|
|
|
Indian Pediatr 2020;57: 619-624 |
 |
Effectiveness of Presumptive Treatment of Acute Febrile Illness With Doxycycline or Azithromycin in Preventing Acute Encephalitis Syndrome in Gorakhpur, India: A Cohort Study
|
|
Jeromie Wesley Vivian Thangaraj1, Kamran Zaman2, Vishal Shete1, Ashok Kumar Pandey2, Saravanakumar Velusamy1, Avinash Deoshatwar3, Mahima Mittal4, Nivedita Gupta5 and
Manoj Murhekar1
From 1ICMR-National Institute of Epidemiology, Chennai; 2ICMR- Regional Medical Research Centre, Gorakhpur; 3ICMR- National Institute of Virology, Pune; 4Baba Raghav Das Medical College, Gorakhpur; and India and 5Indian Council of Medical Research, (ICMR), New Delhi; India.
Correspondence to: Dr Manoj Murhekar, ICMR- National Institute of Epidemiology, Chennai, India.
Email: [email protected]
Received: April 06, 2019;
Initial review: July 13, 2019;
Accepted: January 28, 2020.
Published Online: March 12, 2020;
PII:S097475591600150
|
|
Objective: To estimate effectiveness of presumptive doxycycline or azithromycin treatment in preventing progression of Acute Febrile Illness to Acute Encephalitis Syndrome in Gorakhpur.
Study Design: Prospective cohort study.
Study Setting: Primary healthcare centers and Community healthcare centers of Gorakhpur district, Uttar Pradesh.
Participants: Children aged 1 year to less than 15 years with fever of 3 days to less than 15 days duration attending three selected peripheral health facilities in Gorakhpur during August to October, 2018.
Procedure: 35 medical officers in three selected Primary Healthcare Centers/Community Healthcare centers were sensitized on the treatment strategy. After sensitization, study participants were enrolled and information about prescription of doxycycline or azithromycin was collected. Participants were telephonically followed-up to know their progression status from AFI to AES.
Main outcome measure: Incidence of acute encephalitis syndrome among acute failure illness patients who received presumptive doxycycline or azithromycin treatment and those who did not receive this treatment.
Results: Of the enrolled 930 AFI patients, 801 (86%) were prescribed doxycycline or azithromycin and 725 (78%) could be telephonically followed-up. Progression to acute encephalitis syndrome was seen in 6 of the 621 patients who received presumptive treatment, and 5 of the 104 who did not receive the treatment. The relative risk of developing acute encephalitis syndrome among acute febrile illness patients who were prescribed presumptive treatment with doxycycline or azithromycin was 0.20 (95% CI: 0.06-0.65). The effectiveness of presumptive treatment with doxycycline or azithromycin strategy was 79.9% (95% CI: 35.4-94).
Conclusion: PDA treatment to children presenting with fever in peripheral health facilities of the study blocks in Gorakhpur during August-November, 2018 had good effectiveness in preventing progression of acute febrile illness to acute encephalitis syndrome.
Keywords: Acute undifferentiated febrile illness, Japanese encephalitis, Management, Scrub typhus.
|
Seasonal outbreaks of acute encephalitis syndrome (AES) have been occurring in four districts of Gorakhpur and three districts of Basti division of Uttar Pradesh, India since last four decades [1-3]. These outbreaks occur during monsoon and post monsoon season every year, with cases peaking during August and September before declining in late November. Outbreaks predominantly affect children aged less than 15 years and are associated with high case fatality ratios, ranging between 15 to 25% [3,4]. Japanese encephalitis accounts for less than 10% of AES cases, while the etiology of remaining AES cases remained largely unknown [5]. Studies conducted during 2014–2017 outbreaks revealed presence of IgM antibodies against Orientia tsutsugamushi (OT) in about two thirds of AES cases, suggesting scrub typhus as the major etiology of AES outbreaks [6-9]. Entomological studies have also confirmed transmission of scrub typhus pathogen in this region [10].
