|
We report a case of incomplete Kawasaki disease
in a child who also tested positive for COVID-19. This case
brings attention to the diverse presentation of coronavirus
disease (COVID-19) disease in children.
A 5-year-old previously healthy African American
male was admitted to the Pediatric inpatient floor with daily
fever up to 39.4°C for 8 days. He had a history of rash,
swelling (palms and soles), conjunctivitis, decreased appetite,
diarrhea, dysuria, and abdominal pain. He had been treated with
cefdinir for positive rapid streptococcal antigen test four days
before, without clinical improvement. Physical examination
showed dry, cracked, erythematous lips, non-exudative
conjunctivitis, and bilateral shotty cervical lymphadenopathy
but no rash. He had right scrotal edema and hydrocele suggestive
of epididymo-orchitis on ultrasound. Clinically, he met the
criteria for incomplete Kawasaki disease
(KD).
Initial laboratory workup was significant for
leukocytosis (white blood cells 40,000/cumm), anemia (hemoglobin
8 g/dL), thrombocytopenia (platelet count 104,000/cumm),
elevated inflammatory markers (ESR 72 mm, CRP 25.6 mg/dL,
procalcitonin 27 ng/mL, ferritin 1030 ng/mL), hyponatremia
(serum sodium 121 meq/L), pyuria, hypoalbuminemia (2 g/dL),
elevated liver enzymes (ALT 55 U/L), elevated troponins (0.06
ng/mL) and negative
rapid influenza A/B antigens. Chest X-ray showed an
enlarged cardiac silhouette (Fig. 1). Severe acute
respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA was detected
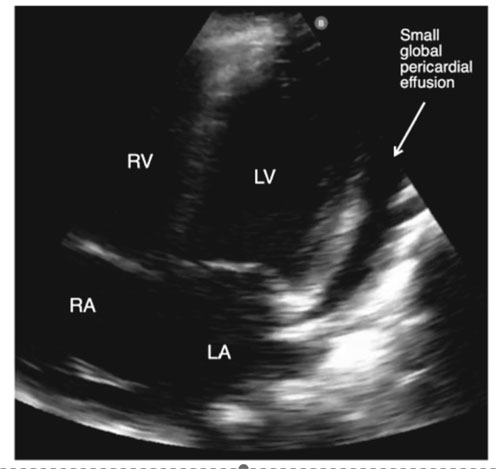
on RT-PCR from his nasopharyngeal swab. Echocardiogram showed a
small global pericardial effusion but no ectasia, dilation, or
aneurysm formation of coronary arteries (Fig. 2).
 |
|
Fig.1 Chest
radiograph showing enlarged cardiac silhouette. |
| |
| |
 |
|
Fig. 2 Apical
four chamber view of a two dimensional echocardiogram of
the patient showing a small global pericardial effusion.
LA-Left Atrium; LV-Left ventricle; RA-Right atrium;
RV-Right ventricle. |
He was transferred to the pediatric intensive care
unit because of hypotension. He received fluid boluses and
intravenous immunoglobulin (IVIG) therapy was begun, which had
to be discontinued because of recurring hypotension. He was
briefly supported with high flow nasal cannula up to 10 liter
for tachypnea and increased work of breathing, which was
weaned-off. Once he was hemodynamically stable, IVIG infusion
was resumed slowly at 5 grams over 10 hours (2-5 mL/minute) for
6 doses for a total dose of 30 grams (1.8 g/kg) [1]
with a different formulation,
after
pre-medicating with diphenhydramine and methylprednisolone (only
for the first dose) and started on medium-dose aspirin (~39
g/kg/day).
The patient recovered on the pediatric floor with
supportive therapy for COVID-19 [3] and was discharged after 6
days in the hospital. Hypotension with elevated inflammatory
markers in patients with KD are the manifestations of KD shock
syndrome (KDSS) [4]. Association between COVID-19 and KDSS [5]
has been speculated, but warrants further investigation.
Adverse effects to IVIG infusion commonly include
hypotension and anaphylactic reactions. This can be treated with
steroids and antihistamines as pre-medication. However, there is
a weak recommendation regarding avoidance of steroids in
patients with COVID-19, with some indirect evidence of disease
worsening [2]. Readers need to be aware of co-occurrence of
Kawasaki disease with COVID-19, and the associated management
issues.
Contributors-
ER-drafted the manuscript; RS-supervised ER and edited the
manuscript; SS-helped with the echocardiographic images and
their labeling; PG-conceived the idea of case report,
supervised, edited and finalized the manuscript.
Funding:
none; Competing interests: None stated.
REFERENCES
1. Son MBF,
Newburger JW. Kawasaki disease. Pediatr Rev. 2018;39:78-90.
2. COVID-19
Treatment Guidelines Panel. Coronavirus Diseases 2019 (COVID-19)
Treatment Guidelines. National Institutes of Health. Available
from: https://www. covid19treatmentguidelines.nih.gov/.
Accessed May 8, 2020.
3. Chiotos K,
Hayes M, Kimberlin DW, Jones SB, James SH, Pinninti SG, et
al. Multicenter Initial Guidance on Use of Antivirals for
Children With COVID-19/SARS-CoV-2. J Pediatric Infect Dis Soc.
2020. Apr 22 [published online ahead of print]. Available from:
https://academic-oup.com/jpids/advance-article/doi/10.1093/jpids/piaa045.
Accessed May 8, 2020.
4. Kanegaye
JT, Wilder MS, Molkara D, Frazer JR, Pancheri J, Tremoulet AH,
et al. Recognition of a Kawasaki disease shock syndrome.
Pediatrics. 2009;123: e783-9.
5. Jones VG, Mills M, Suarez D, Hogan CA, Yeh
D, Bradley Segal J, et al. COVID-19 and Kawasaki disease:
Novel virus and novel case. Hosp Pediatr. 2020 Apr 7.
https://
hosppeds.aappublications.org/content/early/2020/04/06/hpeds.2020-0123.long.
Accessed May 8, 2020.
|

