In the face of the severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2) pandemic, the Indian
government has proactively taken multiple measures to slow
down disease progression. This includes converting some
hospitals to dedicated COVID-19 hospitals, and shutting down
many routine hospital services including outpatient
departments and elective operation theatres, while emergency
services have continued. However, the patients face a tough
dilemma of risk of infection during hospital visits
vis-a-vis denial of adequate care because of these
measures [1].
To ensure continued health services, the government
has given guidelines for practicing telemedicine to aid
continuous delivery of healthcare services to the public.
Telemedicine is defined as the delivery of health care
services, where distance is a critical factor, by all
healthcare professionals using information or communication
technology. It serves the purpose of exchange of valid
information for diagnosis, treatment and prevention of disease
and injury, research and evaluation, and lessens overcrowding
in hospitals, especially in the time of a pandemic [2,3].
Telemedicine aims to ensure equitable services to everyone, is
cost-effective, provides safety to both patient and doctors
during pandemics, and offers timely and faster care. Since
children represent a vulnerable population, detailed guidance
on the delivery of primary and emergent care via
telemedicine services is the need of the hour.
Telemedicine can be classified on the basis of mode
of communication as (i) audio, video or
text-based (video mode is preferred as it allows limited
examination as well); (ii) timing of information
transmitted as real time or asynchronous exchange;
(iii) purpose of consult as first
time or follow up (in non-emergent cases or emergency
consultation); and (iv) according to individuals
involved as patient to medical practitioner, caregiver
to medical practitioner, medical practitioner to medical
practitioner or health worker to medical practitioner [2]. The
use of telemedicine ranges from educational purposes such as
teleconferencing and tele-proctoring, health care delivery,
screening of diseases, and disaster management [3].
Telemedicine is widely used in areas of radiology, dermatology
and pathology; but has had a limited role in other branches in
the past. In 2018, the Bombay High Court had convicted a
doctor couple who were guilty of criminal negligence and death
of a lady after delivery because the doctor had not come and
physically examined the patient. The attending doctor directed
her staff telephonically for patient management. The Supreme
Court at that time had advised doctors to limit the use of
telemedicine and to use it only in emergencies [4]. This will
now change with the latest guidelines [2]. Despite all its
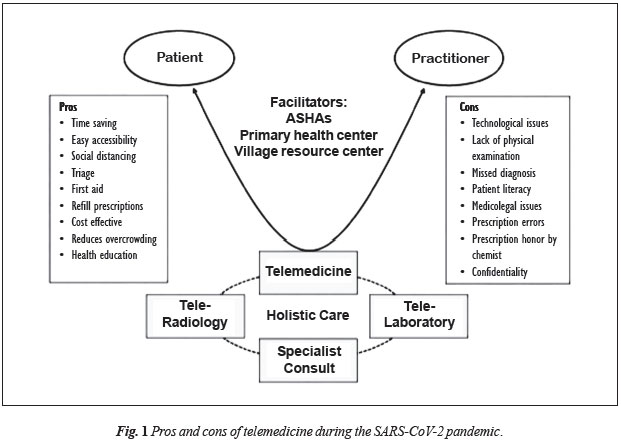
advantages, practicing telemedicine poses several challenges
to clinicians as it is an evolving tool (Fig. I).
 |
Following are some of the issues that need to be
addressed by pediatricians in the current setting of the
COVID-19 pandemic in an Indian scenario and their possible
solutions.
Lack of Physical Examination
Telemedicine has an inherent drawback since the patient is not
actually present and a thorough physical examination is not
possible. The limited examination, which is possible only
through inspection, might be hampered by low video quality or
lack of video facilities altogether. The younger the child
(especially below 2 years), the more difficult it is to make a
diagnosis based on history alone because of overlapping and
nonspecific symptoms in children. This can often lead to
underestimation or misinterpretation of the disease. To
overcome this we can ask the patients to give a detailed
description about their complaints and not merely state the
issues. We can employ the use of peripheral examination
devices like electronic stethoscope, electronic blood pressure
apparatus, pulse oximeter and ultrasonography. However,
accuracy and effectiveness of these devices needs to be
ascertained before recommendations can be made. One way to
partially overcome this challenge is to encourage telemedicine
between a health worker and pediatrician to facilitate a
rudimentary examination [5]. The pediatrician may need to have
a low threshold for ordering basic investigations because of
the limited examination possible. The health care worker can
certainly assist in triaging patients and identifying sick
children requiring an urgent inpatient visit. If no hospital
is available nearby, telemedicine might be the only option
available e.g. in a case with trauma, pediatrician can
advise appropriate first aid which may be lifesaving after
which the patient can visit the nearest hospital for
assessment of the extent of trauma and stabilization.
