|
|
|
Indian Pediatr 2016;53: 485-495 |
 |
Cognitive
Functions and Psychological Problems in Children with Sickle
Cell Anemia
|
|
Gauthamen Rajendran, Padinharath Krishnakumar,
*Moosa Feroze and Veluthedath
Kuzhiyil Gireeshan
From Institute of Maternal and Child Health, and
*Department of Psychology; Government Medical College, Kozhikode, India.
Correspondence to: Dr Gauthamen Rajendran,
Clinical Fellow, Department of Neonatal Medicine, Women’s Center, John
Radcliffe Hospital, Oxford, United Kingdom, OX39DU.
Email: [email protected]
Received: September 02, 2015;
Initial review: October 23, 2015;
Accepted: March 08, 2016
|
Objective: To study the cognitive functions and psychological
problems in children with Sickle cell anemia (SCA).
Methods: Children with SCA were compared with an
age-, sex- and community- matched control group of children with no SCA.
Malin’s Intelligence Scale for Indian children, modified PGI memory
scale, and Childhood Psychopathology Measurement Schedule were used to
assess cognitive functions and psychological problems.
Results: Verbal quotient, performance quotient
and intelligence quotient in SCA group were 77, 81, 78, respectively
versus 92, 95, 93, respectively in non-SCA group (P <0.001).
Borderline intellectual functioning and mild mental retardation were
more common in SCA (70% and 16%, respectively). Children with SCA had
impaired attention, concentration and working memory and more behavior
problems compared to children without SCA.
Conclusions: Cognitive functions are impaired in
children with SCA and they have more psychological problems. Facilities
for early identification and remediation of psychological and
intellectual problems should be incorporated with health care services
for children with sickle cell anemia.
Keywords: Behavioral problems, Intellectual disability,
Memory, Psychopathology.
|
|
S
ickle cell anaemia (SCA) is the most common
inherited hematological disorder world-wide. It is estimated that about
18 to 34 % of the tribal population in the Wayanad district of Kerala,
India suffer from SCA [1,2].
Studies from abroad have reported neurocognitive and
developmental problems associated with SCA [3,4]. Very few authors have
studied the cognitive functions and psychological problems in children
with SCA in India [5].
The Government of Kerala provides comprehensive care
to children with SCA through monthly sickle cell anemia clinics
conducted in primary health centers in the district. The present study
aimed to assess the cognitive functions and psychological problems of
children with SCA attending the monthly clinics.
Methods
The study period was from February 2011 to July 2012
and the study protocol was approved by the Institutional ethics
committee of Government. Medical College, Kozhikode. Fifteen monthly SCA
clinics conducted in Wayanad, provide comprehensive healthcare to 276
children with SCA in the age group of 0-15 years. The study was
conducted in 8 of these SCA clinics. A total of 18 visits were required.
Children in the 6-15 year age group attending the SCA clinics, who were
already diagnosed to have SCA by hemoglobin electrophoresis or high
performance liquid chromatography were included in the study after
obtaining informed consent from their parents. Children with sickle cell
crisis, history of stroke, other chronic illnesses, and neurological
disorders were excluded.
Children with no SCA who were attending the same
primary health center for minor illnesses were included in the control
group. The children in the control group were screened negative for SCA
by clinical examination and solubility test. Children in the study group
and control group were matched for age, sex and community.
All children were evaluated using Malin’s
Intelligence Scale for Indian Children (MISIC), Childhood
Psychopathology Measurement Schedule (CPMS), and modified PGI Memory
Scale. The evaluation was done by a pediatric resident trained in the
use of the scales. Every child was allotted one hour, 25 minutes and 15
minutes for MISIC, PGI memory scale and CPMS tests, respectively and all
tests were done in a single sitting.
MISIC is the Indian adaptation of Wechsler’s
intelligence scale for children. It gives a verbal quotient (VQ),
performance quotient (PQ) and total quotient (IQ) [6]. CPMS is a
parent-reported rating scale for children of age 4 to 14 years [7]. CPMS
scale translated to the local language for the purpose of the study by
the investigators was given to the parent and each item in the scale was
explained to them to get the response.
The PGI memory scale contains 10 subtests and is
standardised for adults [8]. A modified version of PGI memory scale was
found to be applicable in Indian children [9]. In the present study,
three questions in remote memory subtest were modified to be applicable
to children and the modified questionnaire was tested in ten normal
children to check for their ability to answer the questions.
The data was entered in excel data sheet and analyzed
using the SPSS 10.0 software. Two-tailed paired t test was used to
assess the statistical significance and a P value of less than
0.05 was taken as statistically significant. Correlation of age with the
deterioration of cognitive functions of both cases and controls were
done using scatter plots of IQ.