Most scrub typhus infections are subclinical, only a few children develop febrile illness and a small proportion of these patients develop neurological manifestations [9,11]. Hence, early administration of appropriate antibiotics is crucial in preventing progression of acute febrile illness (AFI) due to scrub typhus to AES. Based on the epidemiological, serological and entomological findings, the Indian Council of Medical Research (ICMR), in consultation with various stakeholders, developed strategies for prevention and control of AES for each tier of health care system, focusing on early diagnosis based on clinical as well laboratory investigations and appropriate treatment with doxycycline or azithromycin (ICMR, Unpublished document). For peripheral health facilities, the recommended strategy is to investigate AFI patient for various etiologies including JEV, dengue, scrub typhus, leptospirosis and malaria as per feasibility and treat appropriately. If facilities for laboratory investigations are not available, which is the case in most peripheral facilities in Gorakhpur division, it was recommended that patients presenting with fever of three or more days duration during August-November (when AES cases peak) be presumptively treated with either doxycycline or azithromycin, based on clinical suspicion. In 2016, Government of Uttar Pradesh issued guidelines to the health facilities of districts in Gorakhpur division for this presumptive treatment [12]. We conducted this study in selected peripheral health facilities in Gorakhpur district during an outbreak season in 2018 to estimate the effectiveness of presumptive doxycycline or azithromycin (PDA) treatment strategy in preventing progression of acute febrile illness to AES.
Methods
We conducted the study in three blocks (administrative subunit) viz, Bhathat, Campierganj and Jangal Kaudia in Gorakhpur district. As per the AES surveillance data from the BRD Medical College, Gorakhpur, these blocks, together accounted for 17% of the AES patients reported from Gorakhpur division during 2016-2017. The primary health care in these blocks is delivered through three community health centers (CHCs), 9 primary health centers (PHCs) and 82 health sub-centers (HSCs), whereas the district hospital, Gorakhpur and BRD Medical College, Gorakhpur, respectively are the secondary-care and tertiary-care hospitals in public sector in the district.
We sensitized 35 Medical Officers (including three pediatricians) and seven pharmacists from all the primary/community health centers in the three blocks about etiology of AES in the region. We planned the sensitization meetings separately in each of the three study sites. We sensitized the medical officers in a face-to-face two hour training session, explaining the AES scenario in Gorakhpur division, findings of investigations conducted to know the etiology of AES in Gorakhpur, and the rationale for the presumptive treatment along with treatment algorithm for management of AFI including dosage of doxycycline or azithromycin by weight as by well as age. The recommended dosage was 4.5 mg/kg/day in two divided doses for five days for doxycycline and 10 mg/kg/day in single dose for five days for Azithromycin [13]. Other than sensitization of Medical Officers about the PDA treatment strategy, the study team did not influence the prescription pattern.
The Institutional Ethics Committee of the ICMR-National Institute of Epidemiology, Chennai approved the study protocol. We enrolled all patients aged between 1 to less than 15 years with fever of three or more days to less than 15 days (Acute febrile illness, AFI) duration presenting to the outpatient departments of the selected health facilities. All AFI patients were referred to the study team stationed at the PHCs/CHCs, after they had completed the consultation with medical officers and had received the prescribed medicine at the pharmacy. We enrolled AFI patients after taking informed written consent from their accompanying caregivers. We collected their demographic information and clinical details. We abstracted information about prescription of doxycycline or azithromycin from the medical prescription, and whether the drug was dispensed. We telephonically followed-up AFI patients three days and five days after attending the health facility to collect information about consumption of doxycycline or azithromycin, and their clinical status including recovery, and improvement or worsening of clinical condition. For children who did not improve or recover, we continued the follow-up beyond day 5.
AFI patients with change in mental status (including symptoms such as confusion, disorientation, coma, or inability to talk), and new onset of seizures (excluding simple febrile seizures) were considered as patients of AES [14]. For children who progressed to AES, we collected information about the new symptoms and treatment sought including hospitalization. We visited all patients who were hospitalized, collected information about their clinical and laboratory investigations. These patients was and sera were tested for presence of immunoglobulin M antibodies against O. tsutsugamushi using commercial ELISA (Scrub Typhus Detect, Inbios International Inc, Seattle, USA).
