|
|
|
Indian Pediatr 2018;55: 568-572 |
 |
Comparison of Three Nursing Positions for
Reducing Gastric Residuals in Preterm Neonates:
A Randomized Crossover Trial
|
|
Varanpal Kaur 1,
Rupinder Kaur1
and Shiv Sajan Saini2
From Departments of 1Nursing and
2Pediatrics, PGIMER, Chandigarh, India.
Correspondence to: Dr Shiv Sajan Saini,
Assistant Professor, Department of Pediatrics, PGIMER, Chandigarh,
India. 160012. Email:
[email protected]
Received: July 06, 2017;
Initial review: October 09, 2017;
Accepted: April 07, 2018.
|
|
Objective: To compare left lateral, right lateral, and prone nursing
positions of neonate for reducing pre-feed gastric residuals among
£34
weeks neonates.
Design: Randomized crossover
trial.
Setting: Level-III NICU.
Participants: Neonates
£34
weeks, receiving 50-150 mL/kg/day feeds through oro-gastric route.
Intervention: Neonates were
randomized to left lateral, right lateral and prone positions.
Intervention position was given for eight hours (4 feeds, 9AM to 5PM)
followed by a wash-off period of 16 hours. After 24 hours, each neonate
crossed over to next position as per randomization card to complete
three positions in three consecutive days. Gastric residuals were
collected just before next feed.
Main outcome: Pre-feed
gastric residuals.
Results: Sixty three
neonates were randomized. Fewer neonates in right lateral position had
gastric residuals compared to left lateral position [OR 0.09 (95% CI
0.04, 0.21), P<0.001]. Neonates in right lateral and prone
positions had comparable gastric residuals [OR 0.90 (95% CI 0.36, 2.22),
P=0.82]. Gastric residuals, as a proportion of last feed, were
highest in left lateral [6% (2, 10), maximum 28%] position.
Significantly higher proportion of neonates in right lateral position
had episodes of regurgitation compared to other positions. Oxygen
saturation, heart rate, time to full feeds and duration of hospital stay
were comparable in the three groups.
Conclusions: Left lateral
position was associated with higher but clinically non-significant
pre-feed gastric residuals as compared to right lateral position. Right
lateral position was associated with significantly increased
regurgitation episodes.
Keywords: Desaturation, Left
lateral position, Prone position, Right lateral position.
Trial Registration: CTRI/2015/06/005895.
|
|
O
ptimum nursing position in neonates receiving
enteral nutrition is unknown [1]. Enteral feeding in preterm neonates is
challenging due to immaturity of bowel function, which is frequently
associated with pre-feed gastric residuals, disruption of enteral feeds,
delayed attainment of full enteral feeding, and prolonged hospital stay
[2]. In addition to biological factors such as decreased intestinal
motility, decreased gastrointestinal hormones and enzymes, nursing
position is an important contributory factor for gastric residuals in
neonates [3].
Four nursing positions – supine position, left
lateral (LL), right lateral (RL) and prone positions (PP) – are
described in neonates [1,4-6]. There are limited studies which have
compared these positions. Among all nursing positions, supine position
is associated with increased gastric residuals and gastro-esophageal
reflux (GER) [5-8]. RL position is favoured as it is associated with
less gastric residuals and faster gastric emptying [1]; however, it is
associated with increased GER [9,10]. Additionally, RL, LL and PP have
not been evaluated for relevant clinical outcomes (e.g. episodes
of regurgitation, desaturation, vital signs, oxygenation status, time to
full feeds etc) [4-6]. Furthermore, previous studies comparing these
positions have enrolled convenient sample sizes. Hence, there is
considerable equipoise regarding the ideal nursing position in neonates.
We planned this study to compare LL, RL and PP nursing positions for
pre-feed gastric residuals among preterm neonates
£34 weeks, receiving
enteral feeding.
Methods
We conducted this randomized, open-labelled, active
control, double cross-over trial from July 2014 to March 2015 in a
level-III NICU of a tertiary care referral teaching Institute of
Northern India. We obtained ethical clearance from the Institute’s
Ethics Committee.
We enrolled preterm neonates ( £34
weeks) receiving 50-150 mL/kg/day enteral feeding. We excluded neonates
who required continuous positive airway pressure, mechanical
ventilation, vasoactive drugs, had lethal congenital malformations, or
previously diagnosed definite necrotizing enterocolitis (NEC). We
obtained a informed written consent from one of the parents before
enrolment.
We generated random sequence from the website ‘www.randomizer.org’.