Medico-legal Considerations
With the issue of telemedicine practice guidelines under the
Indian Medical Council Act, 1956, medical practitioners are
now empowered and legally protected to provide telemedicine
services according to guidelines stated [2]. Clinicians may
face difficulties in providing telemedicine services in
medicolegal cases as detailed documentation is required.
Doctors should avoid giving advice in such cases and the
patient must be referred for an urgent in-person visit to the
nearest hospital.
Informed Consent
In cases where patient initiates the conversation, the consent
is implied, but if a doctor initiates the conversation an
informed consent should be taken and documented. For a minor
seeking health care, child assent is also required. The
patient and the parent can send an email, text or an
audio/video message. Wherever in doubt, consent must be
documented/ recorded.
Prescription and Liability
The doctor is liable for any advice he gives. In case the
physician takes advice from another doctor, the liability lies
on the primary physician and it is his discretion whether or
not to follow the other doctors’ advice. He can give a list of
probable or differential diagnosis and can advise the patient
to visit the nearest hospital. Unless the physician is sure of
the diagnosis, no prescription should be given – rather,
patient should be advised to visit the nearest health
facility. Age and weight are important parameters in children
for dosage calculation. Hence we must avoid giving
prescriptions if these parameters are not known. For patients
with chronic diseases, assessment of disease activity becomes
difficult and certain medications e.g. narcotics,
psychotropic drugs etc. are prohibited
for telemedicine use by the authorities. The
prescriptions when given should be in the specified format [2]
and can be counter checked at any point.
Proper record-keeping is essential for first time
and refill prescriptions (allowed for a maximum 6-month period
without onsite visit). A screenshot record of whatsapp chats,
emails texts and video recording can be kept. The pediatrician
can also ask the caregiver to call back when he feels the
symptoms are in evolving phase. Documenting the call-back
instructions given to parents is often as important as
documenting the reported symptoms to cover liability risks.
Prescriptions for common symptoms can be easily copied by
quacks in large numbers leading to irrational drug use and
quackery. For this we should have stringent laws and any
defaulter should face vigorous punishment.
Confidentiality
The practitioner can choose his telemedicine consultation
timings as per convenience. It is his choice to accept or
decline a consultation at any time. It is duty of the doctor
to maintain patient confidentiality and not to share patient
details without consent. Patient images should be sent via
secure, encrypted means of communication [6]. However, in case
either party records conversation there can be a breakdown of
the doctor-patient relationship. This relationship has
multiple cultural influences. The patient’s trust in his/her
doctor is not acquired in a moment, but in long coexistence,
especially in situations of risk [9]. The government
guidelines are not very explicit on how to address any
barriers or chinks in doctor-patient relationship. However,
the practitioner is not liable if the patient information gets
shared due to technological issues [2].
Fee
A similar fee structure as applied for inpatient visits is
applicable here as well. Telemedicine is much more economical
both for the patient and physician as it reduces cost of
travel and stay (during out-station consultations). The Indian
Academy of Pediatrics has recently introduced an app for its
members, which can be used for telemedicine consultation and
payment services.
Holistic Care
Using telemedicine, it is possible to provide a more holistic
care faster e.g., we can take advice from the expert in
a shorter duration without referring the patient for expert
opinion. Services such as tele-radiology, tele-pathology will
also aid us in faster diagnosis. Common procedures (such as
use of metered dose inhalers, technique of giving insulin
injections) can be shared with the patient/caregiver via
YouTube links, pre-prepared videos or live demonstrations.