Results
Fifty eight children with SCA in the age group of 6
-15 years attended the SCA clinics during the visits. Out of them, three
had seizure disorder, two had bronchial asthma, five refused to
participate in the study, and four opted out of the study because of the
time consuming intelligence tests. Thus, study and the control group
finally consisted of 44 children (25 boys and 19 girls) in the 6-15 year
age group. The mean age was 9.9 (2.67) years. All of them were receiving
comprehensive care for the last four years. Thirty two children (72.7%)
in each group belonged to Paniya community while 10 children (22.7%)
were from Kuruma community.
TABLE I MISIC Scores in Children With and Without Sickle Cell Anemia
|
Quotient |
Score (SD) |
Difference (SD) |
|
SCA |
Control |
|
|
Group |
Group |
|
|
Verbal Quotient |
77(6.7) |
92 (7.2) |
15 (6.7) |
|
Performance Quotient |
81 (7.5) |
95 (7.2) |
14 (7) |
|
Intelligence Quotient |
78 (7.5) |
93 (7.1) |
15 (6.4) |
|
P<0.001 for all comparisons; SCA: Sickle cell anemia. |
Children with SCA had lower IQ scores across all
subgroups in both verbal and performance domains (Table I)
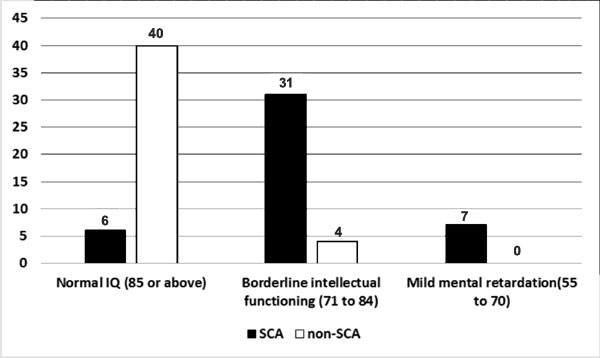
Children with both mild mental retardation and border intellectual
function were higher in the SCA group than non-SCA group (P<0.001) (Fig.
1). None of the children had moderate or severe mental retardation.
There was no statistical evidence to suggest deterioration of IQ with
advancing age in children with SCA.
 |
|
Fig. 1 Prevalence of
intellectual disability in children with and without Sickle-cell
anemia.
|
Mean raw scores of all the eight subtests in the PGI
memory scale, showed statistically significant difference (P
<0.05) between children with SCA and children in the control group (Table
II). The children in the study groups could not perform the delayed
recall and retention of dissimilar pair subtests of the PGI memory scale
and hence not included in the study.
TABLE II PGI Memory Scale Scores in Children With and Without Sickle Cell Anemia
|
Parameter |
Score (SD)
|
|
SCA Group |
Control Group |
|
Remote memory |
3 (1.3) |
4 (1.4) |
|
Recent memory |
1 (0.6) |
2 (1) |
|
Mental balance |
1 (0.4) |
2 (0.5) |
|
Attention and concentration |
6 (2.1) |
8 (1.6) |
|
Immediate recall |
1 (0.2) |
2 (0.5) |
|
retention of similar pairs |
2 (0.9) |
3 (0.8) |
|
Visual retention |
2 (0.8) |
3 (0.9) |
|
Recognition |
2 (0.9) |
3 (0.9) |
|
P<0.001 for all comparisons; SCA: Sickle cell anemia. |
Children in the study group and control group had
scores below the cut-off value of 10 on the CPMS scale, but there was
statistically significant difference between the mean score 4.09 (2.23)
vs. 2.43 (1.58), respectively. On analysis of the subscales of
CPMS, children in the SCA group scored significantly more on the
behavior problem subscale (P=0.002) and the difference was not
statistically significant on other items.
Even after applying ANCOVA (Analysis of co-variance)
there was statistically significant difference in the cognitive
functions (VQ, PQ and IQ) and CPMS score (P<0.05).
Discussion
The present study compared cognitive functions and
psychological problems in children with SCA with an age-, sex- and
community-matched control group of children with no SCA. It was found
that children with SCA had impaired cognitive functions and more
psychological problems compared to children in the control group.
Borderline intellectual functioning and mild mental retardation were
more commonly seen in children with SCA.
Our findings on cognitive functions in children with
SCA are comparable to the results of previous studies which have
reported lower IQ scores in children with SCA [10-12]. The causes of
cognitive impairment in SCA include brain infarction and chronic brain
hypoxia due to low hematocrit and thrombocytosis [11,12]. Since children
with history of stroke were excluded, silent infarcts and chronic brain
hypoxia may be the causes for cognitive impairment in the children in
the present sample.
Age related decline in cognitive functions has been
reported by several studies in the past [10]. In the present study no
correlation was observed between advancing age and cognitive decline.
This may be due to the fact that majority of children in our sample were
below 12 years, and also due to the small sample size.