We used stratified and block randomization. Stratification was done for
the following gestational ages 26 0/7-296/7
weeks, 300/7-316/7
weeks and 320/7-340/7
weeks. Each stratum had permuted, randomly varying
block sizes of 6 or 9. The study investigator, who generated random
sequence and prepared envelops, did not participate in patient
recruitment and management. We achieved allocation concealment by
serially numbered, sealed brown opaque envelopes technique.
Among neonates with gestational age <30 wks, feeding
was initiated with 10-20 mL/kg/d gavage feeds within 24 hours of birth,
and advanced by 20 mL/kg/d. For 30-31 wks of gestation, feeding was
started at 40 mL/kg/d by gavage feeds and advanced every 4 hourly by 2
mL/kg to make to 80 mL/kg/d by the end of 24 hours. For 32-34 wks of
gestation, full enteral feed was started at 60 mL/kg/d by cup and spoon
on day 1. The feeds were given at 2-hourly interval and advanced at 20
mL/kg/d to reach 180 mL/kg/d by day 6-8. Expressed breast milk (EBM) is
aggressively promoted in our unit followed by preterm formula, in case
of non-availability of EBM. If the neonates had gastric residuals upto
33% of the previous feed volume (feed volume
³6 mL), the residuals
were re-fed and next scheduled feed was given in addition, provided the
abdominal examination was normal. If the gastric residuals were 33-50%
of the previous feed volume and the abdominal examination was normal,
the residuals were re-fed along with the feed volume equal to the
difference of scheduled feed and volume of gastric residuals. However,
if the residuals were >50% of last feed volume, the feeds were stopped.
The period of data collection was from July to
September, 2014. The neonates were randomly assigned to three nursing
positions i.e. LL, RL and PP in double cross-over fashion for
three consecutive days. Each position was given for eight hours (morning
9 AM till 5 PM). Four feeds were studied over an 8-hour observation
period. It was followed by a wash-off period of 16 hours, during which
neonates were nursed predominantly in supine position. Next day the baby
was crossed over to subsequent position according to randomisation card.
Thus each neonate was studied for all three positions on three
consecutive days. Pre-feed gastric residuals were measured before each
feed using 2 mL disposable syringe and plunger of the syringe was pulled
gently over 3-5 seconds. We secured a 6-Fr oro-gastric tube in all
neonates for measurement of gastric aspirates irrespective of method of
feeding. Even neonates, who qualified for spoon/ cup feeds, had oro-gastric
tube in situ during 3 days of intervention nursing positions.
Number of feed regurgitations and episodes of desaturations over an
eight-hour observation period were recorded. Regurgitation was defined
as the passage of small amount (clinically judged to be 1-2 teaspoonful)
of fresh or curdled milk, in presence of normal abdominal examination
findings. Desaturation was defined as any SpO 2
value falling below 87%, which could not be explained by mechanical
reasons or artefacts. Immediately after giving feeds, heart rate and
oxygen saturation was recorded at every three minutes interval for first
30 minutes (total 10 observations after every feed). An average of heart
rate and oxygen saturation of 40 such observations, over 8 hours study
period, was recorded for each nursing position. All neonates were
followed up till they reached full feeds (180 ml/kg/day). The duration
of hospital stay of these neonates was recorded.
Our primary outcome was presence of pre-feed gastric
residuals. Our secondary outcomes were: amount of pre-feed residuals,
incidence of feed regurgitations, incidence of desaturations, average
heart rate and SpO 2 over
8-hr observation period, postnatal age to reach full feeds (180 mL/kg/day)
and length of hospital stay.
We planned this study of matched sets of neonates to
receive three nursing positions. Prior data indicated that the
probability of residuals in LL is 0.5 and the correlation coefficient
for exposure between matched interventions is 0.2 [5]. Considering odds
ratio for gastric residuals in RL and PP relative to LL as 0.3, we
needed to study 65 experimental subjects to be able to reject the null
hypothesis with probability (power) 0.8 and Type-1 error 0.05.
