|
|
|
Indian Pediatr 2015;52:
477-480 |
 |
Blood N-terminal Pro-brain Natriuretic
Peptide and Interleukin-17 for Distinguishing Incomplete
Kawasaki Disease from Infectious Diseases
|
|
Ling Wu, Yuanling Chen, Shiling Zhong, Yunyan Li,
Xiahua Dai and Yazhen Di
From Department of Pediatric Rheumatoid Immunology,
Ningbo Women and Childrenís Hospital, Zhejiang, China.
Correspondence to Dr Yazhen Di, Department of
Pediatric Rheumatoid Immunity Ningbo Women and Childrenís Hospital, 339
Liuting Street, Ningbo, Zhejiang 315012, China.
Email: [email protected]
Received: September 23, 2014;
Initial review: December 15, 2014;
Accepted: March 11, 2015.
|
Objective: To explore the
diagnostic value of blood N-terminal pro-brain natriuretic peptide (NT-proBNP)
and interleukin-17(IL-17) for incomplete Kawasaki disease.
Methods: Patients with Kawasaki disease,
Incomplete Kawasaki disease and unclear infectious fever were included
in this retrospective study. Their clinical features, and laboratory
test results of blood NT-proBNP and IL-17 were collected and compared.
Results: 766 patients with complete clinical
information were recruited, consisting of 291 cases of Kawasaki disease,
74 cases of incomplete Kawasaki disease, and 401 cases of unclear
infectious diseases. When the consistency with indicator 2 and 3 in
Kawasaki disease diagnosis criteria was assessed with blood IL-17
≥11.55
pg/mL and blood NT-proBNP ≥
225.5 pg/dL as the criteria, the sensitivity
and specificity for distinguishing incomplete Kawasaki disease and
infectious diseases reached 86.5% and 94.8%, respectively. When we chose
the consistency with indicator 1 and 2 in Kawasaki disease diagnosis
criteria, the appearance of decrustation and/or the BCG erythema, blood
IL-17 ≥11.55
pg/mL and blood NT-Pro BNP ≥225.5
pg/dL as the criteria, the sensitivity and specificity for
distinguishing incomplete Kawasaki disease and infectious diseases was
43.2% and 100%, respectively.
Conclusion: Blood NT-proBNP and IL-17 are useful
laboratory indicators for distinguishing incomplete Kawasaki disease and
infectious diseases at the early stage.
Keywords: Biomarker, Diagnosis, Kawasaki disease, Vasculitis
|
|
K
awasaki disease is an acute and immune vascular
inflammatory disease with unknown etiology. Incomplete Kawasaki disease
has less typical clinical features than the complete type, but it
presents much higher incidence of coronary artery lesion [1].
Intravenous immunoglobulin (IVIG) can effectively prevent coronary
artery lesions of incomplete Kawasaki disease, but the timing of
treatment is very important for its efficacy [2]. Therefore, early
diagnosis and treatment is of great significance for incomplete Kawasaki
disease. However, the diagnosis of incomplete Kawasaki disease is often
delayed due to the lack of typical clinical features and the shortage of
specific laboratory diagnostic indicators for the early stage of
disease. In the present study, we investigated the clinical features and
laboratory indicators in patients with Kawasaki disease, incomplete
Kawasaki disease and unknown infectious fever, and studied whether blood
N-terminal pro-brain natriuretic peptide (NT-pro BNP) and interleukin-17
(IL-17) could have a diagnostic value for distinguishing incomplete
Kawasaki disease and infectious diseases at the early stage.
Methods
The criteria for the selection of research subjects
included: age £5
years; diagnosed as Kawasaki disease, or incomplete Kawasaki disease, or
with fever for ≥3
days with unknown reasons when hospitalized; complete clinical data;
confirmed diagnosis when discharged; excluding other non-infectious
diseases and implicit diagnosis ultimately; and hospitalized between
October 2008 and September 2012. Kawasaki disease was diagnosed as per
standard criteria [3]. The infection diagnosis criteria referred to the
guidelines formulated by the infectious diseases working party of the
German Society of Hematology and Oncology [4]. The research was approved
by the hospitalís Ethnical Committee, and informed consent obtained from
custodians of all participants.
