|
T
he diagnosis of focal segmental
glomerculosclerosis (FSGS) is based on findings on light microscopy
examination, including sclerosis of glomeruli and involvement of only a
portion of the capillary tuft. On immunofluorescence examination, the
segmental lesions may show strong staining for IgM and C3(1, 2).
Occasional cases of familial FSGS have been reported(3). Patients with
steroid resistant nephrotic syndrome (SRNS) are at risk for developing end
stage renal disease(2). We conducted this study to determine the
prognostic value of clinical, laboratory, histopathologic and therapeutic
factors in children with FSGS.
Methods
Of 99 patients with idiopathic FSGS seen at this center
during 1986 to 2002, 62 were included. All patients had features of
nephrotic syndrome, only patients with a minimum follow up of 5 yr or
estimated glomercular filtration rate (GRF)
³75
mL/min/1.73 m2 were included(4). Thirty seven patients who did not return
for follow up visits were excluded. Secondary FSGS was excluded based on
history, clinical, serologic and immunofluorescence examination findings
and imaging studies. Hematuria was defined by presence of
³5
red cells/HPF and hypertension as systolic or diastolic blood pressure
more than 95th percentile for age and gender(5).
Steroid responder was defined as: (i) patients
in remission following treatment with prednisone or prednisolone at a dose
of 2 mg/kg daily for 4 weeks, (ii) remission following therapy with
cyclophosphamide (2 mg/kg for 12 weeks or 3 mg/kg for 8 weeks); or (iii)
remission after therapy with cyclosporine (5 mg/kg daily for 12 months).
Remission was defined as no proteinuria for 3 consecutive days or 24-hour
urine protein excretion <4 mg/m 2/h.
Chronic kidney disease was defined as an abnormality of kidney function
which has been present for 3 or more months(6). Comparison between
patients who were non-responder and responder was done using chi-square
test, Fisher’s exact or Mann-Whitney tests; P<0.05 was considered
significant.
All patients received prednisolone or prednisone at a
dose of 2 mg/kg daily for 4 weeks, then 2 mg/kg every other day 4 weeks
which was tapered slowly in 3-6 months. Twelve patients underwent kidney
biopsy before starting treatment due to gross hematuria, sustained
hypertension, evidence of azotemia or age
£1
yr and others after treatment with steroid due to steroid unresponsiveness
or if they were considered for treatment with cyclophos-phamide or
cyclosporine. In patients with steroids resistance, cyclophosphamide was
used. Patients whose parents did not consent for treatment with
cyclophosphamide received cyclosporine with prednisolone (0.1-0.5 mg/kg on
alternate days). We used cyclosporine in patients with cyclophospha-mide
resistance or relapse of disease after cyclo-phosphamide withdrawal.
Results
Thirty six patients (58%) were
£6
year old and 24 (38.7%) were >6 year; 41 (66.1%) were boys. The mean
(range) of follow-up was 7.2 (0.25-16.3) year. Twenty five patients
(40.3%) were steroid sensitive and rest were steroid resistant.
Table I shows variables in steroid resistant and steroid sensitive
patients. Twelve of 35 patients (34.3%) responded to cyclophosphamide and
2 of 16 (12.5%) responded to cyclosporine. There was no correlation
between age at onset, gender, presence of hematuria or hypertension at
presentation and histopathologic findings with outcome.