Statistical analysis: We compared the incidence of AES among AFI patients who received PDA treatment with that of AFI patients who did not receive PDA, by calculating the relative risk (RR) and its 95% confidence interval (CI). The effectiveness of PDA treatment strategy was calculated by 1-RR formula [15]. We also calculated relative risk of developing AES among Acute undifferentiated febrile illness (AUFI) patients who were prescribed PDA. We conducted sensitivity analysis to account for uncertainty of the outcomes among AFI patients who could not be followed up. We considered three assumptions: (a) incidence of AES among patients who received and who did not receive PDA treatment was same, as found in our study, (b) none of the patients lost to follow-up progressed to AES, and (c) all patients lost to follow-up progressed to AES.
RESULTS
During August to October, 2018, we enrolled 930 AFI patients from three health facilities in the study. Of these, 560 (60%) had consulted a private practitioner before attending the public health facility. Majority (83%) of them had visited traditional healers in their nearby villages for the initial febrile illness episode. At public health facilities, 801 (86%) were prescribed doxycycline or azithromycin.
The mean age of AFI patients who received doxycycline or azithromycin was higher than those who did not receive doxycycline or azithromycin (7.5 vs 6.2 years, P=0.001). The median duration of fever in both the groups was 5 days (Inter-quartile range 4-7 days). The proportion of AFI patients who were prescribed PDA ranged between 76.4% (Campierganj) to 92.7% (Jangal Kaudiya).
We could telephonically follow-up 725 (78%) AFI patients. Of these, 621 (85.6 %) had received doxycycline or azithromycin treatment –489 (78.7%) received azithromycin and 132 (21.3%) received doxycycline (Fig. 1). The remaining 97 (13.4%) received other antibiotics (fluoroquinolones, 41, penicillin derivatives 31; cephalosporin, 13; and sulfonamide, 12) while 7 (1%) did not receive any antibiotics.
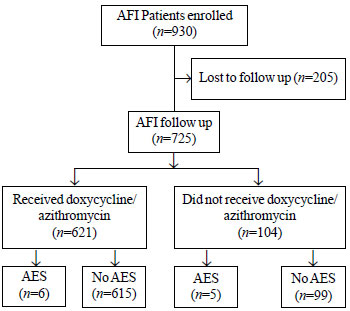 |
| Fig. 1 Flowchart showing acute febrile illness (AFI) patients enrolled and those developing acute encephalitis syndrome (AES) |
Six of the 621 AFI patients who received PDA treatment and five of the 104 who did not receive PDA treatment progressed to AES (cumulative incidence 0.96% and 4.8%, respectively). The relative risk (95% CI) of developing AES among AFI patients who were prescribed PDA treatment was 0.20 (0.06-0.65). The age adjusted relative risk (95% CI) was 0.19 (0.06-0.62). The effectiveness of PDA treatment strategy was 79.9% (95% CI: 35.4–94). Two of the six AES patients who received PDA treatment and three of the five AES patients who did not receive PDA treatment had IgM antibodies against O. tsutsugamushi.
Of the 725 AFI patients, 454 had focal symptoms such as cough, abdominal pain, loose stools, burning micturition. The remaining 271 were considered as acute undifferentiated febrile illness (AUFI). Among the 271 AUFI patients, 236 (87.1%) were prescribed PDA. Three of the 236 AUFI patients who received PDA treatment and three of the 35 who did not receive PDA treatment progressed to AES. The relative risk (95% CI) of developing AES among AUFI patients who were prescribed PDA treatment was 0.14 (0.03-0.70).
The results of sensitivity analysis as per assumptions regarding AFI patients lost to follow-up is shown in Table I.