Data collected included: fever persisting 3-7 days,
polymorphous exanthema, conjunctival congestion (no photophobia and no
secretions), changes of lips and oral cavity, acute cervical
lymphadenopathy (non-purulent, unilateral, diameter >1.5 cm), changes of
peripheral extremities: (reddening and indurative edema of palms and
soles at the initial stage, and membranous desquamation from fingertips
at the recovery phase), decrustation, and BCG erythema. Blood samples of
all patients were drawn at the acute stage and on the day of admission
(3-7 days after the onset, no high dose of intravenous gamma globulin
and aspirin therapy). Laboratory tests included NT-proBNP, IL-17,
C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR). The
level of blood NT-proBNP was quantified using an automated enzyme-linked
fluorescence analyzer (Biomerieux Sa Company, mini-VIDAS, France) and
the matched NT-proBNP reagent. The level of IL-17 was detected by
enzyme-linked immunosorbent assay (ELISA) using the IL-17 ELISA Kit (R&D
System, Minneapolis, USA).
SPSS 13.0 software was used for all data analyses.
The normally distributed measurement data were analyzed with one-way
ANOVA and LSD tests. The count data were analyzed with Fisherís exact
test or chi-square test. P<0.05 was considered as statistically
significant. The value of NT-proBNP was transformed into Napierian
logarithm to approach the normal distribution. The resultant average and
standard deviation of NT-proBNP were then converted back to their actual
values by antilogarithm. Additionally, ROC curve analysis was performed
on the single factor of statistical significance and the meaningful
clinical features and laboratory indicators were further analyzed to
obtain the optimal critical value of incomplete Kawasaki disease
identification and diagnosis.
Results
A total of 766 children (291 with Kawasaki disease
and 74 with Incomplete Kawasaki disease) were recruited. 401 children
had other infectious diseases. 166 of the Kawasaki disease patients were
boys and the mean (SD) age were 2.0 (0.9) (Table I). About
60% of Kawasaki disease was associated with comorbid infections in this
study. The infectious disease patients included 208 cases of respiratory
infection (in particular, 109 cases were with lower respiratory
infection), 21 cases of digestive tract infection, 31 cases of urinary
tract infection, 39 cases of the central nerve system infection, 27
cases of infectious mononucleosis syndrome, 15 cases of lymphadenitis,
and 60 cases of sepsis.
The levels of blood NT-probing, IL-17, CRP and ESR
were very similar in Kawasaki disease and incomplete Kawasaki disease
groups, but all were significantly lower in infectious group (P<0.05,
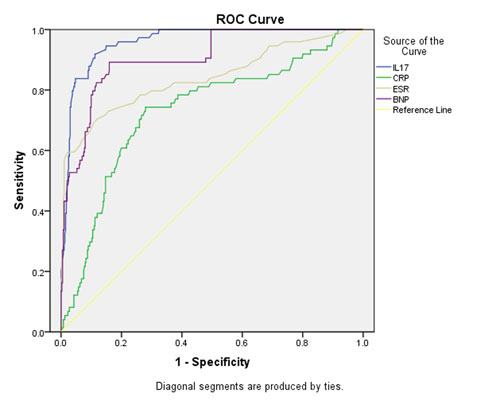
Table I).The areas below the ROC curves of the levels of
blood NT-proBNP and IL-17 were respectively 0.906 and 0.960 (Table
II and Fig. 1). The diagnostic cut-off of blood NT-proBNP
blood IL-17, blood CRP (DCP) and ESR, and the corresponding sensitivity
and specificity for identifying incomplete Kawasaki disease and
infectious diseases is shown in Fig. 1.
