|
|
|
Indian Pediatr 2010;47: 527-528 |
 |
Transjugular Intrahepatic Portosystemic Shunt
(TIPSS) for Budd Chiari Syndrome |
|
RP Hasija, A Nagral*, S Marar† and AR Bavdekar**
From the Departments of Pediatrics,*Gastroenterology, and
†Interventional Radiology, Jaslok Hospital and Research Center, Mumbai and
Department of Pediatrics, ** KEM Hospital, Pune, India.
Correspondence to: Dr Aabha Nagral, Consultant
Hepatologist,
7, Snehasagar, Prabhanagar, Prabhadevi, Mumbai 400 025, India.
Email: [email protected]
Received: March 2, 2009;
Initial review: April 13, 2009;
Accepted: May 8, 2009.
|
|
Abstract
We report a four year old boy who presented with
liver failure secondary to anti-thrombin III deficiency related Budd
Chiari syndrome. He was treated with TIPSS (transjugular intrahepatic
porto systemic shunt) which reversed the encephalopathy, normalised the
liver function and improved growth, pre-empting the need for a liver
transplantation. This is the first reported case of TIPSS in a child
with a fulminant presentation of Budd-Chiari Syndrome.
Key words: Budd chiari Syndrome, Hepatic
venous outflow obstruction, Transhepatic portosystemic shunt.
|
|
B
udd Chiari syndrome (BCS) or
hepatic venous outflow obstruction (HVOO) is a disease complex resulting
from obstruction to the hepatic venous outflow at the level of the hepatic
veins or the inferior vena cava. If left untreated, it results in fatal
portal hypertension, cirrhosis and liver failure. Treatment of HVOO
involves establishing the patency of the hepatic venous outflow tract.
With the introduction of newer radiological
interventions, HVOO has been safely treated with good outcome in adults.
Published literature on radiological therapeutic interventions in
pediatric BCS is scarce. We report an unusual presentation of a child with
BCS presenting with liver failure in whom a radiological intervention
reversed the liver dysfunction.
Case Report
A 4 year male child presented with progressive
abdominal distension secondary to ascites of two months duration. He was
diagnosed to have BCS on ultrasound doppler, which showed occlusion of all
three hepatic veins.
He was brought to our hospital in a comatose state,
deeply icteric, acidotic with severe abdominal distension (ascites and
hepatosplenomegaly; liver 8cm and spleen 3cm palpable). There was a
history of fever of three days, prior to hospitalization. Investigations
revealed Hb-9 g/dL WBC-17,600/mm3,
platelets - 50,800/mm3, serum creatinine – 0.4mg/dL, total bilirubin-
21mg/dL (direct bilirubin- 16 mg/dL), aPTT 70/30 seconds, INR-2.2, albumin
2 g/dL. A thrombophilia profile revealed deficient anti thrombin III (39%;
range: 80-120%). Factor V Leiden mutation, Protein C, Protein S, Anti-phospholipid
antibody and lupus anticoagulant were within normal range. JAK 2 mutation
was absent. The blood and urine cultures were negative. On testing, his
mother was also anti-thrombin III deficient (3%).