Needless to say, this would be possible on a case-case basis
depending on the literacy and understanding of the
patient/caretaker. We can also screen patients through
telecommunication. In case we find a disease suspect we can
refer the patient for urgent testing, isolation and
management. However, certain issues like child abuse and/or
sexual abuse remain outside the purview of telemedicine in
India currently and a hospital visit would be required.
Technological Issues
Lack of widespread access to telecommunication facilities to
the wider public leads to inequitable access to health
services via telemedicine. For example, if there is a
transient error in voice transmission the patient might
receive incomplete information which can be hazardous and may
have medico-legal implications. Any breakdown in technology
should preferably be documented by the provider.
Communication
The primary person of contact in the pediatric age group is
usually not the patients themselves, but the parents or the
caregivers. The already difficult doctor-patient communication
is further compounded with telecom-munication. Moreover,
patient literacy and socio-economic factors might pose
challenges in communi-cation during telephone or video
calling. Prescriptions via this mode can also be
incorrectly interpreted, either by the patients themselves or
the chemists, which can lead to disastrous results. The
solution is to have good quality internet connections,
uninterrupted power supply, workshops on telecommunication,
and designated centers such as post offices, dispensaries and
primary health care centers where good internet services and
trained facilitators like Accredited Social Health Activists
(ASHAs) are available (Fig. I). The staff should
be trained in performing video calls and explaining
prescription to the patients. We should avoid providing
telemedicine by telephonic conversations and should encourage
video calls and provide prescriptions in the fixed format
via email. We should have a better liaison between
tertiary care hospitals and primary heath care centers, as has
been done with the Village resource centers developed by
Indian Space Research Organisation in October, 2018 [8]. If
the practitioner still faces communication glitches, he can
record the issue and terminate the conversation [2].
We as physicians have become comfortable with the
traditional method of providing treatment but in the current
scenario of the COVID-19 pandemic, a temporary change is
required [9]. With more and more healthcare professionals
getting affected, the doctor-patient ratio will further
deteriorate. Telemedicine might be the only promising solution
available. However as the usage of telemedicine will increase
in India, more issues regarding medicolegal aspects might
emerge, which should be deliberated among the medical
fraternity a priori. Although caution is necessary on
the part of a pediatrician, given the benefits of telemedicine
we must welcome it. We may find it as an important adjunct to
the traditional way of practicing medicine.
Contributors:
VM: conceived the idea, is providing telemedicine services,
wrote the 1st draft, and approved the final manuscript; TS:
literature search, assisted in writing the first draft and
approved the final manuscript; CA: edited the manuscript, and
approved the final manuscript.
Funding:
None; Competing interest: None stated.
REFERENCES
1.
Keesara, S, Jonas A, Schulman K. Covid-19 and health
care’s digital revolution. N Engl J Med. 2020;382:e82.
Accessed April 10, 2020.
2.
Board of Governors. Telemedicine Practice Guidelines
Enabling Registered Medical Practitioners to Provide
Healthcare Using Telemedicine. Available from:
https://www.Mohfw.gov.in/pdf/telemedicine. Accessed April
5, 2020.
3.
Burke B, Hall R. Telemedicine: Pediatric applications.
Pediatrics. 2015;136:e293-e308
4.
Aggarwal KK. Prescription sans diagnosis: A case of
culpable neglect. India Legal. Available from:
https://www.indialegallive.com-ConstitutionalNews–Courts.
Accessed April 8, 2020.
5.
Lakhe A, Sodhi I, Warrier J, Sinha V. Development of
digital stethoscope for telemedicine. J Med Eng Technol.
2016;40:20-24.
6.
Arumugham S, Rajagopalan S, Rayappan JBB, Amirtharajan
R. Networked medical data sharing on secure medium - A web
publishing mode for DICOM viewer with three layer
authentication. J Biomed Inform. 2018;86:90-105.
7.
Luz PLD. Telemedicine and the doctor/patient
relationship. Arq Bras Cardiol. 2019;113:100-2.
8.
Village Resource Centre - ISRO [Internet]. 2020.
Available from:
https://www.isro.gov.in/applications/village-resource-centre.
Accessed April 18, 2020.
9.
Kittleson MM. The
invisible hand - medical care during the pandemic. N Engl J
Med. 2020; 382:1586-87.

