Coronavirus disease (COVID-19) in children
appears to be largely a benign condition. However, there are
reports of children presenting significantly unwell across
Europe and USA in the last couple of weeks with a new
multisystem inflammatory syndrome [1]. We report a child with
COVID-19 who had overlapping features of Toxic Shock Syndrome
(TSS) and Kawasaki disease (KD).
A previously well, eight-year-old boy presented
with fever, cough and throat pain. He was admitted to a local
hospital on day 4 of illness in view of high-grade fever spikes.
Investigations showed neutrophilic leukocytosis (total white
blood cell count 23,000/µL, Neutrophils 89%) with raised acute
phase reactants (C-reactive protein, CRP 120 mg/L). Chest X-ray
showed right upper and middle lobe infiltrates. Reverse
transcriptase polymerase chain reaction (RT-PCR) for severe
acute respiratory illness novel coronavirus 2 (SARS-CoV-2) was
negative. Treatment was empirically started with ceftriaxone and
azithromycin. Despite treatment for three days, he continued to
have high fever, worsening respiratory symptoms and was referred
to our hospital.
On arrival, he was alert, had
respiratory rate of 50/min, intercostal retractions and was
maintaining SpO2 in
room air. He was febrile with tachycardia (HR 160/min),
hypotension (80/31 mm Hg), warm extremities and a capillary
refill time of 3 seconds. He was also noted to have a
generalized non-pruritic erythematous skin rash, non-purulent
bulbar conjunctivitis, cracked lips, strawberry tongue, edema of
limbs, tender hepatomegaly and abdominal distention.
Investigations in our hospital showed haemoglobin of 8.9 g/dL,
neutrophil predominant leukocytosis (total count 17,600/µL, 86%
neutrophils), platelet count 3,95,000/µL, markedly raised
CRP (317 mg/L), raised erytherocyte sedimentation rates
(115 mm/h), hyper-ferritinemia (Ferritin 1,496 ng/mL),
hypoalbuminemia (2.6 g/dL), hyponatremia (133 mEq/L), normal
kidney and liver function, and 2+ proteinuria. He was given a
fluid bolus and treatment empirically started with
piperacillin-tazobactam and doxycycline. When reassessed after
30 minutes, he was febrile, hypotensive and had increased work
of breathing. He was shifted to the pediatric intensive care
unit. The initial differential diagnoses were pneumonia with
septic shock, COVID-19 penumonitis, KD and TSS.
High-flow nasal cannula (HFNC) support was started and
antibiotics were modified to meropenem, vancomycin and
clindamycin. The blood pressure was stable and urine output was
normal. Intravenous Immunoglobulin (IVIG) was given (2 g/kg)
with aspirin (75 mg once-a-day). Echocardio-gram did not show
any abnormalities and repeat chest X-ray showed increased
right-sided infiltrates. Repeat nasopharyngeal COVID-19 RT-PCR
was positive. Multiplex PCR of nasopharyngeal aspirate (BioFire
FilmArray) detected Coronavirus OC43 and Human
Rhino/Enterovirus. As he improved, he was gradually weaned off
HFNC. Blood cultures showed no growth and antibiotics were
changed to ceftriaxone. In light of the persistent high-grade
fever and elevated CRP (121 mg/L), 72 hours after IVIG infusion,
he was given tocilizumab (8 mg/kg IV over 2 hours). Twelve hours
later, his fever spikes settled, and inflammatory parameters
rapidly decreased to baseline (Fig. 1). He was
noted to have periungual peeling of skin and recovered
completely after two weeks of illness.
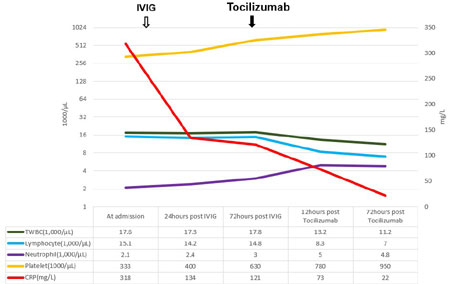 |
| Fig. 1 Trend of
inflammatory markers in a child with hyper-inflammatory
syndrome and COVID-19. |
The clinical characteristics of COVID-19 disease
progression and outcome in children and young adults appear
significantly milder compared to older individuals [2]. However,
there is now a growing recognition of a small number of children
presenting with a multisystem inflammatory syndrome. This rare
syndrome shares common features with other pediatric
inflammatory conditions, including KD,
Staphylococcal/streptococcal toxic shock, bacterial sepsis and
macrophage activation syndrome. It can also present with unusual
abdominal symptoms with elevated inflammatory markers. Recently
8 children have been reported to present with hyper-inflammatory
shock [3]. This has been labelled as Pediatric multisystem
inflammatory syndrome temp-orally associated with COVID-19 and a
case definition has been suggested [1]: a child presenting with
persistent fever, inflammation (neutrophilia, elevated CRP and
lymphopenia) and evidence of single or multi-organ dysfunction
(shock, cardiac, respiratory, renal, gastrointestinal or
neurological disorder) with additional features, which may
include fulfilling full or partial criteria for KD; exclusion of
any other microbial cause, including bacterial sepsis,
staphylococcal or streptococcal shock syndromes; and SARS-CoV-2
PCR testing may be positive or negative
Our case fulfils these criteria. It is likely that
cytokine storm (CS) is one of the major causes of acute
respiratory distress syndrome (ARDS), multi-organ dysfunction
and possibly pediatric multisystem inflammatory syndrome [4].