A previous study from India found that children with
SCA have poor quality of life and all domains viz. physical,
psychological and cognitive domains are affected [5]. In the present
sample even though all children had scores below the cut-off value on
the CPMS, the scores were significantly higher compared to those of the
children in the control group indicating that children with SCA have
more psychological problems. Other studies have reported that
psychological disorders like anxiety and depression are more frequent in
children with SCA [13,14]. Gold, et al. [15] have reported that
even though children with SCA have no more behavior problems compared to
their siblings, they have more behavior problems compared to the general
population. In the present sample children with SCA differed
significantly on the behavior problem subscale of the CPMS. The reason
for this may be that psychological disorders commonly occur when the
children reach adolescence, and psychological distress in young children
most often present with externalizing behaviors.
The strengths of the present study include the fact
that study was conducted in a community-setting, the control group was
recruited from the same tribal community, and one-to-one matching was
done. Since the sample of children with SCA belonged to a tribal
population with unique social and cultural characteristics,
generalization of the result should be with caution. Small sample size
and lack of blinding while doing the tests are also limitations of the
study.
The present study emphasizes the importance of
assessment of cognitive functions and psychological well-being in
children with sickle cell anemia. Facility for early identification and
remediation of cognitive impairments and psychological problems should
be considered while planning health care services for children with
sickle cell anemia.
Acknowledgement: Professor Dr A Riyaz, Department
of Pediatrics, for his constant guidance and encouragement for the
completion of the study. Dr. Biju, Assistant Professor, Department of
Social and Preventive Medicine, for his supervision and guidance in the
analysis of the data.
Contributors: GR: conceptualized and designed the
study, designed data collection instruments, collected data, carried out
initial analyses, drafted the initial manuscript, and approved the final
manuscript as submitted; PK, MF, and VKG: carried out the further
analyses, reviewed and revised the manuscript, and approved the final
manuscript as submitted.
Funding: None; Competing interest: None
stated.
|
What This Study Adds?
• Children with sickle cell anemia have impaired cognitive
functions and more psychological problems compared to children
without sickle cell anemia.
|
References
1. Feroze M, Aravindan KP. Sickle cell disease in
Wayanad, Kerala: Gene frequencies and disease characteristics. Nat Med J
India. 2001;14:267.
2. Colah RB, Mukherjee MB, Martin S, Ghosh K. Sickle
cell disease in tribal populations in India. Indian J Med Res.
2015;141:509-15.
3. Armstrong FD, Elkin TD, Brown RC, Glass P, Rana
S, Casella JF, et al. Developmental function in toddlers with
sickle cell anemia. Pediatrics. 2013;131:406-14.
4. Glass P, Brennan T, Wang J, Luchtman-Jones L, Hsu
L, Bass CM, et al. Neurodevelopmental deficits among infants and
toddlers with sickle cell disease. J Dev Behav Pediatr. 2013;34:399-405.
5. Patel AB, Pathan HG. Quality of life in children
with sickle cell hemoglobinopathy. Indian J Pediatr. 2005;72:567-71.
6. Malin AJ. Manual for Malin’s Intelligence Scale
for Indian Children (MISIC). Lucknow: Indian Psychological Corporation,
1969.
7. Malhotra S, Varma VK, Verma SK, Malhotra A. A
childhood psychopathology measurement schedule: Development and
standardization. Indian J Psychiatr. 1988;30:325-32.
8. Prashad D, Wig NN. PGI memory scale (revised
manual) PGIMER, Chandigarh, National Psychological Corporation, 1988.
9. NS Gajre, Fernandez S, Balakrishna N, Vazir
S. Breakfast eating habit and its influence on attention-concentration,
immediate memory and school achievements. Indian Pediatr. 2008;45:824-8.
10. Steen RG, Fineberg-Buchner C, Hankins G, Weiss
L, Prifitera A, Mulhern RK. Cognitive deficits in children with sickle
cell disease. J Child Neurol. 2005;20:102-7.
11. Steen RG, Miles MA, Helton KJ, Strawn S, Wang W, Xiong
X, et al. Cognitive impairment in children with hemoglobin SS
sickle cell disease: relationship to MR imaging findings and hematocrit.
AJNR Am J Neuroradiol. 2003;24:382-9.
12. Hogan AM, Pit-ten Cate IM, Vargha-Khadem F, Prengler
M, Kirkham FJ. Physiological correlates of intellectual function in
children with sickle cell disease: hypoxaemia, hyperaemia and brain
infarction. Dev Sci. 2006;9:379-87.
13. Schatz J, Roberts CW. Neurobehavioral impact
of sickle cell disease in early childhood. J Int Neuropsychol
Soc. 2007;13:933-43.
14. Unal S, Toros F, Kütük MÖ, Uyanýker MG.
Evaluation of the psychological problems in children with sickle cell
anemia and their families. Pediatr Hematol Oncol. 2011;28:321-8.
15. Gold JI, Mahrer NE, Treadwell M, Weissman L,
Vichinsky E. Psychosocial and behavioral outcomes in children with
sickle cell disease and their healthy siblings. J Behav Med. 2008;
31:506-16.
|
|
|
 |
|