TABLE I Comparison of Baseline and Laboratory Parameters Among Children with Kawasaki Disease,
Incomplete Kawasaki Disease and Other Infections
|
Parameter |
Kawasaki |
Incomplete |
Infectious
|
|
disease |
Kawasaki |
diseases
|
|
(n= 291) |
disease |
(n= 401) |
|
|
(n= 74) |
|
|
Age (y) |
2.0 (0.9) |
1.9 (0.9) |
2.2 (1.1) |
|
Gender (male), n (%) |
166 (57.0) |
41 (55.4) |
223 (55.6) |
|
NT-proBNP (pg/dL) |
802.5 (4.5) |
900.4 (3.8) |
121.0 (2.5)*# |
|
IL-17 (pg/mL) |
35.4 (13.5) |
33.8 (15.5) |
7.7 (7.2)*# |
|
CRP (mg/L) |
68.7 (51.4) |
63.5 (41.9) |
35.9 (33.2)*# |
|
ESR (mm/h) |
59.8 (31.1) |
61.4 (31.4) |
27.8 (14.2)*# |
|
*Compared with Kawasaki disease group P<0.05; #Compared with
Incomplete Kawasaki disease group P<0.05; All values in mean
(SD). |
TABLE II Diagnostic Values of Blood NT-proBNP, IL-17, CRP and ESR in Distinguishing Incomplete
Kawasaki Disease and Infectious Diseases
|
Parameter |
Diagnostic |
Sensitivity |
Specificity |
Area-under |
P
|
|
cut-off |
(%) |
(%) |
the curve |
|
|
NT-proBNP (pg/dL) |
≥ 225.5 |
89.2 |
84.0 |
0.906 |
<0.001 |
|
IL-17 (pg/mL) |
≥ 11.55 |
91.9 |
88.8 |
0.960 |
<0.001 |
|
CRP (mg/L) |
≥ 38.05 |
74.3 |
72.1 |
0.731 |
<0.001 |
|
ESR (mm/h) |
≥ 44.5 |
70.3 |
88.3 |
0.840 |
<0.001 |
 |
|
Fig. 1 ROC curves of blood NT-proBNP,
IL-17, CRP and ESR for distinguishing Incomplete Kawasaki
disease and infectious diseases.
|
We finally combined the clinical manifestations and
laboratory results for distinguishing incomplete Kawasaki disease and
infectious diseases. When we chose the consistency with indicator 2 and
3 in Kawasaki disease diagnosis criteria, blood IL-17
≥ 11.55 pg/mL and
blood NT-proBNP ≥225.5
pg/dL as the criteria, the sensitivity and specificity for
distinguishing incomplete Kawasaki disease and infectious diseases
reached 86.5% (64/74) and 94.8% (380/401), respectively. When we chose
the consistency with indicator 1 and 2 in Kawasaki disease diagnosis
criteria, the appearance of decrustation and (or) the BCG Erythema,
blood IL-17 ≥11.55
pg/mL and blood NT-proBNP ≥225.5
pg/dL as the criteria, the sensitivity and specificity for
distinguishing incomplete Kawasaki disease and infectious diseases
reaches 43.2% (32/74) and 100% (401/401), respectively.
Discussion
In this retrospective record-review, we found that
the blood NT-proBNP levels in Kawasaki disease and incomplete Kawasaki
disease are higher than that in infectious diseases. Recent studies also
report that the level of blood NT-proBNP is of great significance in
diagnosing incomplete Kawasaki disease at an early time [5,6]. Secreted
NT-proBNP is increased in Kawasaki disease and incomplete Kawasaki
disease because of the partial inflammatory damages of cardiac muscle,
and also increased synthesis in the ventricular myocytes stimulated by
some inflammatory factors [7,8].
We found a much higher level of blood IL-17 in
Kawasaki disease and incomplete Kawasaki disease compared with
infectious disease. IL-17, as an inflammatory factor, guides neutrophil
and monocyte towards vascular wall to catalyze the reaction of
inflammations and participate in the emergence of multiple self-immune
diseases and inflammatory responsive diseases, for example systemic
lupus erythematosus [9], systemic onset juvenile idiopathic arthritis
[10] and Kawasaki disease [11], by inducing the penetration and damages
of blood vessel tissues [12-14]. It seems that the combination of blood
IL-17 and NT-proBNP further improves the specificity for the diagnosis
of incomplete Kawasaki disease.