DISCUSSION
The findings of our study indicate that PDA treatment to children with AFI attending peripheral health facilities was effective in preventing progression of AFI to AES. Several studies also strongly recommend presumptive/empiric treatment with either Doxycycline or Azithromycin, where Scrub Typhus is endemic to minimize risk of death and severity of the disease [16-19]. Untreated AFI due to Scrub Typhus progress to AES by vascular injury to meninges [20]. Central nervous system involvement occurs as a part of systemic infection. Pathogen factors like strain type and evolution of the organism to escape host immune systems might also contribute towards progression of illness [21-24]. There were several reasons for considering presumptive treatment of AFI patients with doxycycline or azithromycin in Gorakhpur division. This includes lack of laboratory facilities for diagnosis of scrub typhus infection at primary care facilities. Moreover, serological tests for diagnosis becomes positive only around 5-7 days [25-27]. Other reasons include significant proportion of scrub typhus among the AFI patients, distinct seasonality of the disease during post-monsoon months, risk of progression of AFI patients to AES which is associated with high case fatality, and over-burdened public health facilities. Overreliance on traditional healers in rural areas results in delay in reporting to public health facilities. There are very few studies which have attempted to estimate the effectiveness of the presumptive treatment with either doxycycline or azithromycin among AFI patients. In a study by Phimda, et al. [28], both doxycycline and azithromycin given empirically to adult patients with AUFI, were found to be highly effective with success rates of 96.5% and 97.4%, respectively.
In our study, azithromycin was prescribed more frequently than doxycycline by medical officers. This could be due to hesitancy among medical officers to prescribe doxycycline among young children as well as lack of drug supply. DHR-ICMR guidelines recommend doxycycline as one of the most effective antibiotics for the treatment of suspected rickettsial infections in India [13]. Also short course (<10 days) of doxycycline treatment is not associated with any increased risk of dental staining, enamel hypoplasia, or tooth color differences [29].
Our study has certain limitations. First, we followed up AFI patients telephonically and not by house to house visits. We therefore had to rely on parents’ responses about treatment. Parents of all the 725 children informed that their children had consumed doxycycline or azithromycin in the prescribed doses. Second, we did not test AFI patients for scrub typhus etiology. This would have provided accurate information about incidence of AES among scrub typhus positive patients. Third, we could not follow-up 23% AFI patients who received PDA treatment and 19% patients who did not receive PDA treatment. Patients were considered lost to follow up only when we were not able to contact patients either at day 3 or day 5 or beyond. We conducted a sensitivity analysis to account for uncertainty of the outcomes among patients who were lost to follow-up. Of the three assumptions, two assumptions indicated a protective effect for PDA treatment strategy, while the third assumption was remotely possible. Fourth, since PDA has been recommended for AFI patients in public health facilities and already been rolled out, it was not possible to evaluate its efficacy using a clinical trial design.
Prescribing doxycycline or azithromycin presumptively, to children presenting with fever in peripheral health facilities between August and October could reduce AES burden by preventing progression of AFI to AES. The Government of Uttar Pradesh has already issued guidelines to district and block medical officers to prescribe Doxycycline or Azithromycin to AFI patients attending peripheral health facilities of Gorakhpur and Basti divisions. However, the strategy needs to be strengthened at the block level. The medical officers have to be repeatedly sensitized on rationale for PDA treatment among suspected scrub typhus patients. A close monitoring of implementation of this strategy, monitoring resistance to these antimicrobials, and ensuring adequate supply of doxycycline and azithromycin would yield higher compliance on PDA treatment strategy by the medical officers. Further, significant reduction in the disease burden due to AES in the region would require sensitizing doctors in private sector as well.
Ethical clearance: Institutional Ethics Committee of ICMR- National Institute of Epidemiology, Chennai; NIE/IHEC/201507-01, dated 18 July, 2018.
Acknowledgement: Mr Kaushik Kumar for support in data collection.
Contributors: JWVT, NG, MM, MVM: conceived and designed the study; VS, AP, AD: collected data; KZ, AP: conducted laboratory investigations; SV, JWVT: analyzed the data; JWVT, MVM: prepared the first draft of the manuscript; KZ, VS, AP, SV, AD, MM, NG: provided critical inputs to revise the manuscript. All authors read and approved the final version of the manuscript.
