant therapy necessary to achieve
the desired effects.
Behavioral Interventions
Parent-child behavioral therapy is aimed at improving
parent-child relationships through enhanced parenting techniques.
Behavioral interventions are most effective if parents understand the
principles of behavior therapy (i.e., identification of
antecedents and altering the consequences of behavior) and the
techniques are consistently implemented [11,20-22]. Indications of
behavioral intervention include: (a) Initial intervention for
preschool children with ADHD (preferred to medication); (b)
Adjunct to medication for school-aged children and adolescents with
ADHD; (c) For children who have problems with inattention,
hyperactivity, or impulsivity but do not meet criteria for ADHD (sub-syndromic).
Specific interventions include: (a) Positive reinforcement; (b)
Time-out; (c) Response cost (withdrawing rewards/ privileges when
problem behavior occurs) and d) Token economy (combination of positive
reinforcement and response cost) [22]. Box 1 provides
useful strategies for parents and teachers to help children with ADHD
regulate their own behavior [11,23].
|
Box 1 Strategies for Parents and Teachers
to Regulate Behaviors in Children with ADHD
1. Maintaining a daily schedule (e.g.,
time table, post- its, reminders)
2. Using charts and checklists to help the
child stay ‘on task’
3. Keeping distractions to a minimum
4. Limiting choices
5. Providing specific and logical places for
the child to keep his school books, toys, and clothes
6. Setting small, reachable goals
7. Rewarding positive behavior (e.g.,
with a ‘token economy’)
8. Identifying unintentional reinforcement of
negative behaviors
9. Finding activities in which the child can
be successful (e.g., hobbies, sports)
10. Using calm discipline (e.g., time
out, distraction, removing the child from the situation)
|
Educational interventions
Children with ADHD may require changes in their
educational program, including (a) Provision of tutoring or
resource room support (either in a one-on-one setting or within the
classroom), (b) Classroom modifications, (c)
Accommodations, and (d) Behavioral interventions [11,23].
Pharmacologic Intervention
The drugs used for management of ADHD and their
side-effects are detailed in Tables II, III and IV.
The choice of medication depends on whether the child is in preschool in
which case a stimulant (Methylphenidate) may be given, if indicated. For
a school-aged child or adolescent, a stimulant is the first-line
agent, followed by amphetamines or a monoamine reuptake inhibitor i.e.,
Atomoxetine. Other medications (e.g., Alpha-2-adrenergic
agonists) usually are used when children respond poorly to a trial of
stimulants or Atomoxetine, or when children have unacceptable side
effects or significant coexisting conditions. The duration of action of
the recommended drug and the child’s ability to swallow pills also
influence the choice of medication.
TABLE II Medications for ADHD
|
Type of drug |
Name of the drug |
Dosage forms |
Duration of action |
Dosage |
Maximum dose |
|
Stimulant |
Methylphenidate |
5 mg, 10 mg and
|
3-5 hours |
Start with 5 mg/day for 1st day;
|
£25 kg: 35 mg;
|
|
|
20 mg tablets |
|
then 5 mg twice a day |
>25 kg:60 mg.
|
|
Stimulant |
Delayed onset
|
5 mg, 10 mg and |
3-8 hours
|
5 mg/day twice daily dosing;
|
£50 kg: 60 mg |
|
methylphenidate |
20 mg tablets |
|
increments of 20 mg per day,
|
>50 kg: 100 mg.