In children with fever of more than five days without
a diagnosis, accompanied by indicator 1 and 2 of Kawasaki disease
diagnosis criteria (decrustation and/or BCG erythema), and blood IL-17
≥11.55 pg/mL
and blood NT-probing ≥225.5
pg/dL; the specificity for distinguishing incomplete Kawasaki disease
and infectious diseases reached almost 100%. Therefore, even if the
patients are at the early stage and have no coronary artery lesions,
based on decrustation and or BCG erythema, and abnormally high blood
IL-17 and NT-proBNP levels, they can be reasonably diagnosed with
incomplete Kawasaki disease.
Contributors: All authors have contributed,
designed and approved the study.
Funding: Zhejiang Medical and Hygienic Scientific
Research Fund (2008B168); Competing interests: None stated.
References
1. Sudo D, Monobe Y, Yashiro M, Mieno MN, Uehara R,
Tsuchiya K, et al. Coronary artery lesions of incomplete Kawasaki
disease: a nationwide survey in Japan. Eur J Pediatr. 2012;171:651-6.
2. Muta H, Ishii M, Yashiro M, Uehara R, Nakamura Y.
Late intravenous immunoglobulin treatment in patients with Kawasaki
disease. Pediatrics. 2012;129:e291-7.
3. Newburger JW, Takahashi M, Gerber MA, Gewitz MH,
Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term
management of Kawasaki disease: a statement for health professionals
from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki
Disease, Council on Cardiovascular Disease in the Young, American Heart
Association. Pediatrics. 2004;114:1708-33.
4. Penack O, Beinert T, Buchheidt D, Einsele H,
Hebart H, Kiehl MG, et al. Management of sepsis in neutropenia:
guidelines of the infectious diseases working party (AGIHO) of the
German Society of Hematology and Oncology (DGHO). Ann Hematol.
2006;85:424-33.
5. Cho SY, Kim Y, Cha SH, Suh JT, Han MY, Lee HJ.
Adjuvant Laboratory Marker of Kawasaki Disease; NT-pro-BNP or hs-CRP.
Ann Clin Lab Sci. 2011;41:360-3.
6. No SJ, Kim DO, Choi KM, Eun LY. Do predictors of
incomplete Kawasaki disease exist for infants? Pediatr Cardiol.
2013;34:286-90.
7. Iwashima S, Ishikawa T. B-type natriuretic peptide
and N-terminal pro-BNP in the acute phase of Kawasaki disease. World J
Pediatr. 2013;9:239-44.
8. Di Yazhen, Wu Ling, Li Yunyan, Ma Tianrui, Wang
Tianbo, Lin Yahong, et al. The clinical value of plasma
N-terminal pro-brain natriuretic peptide and serum albumin in the early
diagnosis of incomplete Kawasaki disease. Chinese J Rheumatol.
2013;9:595-600.
9. Rana A, Minz RW, Aggarwal R, Anand S, Pasricha N,
Singh S. Gene expression of cytokines (TNF-alpha, IFN-gamma), serum
profiles of IL-17 and IL-23 in paediatric systemic lupus erythematosus.
Lupus. 2012;21:1105-12.
10. Omoyinmi E, Hamaoui R, Pesenacker A, Nistala K,
Moncrieffe H, Ursu S, et al. Th1 and Th17 cell subpopulations are
enriched in the peripheral blood of patients with systemic juvenile
idiopathic arthritis. Rheumatology (Oxford). 2012;51:1881-6.
11. Jia S, Li C, Wang G, Yang J, Zu Y. The T helper
type 17/regulatory T cell imbalance in patients with acute Kawasaki
disease. Clin Exp Immunol. 2010;162:131-7.
12. Jadidi-Niaragh F, Mirshafiey A. The deviated
balance between regulatory T cell and Th17 in autoimmunity.
Immunopharmacol Immunotoxicol. 2012;34:727-39.
13. Maddur MS, Miossec P, Kaveri SV, Bayry J. Th17
cells: biology, pathogenesis of autoimmune and inflammatory diseases,
and therapeutic strategies. Am J Pathol. 2012;181:8-18.
14. Miossec P, Kolls JK. Targeting IL-17 and TH17
cells in chronic inflammation. Nat Rev Drug Discov. 2012;11:763-76.
|
|
|
 |
|