Funding: Indian Council of Medical Research, New Delhi
Competing interest: None stated.
What is Already Known?
• Treatment with doxycycline or azithromycin is effective in the treatment of rickettsial infections.
What This Study Adds?
• Presumptive doxycycline or azithromycin was effective in preventing progression of patients with acute febrile illness as well as acute undifferentiated febrile illness to acute encephalitis syndrome in Gorakhpur, India. |
References
- Mathur A, Chaturvedi UC, Tandon HO, Agarwal AK, Mathur GP, Nag D, et al. Japanese encephalitis epidemic in Uttar Pradesh, India during 1978. Indian J Med Res. 1982;75:161-9.
- Rathi AK, Kushwaha KP, Singh YD, Singh J, Sirohi R, Singh RK, et al. JE virus encephalitis: 1988 epidemic at Gorakhpur. Indian Pediatr. 1993;30:325–33.
- Mittal M, Kushwaha KP. AES: Clinical presentation and dilemmas in critical care management. Commun Dis. 2014;46:50-65.
- Kakkar M, Rogawski ET, Abbas SS, Chaturvedi S, Dhole TN, Hossain SS, et al. Acute encephalitis syndrome surveillance, Kushinagar district, Uttar pradesh, India. 2011-2012. Emerg Infect Dis. 2013;19:1361-9.
- Ranjan P, Gore M, Selvaraju S, Kushwaha KP, Srivastava DK, Murhekar M. Changes in acute encephalitis syndrome incidence after introduction of Japanese encephalitis vaccine in a region of India. J. Infect. 2014;69:200-2.
- Murhekar MV, Mittal M, Prakash JAJ, Pillai VM, Mittal M, Kumar CG, et al. Acute encephalitis syndrome in Gorakhpur, Uttar Pradesh, India–Role of scrub typhus. J. Infect. 2016;73:623-6.
- Mittal M, Bondre V, Murhekar M, Deval H, Rose W, Verghese V, et al. Acute encephalitis syndrome in Gorakhpur, Uttar Pradesh, 2016: Clinical and laboratory findings. Pediatr Infect Dis J. 2018;37:1101-6.
- Mittal M, Thangaraj JWV, Rose W, Verghese VP, Kumar CG, Mittal M, et al. Scrub typhus as a cause of acute encephalitis syndrome, Gorakhpur, Uttar Pradesh, India. Emerg Infect Dis. 2017;23:1414.
- Thangaraj JWV, Mittal M, Verghese VP, Kumar CG, Rose W, Sabarinathan R, et al. Scrub typhus as an etiology of acute febrile illness in Gorakhpur, Uttar Pradesh, India, 2016. Am J Trop Med Hyg. 2017;97:1313-5.
- Sadanandane C, Jambulingam P, Paily KP, Kumar NP, Elango A, Mary KA, et al. Occurrence of Orientia tsutsugamushi, the etiological agent of scrub typhus in animal hosts and mite vectors in areas reporting human cases of acute encephalitis syndrome in the Gorakhpur region of Uttar Pradesh, India. Vector Borne Zoonotic Dis. 2018 17;10:539-547.
- Thangaraj JWV, Vasanthapuram R, Machado L, Arunkumar G, Sodha SV, Zaman K, et al. Risk factors for acquiring scrub typhus among children in Deoria and Gorakhpur districts, Uttar Pradesh, India, 2017. Emerg Infect Dis. 2018;24:2364-7.
- Govt of Uttar Pradesh. AES/JE control strategy. Treatment with Doxycycline/Azithromycin. 21/F/S.NO/AES/JE/2016/2044-49. 2016.
- Rahi M, Gupte MD, Bhargava A, Varghese GM, Arora R. DHR-ICMR Guidelines for Diagnosis and Management of Rickettsial Diseases in India. Indian J Med Res. 2015;141:417-22.