|
|
|
|
|
every 3-7 days |
|
|
Non-stimulant |
Atomoxetine |
10, 18 and 25 mg |
10-12 hours |
Start with 0.5 mg/kg per day |
100 mg per day or
|
|
|
|
|
for minimum 3 days and
|
1.4 mg/kg, |
|
|
|
|
increase to 1.2 mg/kg per day |
whichever is lesser
|
|
|
|
|
after at least 3 days |
|
TABLE III Side-effects of Stimulant Medications and Management
|
Side-effects |
Management |
|
Decreased appetite |
Counsel on high-protein, high-calorie diet and frequent snacks;
advise on medication after meals |
Tics
|
If distressing, taper or discontinue stimulant medication and
consider guanfacine ER or clonidine ER monotherapy or
augmentation |
|
Poor growth |
No action as ultimate adult height is not compromised |
|
Dizziness |
Self-resolving; symptomatic treatment |
|
Insomnia/nightmares |
Sleep hygiene; encourage natural sleep; melatonin as needed |
Mood lability
|
Look for direct effect of medication (emotional symptoms
correlate with expected time of medication effect) – if present,
discontinue medication; if rebound effect (emotional symptoms
occur later in day as medication expected to wearing off), then
add short-acting stimulant in afternoon |
|
Rebound symptoms
|
Add short-acting stimulant in afternoon; add slow-release
tablets
|
TABLE IV Side-effects of Non-stimulant Medications and Management
|
Side-effects |
Management |
|
Gastrointestinal distress |
Typically self-resolves; symptomatic care |
|
Headache |
Typically self-resolves; symptomatic care |
|
Sedation (drowsiness) |
Administer medication at bed-time |
|
Transient growth effects |
No action; adult height not affected |
|
Elevated blood pressure or heart rate |
No action if within age appropriate norms and asymptomatic |
|
Suicidal ideation, hepatotoxicity, priapism (rare) |
Counsel families on warning signs and symptoms of hepatotoxicity;
discontinue medication; re-evaluation of the child |
Stimulants are preferred to other medications because
stimulants have rapid onset of action, and a long record of safety and
efficacy. Individual differences in metabolism are more significant than
weight-based dosing of stimulant medications. The optimal regimen is
determined by changes in core symptoms and occurrence of side effects
[18,26].
Stimulant medications usually are started at the
lowest dose that produces an effect and increased gradually (e.g., every
3-7 days) until core symptoms improve by 40% - 50% compared with
baseline, or adverse effects become unacceptable. The frequency of
stimulant medication (i.e., both, times per day and days per week) is
based upon the type of ADHD and the functional domains in which
improvement is desired. Onset of action is very important in a
school-going child. At a therapeutic dose, the effects of stimulant
medications on core symptoms usually are apparent in 30-40 minutes after
administration and continue for the expected duration of action.
Appetite suppression may indicate treatment response. Inadequate dose
may be indicated by shorter than expected duration of action [18].
A child with the predominantly inattentive type of
ADHD may need medication only on school days. A child who has difficulty
with peer relationships may need medication every day. A child who
participates in after-school sports or activities on certain days of the
week may require longer-acting preparations or more frequent dosing on
those days. Optimal dose is the dose at which target outcomes are
achieved with minimal side effects.
Parents should be advised that 2-6 weeks of
medication maybe needed for any therapeutic effect to show and before
dose-reduction is considered. If side-effects are severe, the clinician
may decrease the dose of medication or change to another ADHD medication
(stimulant or non-stimulant) [27].
After several years of medication, children and
adolescents who have had stable improvement in ADHD symptoms and target
behaviors are offered a trial off, of medication to determine whether
medication is still necessary. If symptoms re-appear, after a period of
remission, consider the risk factors/stressors that have led to the same
and counsel parents on mitigating those; and resume medication. Children
with ADHD may require changes in their educational programming.
Combination therapy with medications and behavior/ psychological therapy
is superior to behavior/ psychological therapy alone and necessary for
restoration of function and inclusion.
Combination Therapy
Combination therapy uses both behavioral
interventions and medications. Combination therapy may be warranted in
preschool children who do not respond to behavioral interventions.
In a systematic review and a meta-analysis,
combination therapy with medications and behavior/psychological therapy,
was superior to behavior/ psychological therapy alone. Children
receiving combination therapy may require lower doses of medication and
achieve greater improvement in non-ADHD symptoms (e.g.,
oppositional/aggressive, internalizing, teacher-rated social skills,
parent-child relations and reading achievement) than children receiving
medication alone. Cognitive behavioral therapy may be a helpful adjunct
to medications for adolescents with ADHD. Dietary interventions are not
recommended.
Referral to a developmental pediatrician, child
neurologist or child psychiatrist is needed in case of Co-morbid
conditions (e.g., oppositional defiant disorder, conduct disorder,
substance abuse, emotional problems); b) Coexisting neurologic or
medical conditions (e.g., seizures, tics, autism spectrum disorder,
sleep disorder); c) La) Lack of response to a controlled trial of
stimulant or Atomoxetine therapy [25, 28-30].