IL-6 is a key cytokine in this process and few studies suggest
that CS is positively correlated with disease severity [5].
Various immunomodulators have been discussed and tried for
controlling the inflammatory response [6]. Tocilizumab, an IL-6
receptor antagonist approved by the US FDA for treating of
Cytokine release syndrome (CRS), is now in clinical trials for
treating severe COVID-19 pneumonia [7]. Tocilizumab blocks
downstream signal transduction by binding membrane IL-6 receptor
and soluble IL-6 receptor and plays a role in the treatment of
CS in COVID-19 [8]. High CRP levels seen in our case shows that
this inflammatory syndrome is likely mediated by IL-6. Our case
suggests that immunomodulation with IVIG and IL-6 blockade can
be an effective therapeutic strategy, which has a scientific
rationale. It is clear from Europe and the USA that appearance
of this syndrome in children follows the peak of infections in
affected areas. The immunopathology behind this phenomenon is
yet to ascertained. We believe that children across India may
present with this inflammatory syndrome related to COVID-19 in
the weeks ahead and would like to highlight this to
pediatricians across India. Tocilizumab may prove to be an
effective second line agent in IVIG refractory children with
COVID-19 hyper-inflammatory syndrome
Though most SARS-CoV-2 infections in children are
likely to present with mild features, some may develop a
hyper-inflammatory syndrome, which may require treatment with
IVIG and Tocilizumab. Pediatricians should be aware of such
presentation and immuno-modulatory treatment modalities.
Contributors:
SB,TMN,BR: took part in treating the patient and preparing the
manuscript; AVR: patient management and preparing the
manuscript.
Funding:
None; Competing interest: None stated.
REFERENCES
1. RCPCH.
Guidance - Paediatric multisystem inflammatory syndrome
temporally associated with COVID-19.Available from:
https://www.rcpch.ac.uk/resources/guidance-paediatric-multisystem-inflammatory-syndrome-temporally-associated-covid-19.
Accessed May 02, 2020.
2.
Balasubramanian S, Rao NM, Goenka A, Roderick M, Ramanan AV.
Coronavirus Disease (COVID-19) in Children - What We Know So Far
and What We Do Not?. Indian Pediatr.2020 Apr 9 [Epub ahead of
print]. Available from:https://www.indianpediatrics.net/COVID29.03.2020/SA-00159.pdf.
Accessed May 09, 2020.
3. Riphagen S,
Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P.
Hyperinflammatory shock in children during COVID-19 pandemic.
Lancet. 2020 May 07. [Epub ahead of print]. Available from:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31094-1/fulltext.
Accessed on May 09, 2020.
4. Ye Q, Wang
B, Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’
in COVID-19. J Infect. 2020 Apr 10. [Epub ahead of print].
Available from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7194613/pdf/main.pdf.
Accessed May 09, 2020.
5. Huang C,
Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical
features of patients infected with 2019 novel coronavirus in
Wuhan, China. Lancet 2020;395:
497-506.
6. Zhang W,
Zhao Y, Zhang F, Wang Q, Li T, Liu Z, et al. The use of
anti-inflammatory drugs in the treatment of people with severe
coronavirus disease 2019 (COVID-19): The perspectives of
clinical immunologists from China. Clin Immunol.
2020;214:108393.
7.
ClinicalTrials.gov: A Study to Evaluate the Safety and Efficacy
of Tocilizumab in Patients with Severe COVID-19 Pneumonia.
Available from:
https://clinicaltrials.gov/ct2/show/NCT04320615. Accessed
May 03, 2020.
8.
Luo P, Liu Y, Qiu
L, Liu X, Liu D, Li J. Tocilizumab treatment in COVID 19: A
single center experience. J Med Virol. 2020 Apr 06 [Epub ahead
of print]. Available from:
https://onlinelibrary.wiley.com/doi/epdf/10.1002/jmv. 25801.
Accessed May 9, 2020.