- World Health Organization. Acute Encephalitis Syndrome. Japanese Encephalitis Surveillance Standards. January 2006. From WHO-Recommended standards for Surveillance of Selected Vaccine-preventable Diseases. WHO/V&B/03.01 [Internet]. World Health Organization; 2006. Available from: http://apps.who.int/iris/bitstream/10665/68334/1/ WHO_V-B_03.01_eng. pdf. Accessed on 15th February 2019.
- Orenstein WA, Bernier RH, Dondero TJ, Hinman AR, Marks JS, Bart KJ, et al. Field evaluation of vaccine efficacy. Bull World Health Organ. 1985;63:1055-68.
- Mayxay M, Castonguay-Vanier J, Chansamouth V, Dubot-Pérès A, Paris DH, Phetsouvanh R, et al. Causes of non-malarial fever in Laos: A prospective study. Lancet Glob Health. 2013 ;1: e46-54.
- Phongmany S, Rolain J-M, Phetsouvanh R, Blacksell SD, Soukkhaseum V, Rasachack B, et al. Rickettsial infections and fever, Vientiane, Laos. Emerg Infect Dis. 2006;12: 256-62.
- Luvira V, Silachamroon U, Piyaphanee W, Lawpoolsri S, Chierakul W, Leaungwutiwong P, et al. Etiologies of acute undifferentiated febrile illness in Bangkok, Thailand. Am J Trop Med Hyg. 2019;100:622-9.
- McGready R, Ashley EA, Wuthiekanun V, Tan SO, Piman-panarak M, Viladpai-nguen SJ, et al. Arthropod borne disease: The leading cause of fever in pregnancy on the Thai-Burmese border. PLoS Negl Trop Dis. 2010;4. e888.
- Peter JV, Sudarsan TI, Prakash JAJ, Varghese GM. Severe scrub typhus infection: Clinical features, diagnostic challenges and management. World J Crit Care Med. 2015;4:244-50.
- Rajapakse S, Rodrigo C, Fernando D. Scrub typhus: pathophysiology, clinical manifestations and prognosis. Asian Pac J Trop Med. 2012;5:261-4.
- Jeong YJ, Kim S, Wook YD, Lee JW, Kim K-I, Lee SH. Scrub typhus: Clinical, pathologic, and imaging findings. Radiographics. 2007;27:161-72.
- Cho N-H, Choi C-Y, Seong S-Y. Down-regulation of gp96 by Orientia tsutsugamushi. Microbiol Immunol. 2004;48:297-305.
- Mahajan SK, Rolain J-M, Kanga A, Raoult D. Scrub typhus involving central nervous system, India, 2004–2006. Emerg Infect Dis. 2010;16:1641-3.
- Kim DM, Lee Y-M, Back J-H, Yang TY, Lee JH, Song H-J, et al. A serosurvey of Orientia tsutsugamushi from patients with scrub typhus. Clin Microbiol Infect. 2010;16:447-51.
- Ching WM, Wang H, Eamsila C, Kelly DJ, Dasch GA. Expression and refolding of truncated recombinant major outer membrane protein antigen (r56) of Orientia tsutsugamushi and its use in enzyme-linked immunosorbent assays. Clin Diagn Lab Immunol. 1998;5:519-26.
- Varghese GM, Rajagopal VM, Trowbridge P, Purushothaman D, Martin SJ. Kinetics of IgM and IgG antibodies after scrub typhus infection and the clinical implications. Int J Infect Dis. 2018;71:53-5.
- Phimda K, Hoontrakul S, Suttinont C, Chareonwat S, Losuwanaluk K, Chueasuwanchai S, et al. Doxycycline versus azithromycin for treatment of leptospirosis and scrub typhus. Antimicrob Agent Chemother. 2007;51: 3259-63.
- Todd SR, Dahlgren FS, Traeger MS, Beltrán-Aguilar ED, Marianos DW, Hamilton C, et al. No visible dental staining in children treated with doxycycline for suspected Rocky Mountain Spotted Fever. J Pediatr.2015;166:1246-51.
|
|
|
 |
|