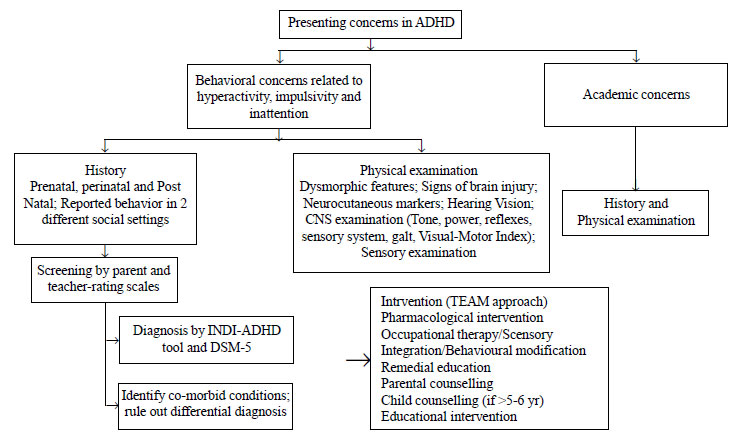
Fig.1 provides a flowchart for the management
of ADHD.
 |
|
Fig. 1 Flowchart for management of
ADHD.
|
Disability Certification
Government organizations, the Persons with Disability
Act (Equal Opportunities, Protection of Rights and Full
Participation),1995, and the National Trust for the Welfare of Persons
with Autism, Cerebral Palsy, Mental Retardation and Multiple
Disabilities act, 1999, do not recognize ADHD as a neurodevelopmental
disorder. Currently, there are no provisions for certifying children
with ADHD. However, the Rashtriya Bal Swasthya Karyakram (RBSK) focuses
on early detection and intervention of disease, disabilities,
deficiencies and developmental problems including ADHD. Owing to the
fact that it is the most common childhood neuro-behavioural disorder;
high prevalence rates in India, and the dire need for affected children
to receive sustained multidisciplinary interventions over a long period,
the expert group strongly recommends disability certification for ADHD.
Conclusion
ADHD is characterized by behavioral, emotional and
academic concerns, and requires a range of interventions such as
medications, behavioural intervention, occupational therapy/sensory
integration, remedial education, parent and child counselling and
classroom modifications. A comprehensive inter-disciplinary approach
leads to sustained alleviation of symptoms and greater capacity-building
of caregivers and children to adjust with the disease over the long
term.
1. Faraone SV, Sergeant J, Gillberg C, Biederman J.
The worldwide prevalence of ADHD: is it an American condition? World
Psychiatry. 2003;2:104-13.
2. American Psychiatric Association. Diagnostic and
statistical manual of mental disorders. 4th ed. Washington, DC: American
Psychiatric Association; 2000.
3. Venkata JA, Panicker AS. Prevalence of attention
deficit hyperactivity disorder in primary school children. Indian J
Psychiatry. 2013;55:338-42.
4. Duggal C, Dalwai S, Bopanna K, Datta V, Chatterjee
S, Mehta N. Childhood Developmental and Psychological Disorders: Trends
in Presentation and Interventions in a Multidisciplinary Child
Development Centre. Indian J Soc Work. 2014;75:495-522
5. American Psychiatric Association. Diagnostic and
statistical manual of mental disorders, 5th edition. Arlington, VA:
American Psychiatric Association; 2013.
6. Naik A, Patel S, Biswas DA. Prevalence of ADHD in
a rural Indian population. Innovative J Med and Health Science.
2016;6:45-6.
7. Suvarna BS, Kamath A. Prevalence of attention
deficit disorder among preschool age children. Nepal Med Coll J.
2009;11:1-4.
8. Levin FR, Kleber HD. Attention-deficit
hyperactivity disorder and substance abuse: relationships and
implications for treatment. Harv Rev Psychiatry. 1995;2: 246-58.
9. Weiler MD, Bernstein JH, Bellinger DC, Waber DP.
Processing speed in children with attention deficit/hyperactivity
disorder, inattentive type. Child Neuropsychol. 2000;6:218-34.
10. Faraone SV, Biederman J, Mick E. The
age-dependent decline of attention deficit hyperactivity disorder: a
meta-analysis of follow-up studies. Psychol Med. 2006; 36:159-65.
11. Subcommittee on Attention-Deficit/ Hyperactivity
Disorder, Steering Committee on Quality Improvement and Management.
ADHD: clinical practice guideline for the diagnosis, evaluation, and
treatment of attention-deficit/hyperactivity disorder in children and
adolescents. Pediatrics. 2011.
12. Mukherjee S, Aneja S, Russell PS, Gulati S,
Deshmukh V, Sagar R, et al. INCLEN diagnostic tool for attention
deficit hyperactivity disorder (INDT-ADHD): Development and validation.