TABLE I
Correlation between Clinical Features and Outcome in Idiopathic FSGS
|
Variable |
Steroid
Sensitive |
Steroid
Resistant |
Renal function on
last follow-up
|
| |
Group 1
(n=25) |
Group 2
(n=37) |
Normal renal function |
Chronic kidney
disease |
Group 1
(n=22) |
Group 2
(n=15) |
Group1
(n=3) |
Group 2
(n=22) |
| Age ≤ 6
yr |
20 |
17 |
17 |
6 |
3 |
11 |
| Age > 6
yr |
5 |
18 |
5 |
9 |
0 |
9 |
| Males |
18 |
23 |
15 |
11 |
3 |
12 |
|
Hypertensive |
4 |
8 |
3 |
2 |
1 |
6 |
| Hematuria
|
7 |
20 |
7 |
6 |
0 |
14 |
|
Renal histology† |
|
Hilar FSGS |
9 |
6 |
8 |
3 |
1 |
3 |
|
Tip FSGS |
5 |
12 |
4 |
5 |
1 |
7 |
|
Non-specified FSGS |
4 |
7 |
4 |
3 |
0 |
4 |
|
Collapsing FSGS |
2 |
10 |
1 |
3 |
1 |
7 |
|
Mild to moderate glomerulosclerosis |
19 |
29 |
16 |
13 |
3 |
16 |
|
Severe glomerulosclerosis |
1 |
6 |
1 |
1 |
0 |
5 |
| No
tubular atrophy |
2 |
4 |
2 |
2 |
0 |
2 |
|
Mild to moderate tubular atrophy |
16 |
24 |
13 |
10 |
3 |
14 |
|
Severe tubular atrophy |
2 |
7 |
2 |
2 |
0 |
5 |
| No
interstitial fibrosis |
1 |
4 |
1 |
2 |
0 |
2 |
|
Mid to moderate interstitial fibrosis |
17 |
21 |
14 |
10 |
3 |
11 |
|
Severe interstitial fibrosis |
2 |
10 |
2 |
2 |
0 |
8 |
* The age at onset
of two patients was unknown.
† Immunofluorescence microscopy examination was done in 34 patients
and detailed review of renal histopathology in 55. |
Histologic specimens were reviewed for proportion of
glomeruli showing segmental glomerulosclerosis, interstitial fibrosis,
tubular atrophy and types of FSGS (tip, hilar, collapsing and
non-specified types). Severe interstitial fibrosis was found (P=0.03)
in patients whose diseases progressed to chronic kidney disease. Patients
showing steroid resistance or non-response to cyclophosphamide were
significantly more likely to show deranged renal functions (P=0.0002
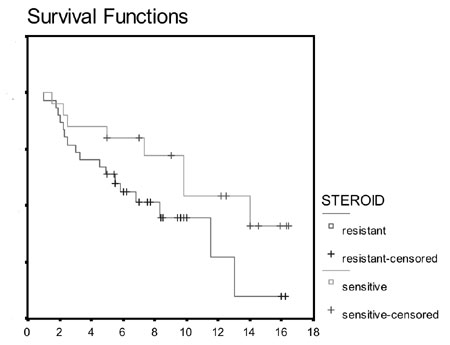
and P=0.003, respectively). Fig. 1 shows renal
survival in steroid sensitive versus steroid resistant FSGS.
Relative risks for renal dysfunction in steroid, cyclophosphamide and
cyclosporine non-responders were 2.17 (95% confidence interval (CI)
1.43-3.29), 3.13 (95% CI 1.49-6.59) and 2.33 (95% CI 1.27-4.27),
respectively.
 |
Follow up (months) |
| |
|
|
Total |
number |
number |
percent |
| |
|
events |
censored |
censored |
|
Steroid sensitive |
25 |
8 |
17 |
68 |
|
Steroid sensitive |
37 |
17 |
20 |
54 |
|
| |
Fig. 1 Kaplan Meir graph showing renal survival outcome in
steroid sensitive versus steroid resistant FSGS.
|
Discussion
Ostalska, et al.(7) reported a less favorable
clinical course in children <1 year of age. The clinical course has been
suggested to be satisfactory if sclerotic lesions are peripheral, although
these findings have not been confirmed by others(8). Renal survival has
been directly associated with degree of proteinuria(9). Cyclophosphamide
may have some survival benefits in those with at least a partial response
measured by impact on proteinuria and progression to ESRD(10), but a
randomized trial showed that there was no difference in renal survival
after cyclophosphamide treatment(11).
It is suggested that therapy with alkylating agents
might not be useful for treatment of primary FSGS. Patients in this study
showed a relatively better response to cyclophosphamide and 34.3% reached
complete remission. Two out of 12 (16.2%) patients who were
cyclophosphamide responsive and 17 out of 23 (73.9%) non responders showed
progression of renal dysfunction.