The patient was first stabilized hemodynamically and
given broad spectrum antibiotics and anti-coma measures till he regained
consciousness and became afebrile. While he improved clinically, the
bilirubin levels kept rising to a maximum of 29 mg/dL. On day 6 of
hospitalization, under the cover of fresh frozen plasma and
cryoprecipitate, IVC and hepatic venogram was performed, which revealed
ostial blocks of all three hepatic veins. The right branch portal vein was
cannulated from the IVC, portal venous pressure measured 28 mm Hg. A 10mm
× 6 cm ‘Viatorr’ stent was placed between the main portal vein and IVC
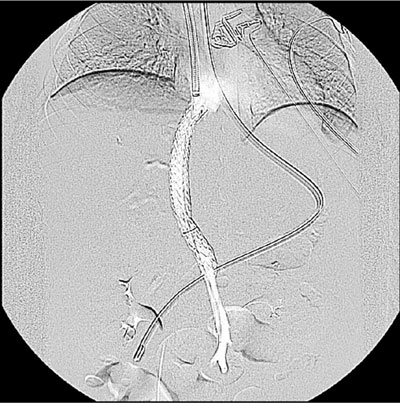
(Fig. 1). Post procedure, the venogram showed good flow from
portal vein to IVC, and the porto-systemic gradient was 4 mm Hg. The liver
size reduced rapidly (to just being palpable at time of discharge) and the
ascites, which had been therapeutically tapped dry pre-procedure, did not
recur. He was off diuretics immediate post procedure and ascites free on
day 10. There were no further episodes of hepatic encephalopathy. The INR
was 2.8 and total bilirubin was 28 mg/dL; anticoagulation was thus
deferred immediate post-procedure. Follow-up showed normalization of liver
function over the next six months. Growth monitoring showed a growth spurt
and ‘catch-up growth’ in both weight and height velocity. Follow-up
doppler at 10 days and 6 months post procedure showed normal stent flow
and no ascites.
 |
|
Fig. 1 Viatorr stent placed between the
main portal vein and the inferior vena cava. |
Discussion
Transjugular intrahepatic portosystemic shunt (TIPSS)
for hepatic venous outflow obstruction, though commonly used in
adults(1,2), is rarely used in children(3-5). There is no report of TIPSS
for a fulminant presentation of BCS in a child. TIPSS in a setting of such
high levels of bilirubin and INR is usually a contraindication, as it may
precipitate hepatic encephalopathy in the setting of cirrhosis. However,
in our patient, TIPSS was performed with the aim of reducing the portal
hypertension and improving the blood flow to the liver. Since the cause
(compromised venous outflow) in this child was treated with TIPSS, he
actually improved in terms of hepatomegaly, liver function and
encephalopathy. TIPSS also averted the need for a liver transplantation.
This is unlike performing a TIPSS in a decompensated cirrhotic patient,
where encephalo-pathy is likely to worsen. However, these inter-ventions
have to be used selectively. Our recently published data of this
intervention in children with BCS shows it to be safe and successful(6).
Contributors: Treatment conceived by AN, SM
and AB. Manuscript prepared by RH and supervised by AN.
Funding: None.
Competing interests: None stated.
References
1. Griffith JF, Mahmoud AE, Cooper S, Elias E, West RJ,
Olliff SP. Radiological intervention in Budd Chiari syndrome: techniques
and outcome in 18 patients. Clin Radiol 1996; 51: 775-784.
2. Eapen CE, Velissaris D, Hevdtmann M, Gunson B,
Olliff S, Elias E. Favourable medium term outcome following hepatic vein
recanalisation and/or transjugular intrahepatic portosystemic shunt for
Budd Chiari syndrome. Gut 2006; 55: 761-763.
3. Huppert PE, Astfalk W, Brambs HJ, Schweizer P,
Schott U, Pereira P, et al. Transjugular intrahepatic portosystemic
shunt in children. Initial clinical experiences and literature review.
Rofo 1998; 168: 595-603.
4. Cauchi J , Oliff S, Baumann U, Mirza D, Kelly D,
Hewitson J, et al. The Budd-Chiari syndrome in children: the
spectrum of management. J Pediatr Surg 2006; 41: 1919 - 1923.
5. Bogdan H, Franchi-Abella S, Aurelie P, Dalila H,
Alexis M, Sibert A, et al. Budd-Chiari syndrome and essential
thrombocythemia in a child: favorable outcome after transjugular
intrahepatic portosystemic shunt. J Pediatr Gastroenterol Nutr 2008; 46:
334-337.
6. Nagral A, Hasija RP, Marar S, Nabi F. Budd Chiari
syndrome in children: experience with therapeutic radiological
intervention. J Pediatr Gastroenterol Nutr 2010; 50: 74-78.
|
|
|
 |
|