Indian Paediatr. 2014;51:457-62.
13. Krull KR, Augustyn M, Torchia M. Attention
deficit hyperactivity disorder in children and adolescents: Clinical
features and evaluation. [cited 2012]. Available from:
http://www.uptodate.com/contents/attention-deficit-hyperactivity-disorder-in-children-and-adolescents-clinical-features-and-evaluation?source=search_
result&search=attention+deficit+hyperactivity+
disorder+children&selected Title=2~150. Accessed January 23, 2016.
14. Gilger JW, Pennington BF, DeFries JC. A twin
study of the etiology of comorbidity: attention-deficit hyperactivity
disorder and dyslexia. J Am Acad Child Adolesc Psychiatry.
1992;31:343-8.
15. National Collaborating Centre for Mental Health,
UK. Attention deficit hyperactivity disorder: diagnosis and management
of ADHD in children, young people and adults. [cited 2009]. Available
from:
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0034228/toc/?report=reader.
Accessed January 23, 2016.
16. Taylor E, Döpfner M, Sergeant J, Asherson P,
Banaschewski T, Buitelaar J, et al. European Clinical Guidelines
for Hyperkinetic Disorder–First Upgrade. Eur Child Adolesc Psychiatry.
2004;13:i7-i30.
17. Sedky K, Bennett DS, Carvalho KS. Attention
deficit hyperactivity disorder and sleep disordered breathing in
pediatric populations: a meta-analysis. Sleep Med Rev. 2014;18:349-56.
18. Wender EH. Managing stimulant medication for
attention-deficit/hyperactivity disorder. Pediatr Rev. 2001;23:234-6.
19. Collett BR, Ohan JL, Myers KM. Ten-year review of
rating scales. V: scales assessing attention-deficit/hyperactivity
disorder. J Am Acad Child Adolesc Psychiatry. 2003;42:1015-37.
20. Charach A, Carson P, Fox S, Ali MU, Beckett J,
Lim CG. Interventions for preschool children at high risk for ADHD: a
comparative effectiveness review. Pediatrics. 2013;131:1-21.
21. Kaplan A, Adesman A. Clinical diagnosis and
management of attention deficit hyperactivity disorder in preschool
children. Curr Opin Pediatr. 2011;23:684-92.
22. Floet AL, Scheiner C, Grossman L.
Attention-deficit/hyperactivity disorder. Paediatr Rev. 2010;31:56-69.
23. American Academy of Pediatrics. Understanding
ADHD. Information for parents about attention-deficit/hyperactivity
disorder. [cited 2001]. Available from:
http://www.pediatricenter.org/docs/ADHD%20AAP%20hand out_HE0169.pdf.
Accessed January 23, 2016.
24. Manansala MA, Dizon EI. Shadow teaching scheme
for children with autism and attention deficit-hyperactivity disorder in
regular schools. Educ Q. 2010;66:34-49.
25. Pliszka S. AACAP Work Group on Quality Issues.
Practice parameter for the Assessment and Treatment of Children and
Adolescents with Attention-deficit/hyperactivity Disorder. J Am Acad
Child Adolesc Psychiatry. 2007;46:894-921.
26. Kaplan G, Newcorn JH. Pharmacotherapy for child
and adolescent attention-deficit hyperactivity disorder. Paediatr Clin N
Am. 2011;58:99-120.
27. Southammakosane C, Schmitz K. Pediatric
psychopharma-cology for treatment of ADHD, depression, and anxiety.
Pediatrics. 2015;136:351-9.
28. The MTA Cooperative Group. Multimodal Treatment
Study of Children with ADHD. A 14-month randomized clinical trial of
treatment strategies for attention-deficit/hyperactivity disorder. Arch
Gen Psychiatry. 1999; 56:1073-86.
29. Brown RT, Amler RW, Freeman WS, Perrin JM, Stein
MT, Feldman HM, et al. American Academy of Paediatrics Committee
on Quality Improvement; American Academy of Paediatrics Subcommittee on
Attention-Deficit/Hyperactivity Disorder. Paediatrics.
2005;115:e749-e57.
30. Van der Oord S, Prins PJ, Oosterlaan J, Emmelkamp
PM. Efficacy of methylphenidate, psychosocial treatments and their
combination in school-aged children with ADHD: a meta-analysis. Clin
Psychol Rev. 2008;28:783-800.