Paik, et al.(12) showed that asymptomatic
proteinuria at presentation, initial renal insufficiency; higher segmental
sclerosis, severe tubulointerstitial changes, initial non-responder and
absence of remission are poor prognostic factors. Another study reported a
renal survival rate of 90% in responders while in non-responders it was
48%(13). In our study, renal survival rates for steroid, cyclophosphamide
and cyclosporine responders were 88%, 83.8% and 100%, respectively.
Findings from this study suggest that satisfactory responses to therapy
with steroids and cyclophosphamide results in improved long term outcome.
Acknowledgment
The authors would like to thank Drs Bodaghi, Esfehani,
Mohseni, Ahmadi, Mahjob and Sadeghi and Ms Haddady for their help in this
work and in the preparation of the manuscript.
Contributors: MN, AM and NM were involved in
designing the study; MN and HN were involved in data collection. The final
manuscript was approved by all authors.
Funding: None.
Competing interests: None stated.
|
What This Study Adds?
• Therapy with cyclophosphamide is promising in
patients with steroid resistant focal segmental glomerulosclosis.
|
References
1. Alpers CE. The kidney. In: Kumar V, Abbas AK,
Fausto N, eds. Robbins and Cortan pathologic basis of disease, 7 th
edn. Philadelphia: Elsevier Saunders; 2005. p. 955-1021.
2. Niaudet P. Steroid-resistant idiopathic nephrotic
syndrome in children. In: Avner ED, Harmon W, Niaudet P, eds. Pediatric
Nephrology Textbook, 5th edn. Philadelphia:
Williams and Wilkins; 2004. p. 557-573.
3. Frishberg Y, Rinat C, Megged O, Shapira E, Feinstein
S, Raas-Rothschild A. Mutations in NPHS2 encoding podocin is a prevalent
cause of steroid-resistant nephrotic syndrome among Israeli-Arab children.
J Am Soc Nephrol 2002; 13: 400-405.
4. Guignard JP, Santos F. Laboratory investigations.
In: Avner ED, Harmon W, Niaudet P, eds. Pediatric Nephrology Textbook,
5th edn. Philadelphia: Williams and
Wilkins; 2004. p. 399-424
5. Bender JU, Bonilla-Felix MA, Portman RJ.
Epidemiology of hypertension. In: Avner ED, Harmon W, Niaudet P,
ed. Pediatric Nephrology Textbook, 5th edn.
Philadelphia: Williams and Wilkins; 2004. p.1125-1151.
6. Levin A. The advantages of a uniform terminology and
staging system for chronic kidney disease (CKD). Nephrol Dial Transplant
2003; 18: 1446-1451.
7. Ostalska-Nowicka D, Zachwieja J, Maciejewski J,
WoŸniak A, Salwa-Urawska W. The prognostic value of glomerular immaturity
in the nephrotic syndrome in children. Pediatr Nephrol 2004; 19: 633-637.
8. Morita M, White RH, Coad NA, Raafat F. The clinical
significance of the glomerular location of segmental lesions in focal
segmental glomerulosclerosis. Clin Nephrol 1990; 33: 211-219.
9. Gipson DS, Chin H, Presler TP, Jennette C, Ferris
ME, Massengill S, et al. Differential risk of remission and ESRD in
childhood FSGS. Pediatr Nephrol 2006; 21: 344-349.
10. Geary DF, Farine M, Thorner P, Baumal R. Response
to cyclophosphamide in steroid-resistant focal segmental
glomerulosclerosis: a reappraisal. Clin Nephrol 1984; 22: 109-113.
11. Abeyagunawardena AS, Sebire NJ, Risdon RA, Dillon
MJ, Rees L, Van’t Hoff W, et al. Predictors of long-term outcome of
children with idiopathic focal segmental glomerulosclerosis. Pediatr
Nephrol 2007; 22: 215-221.
12. Paik KH, Lee BH, Cho HY, Kang HG, Ha IS, Cheong HI,
et al. Primary focal segmental glomerular sclerosis in children:
clinical course and prognosis. Pediatr Nephrol 2007; 22: 389-395.
13. Tarshish P, Tobin JN, Bernstein J, Edelmann CM Jr.
Cyclophosphamide does not benefit patients with focal segmental
glomerulosclerosis. A report of the International Study of Kidney Disease
in Children. Pediatr Nephrol 1996; 10: 590-593.
|