Statistical analysis: The amount of
pre-feed gastric residuals was compared with Friedman’s two way analysis
of variance by ranks. Number of feed regurgitations, episodes of
desaturations in 8-hr period, average heart rate and SpO 2,
time to reach full feeds and length of hospital stay were compared
between three positions by using Friedman’s test or Repeated measures
analysis of variance, wherever applicable. The categorical variables
were compared between three positions by Cochran-Q test. A P
value of <0.05 was taken as significant. Analysis was done using
statistical software packages SPSS version 20.0. (IBM, New York)
Results
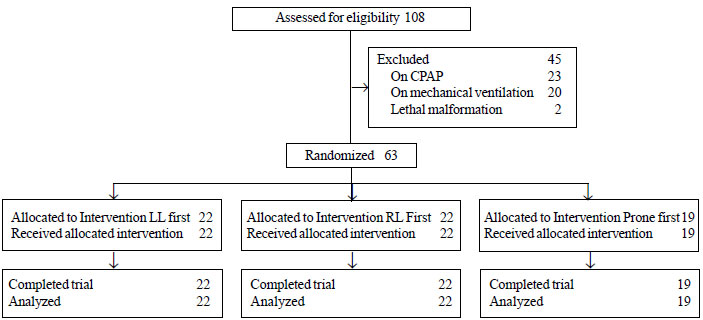
We recruited 63 neonates during the study period (Fig.1).
These neonates were randomized in three positions: LL (n=19), RL
(n=22) and PP (n=22). Each neonate completed all three
positions. The baseline characteristics of all study neonates are
presented in Table I.
 |
|
Fig. 1 Study flow diagram.
|
TABLE I Baseline Characteristics of Enrolled Neonates
|
Characteristics |
Number (%) |
|
Gestational age (wk), mean (SD) |
31 (2) |
|
Birthweight (g), mean (SD) |
1272 (307) |
|
Length (cm), mean (SD) |
39 (3) |
|
Head circumference (cm), mean (SD) |
27 (2) |
|
Postnatal age (d), median (IQR) |
6 (4, 10) |
|
Male gender (%) |
39 (62) |
|
Small for gestational age (%) |
22 (35) |
|
Antenatal steroids (%) |
51 (81) |
|
Maternal PIH (%) |
22 (35) |
|
Absent/reverse end diastolic flow in umbilical artery (%) |
1 |
|
Premature rupture of membranes (%) |
22 (40) |
|
Chorioamnionitis (%) |
1 (2)
|
|
Caesarean section (%) |
30 (48) |
The proportion of neonates, who received exclusive
EBM, was above 90% in all the groups (Table II). Although
pre-feed aspirates was recorded in 25% of all study neonates, its
quantity was <33% of last feed volume. Abdominal examination of all the
neonates was normal (Table II).
TABLE II Feeding and Abdominal Characteristics of Neonates During Each Intervention Period (N=63)
|
Characteristics |
Left Lateral
|
Right Lateral
|
Prone
|
Pvalue |
|
Amount of feeds (mL/kg/d), median (IQR) |
123 (89, 155) |
121 (89, 149) |
116 (88, 151) |
0.7 |
|
Abdominal girth (cm) , median (IQR) |
21 (21, 23) |
21 (21, 23) |
22 (20, 22) |
0.7 |
|
No. of stools in past 8 h, median (IQR)
|
2 (1, 2) |
2 (1, 2) |
2 (1, 2) |
1.0 |
|
Exclusive expressed breastmilk, n (%) |
58 (92) |
58 (92) |
57 (91) |
0.6 |
|
Orogastric feeds, n (%)
|
62 (98) |
63 (100) |
63 (100) |
0.4 |
The proportion of neonates having gastric residuals
were maximum in LL followed by prone and least in RL position. The odds
of having gastric residuals in RL position were significantly less as
compared to LL [30% vs 83%; OR (95% CI), 0.09 (0.04, 0.21); P
<0.001] whereas odds of having gastric residuals in PP position were
similar to LL [51% vs 30%; OR (95% CI), 0.90 (0.36, 2.22);
P=0.82]. The amount of gastric residuals as a proportion of last feed,
was highest for LL followed by PP and least in RL, the differences were
statistically significant P<0.001 (Table III). No
neonate required interruption in feeding because of gastric residuals
during the study period. Significantly higher proportion of neonates in
RL position had episodes of regurgitation (Table III). LL,
RL and PP were comparable for neonates having desaturations, average
oxygen saturation, and average heart rate observed over study period.
The time to reach full feeds and duration of hospital stay was also
comparable in three groups (Table III).
TABLE III Outcomes in Neonates Nursed in Different Positions (N=63)
|
Characteristics |
Left Lateral
|
Right Lateral
|
Prone
|
Pvalue |
|
Amount of gastric residuals (%)#$
|
6 (2, 10) |
0 (0, 1) |
1 (0, 3) |
<0.001 |
|
Neonates having regurgitation (%) |
1 (2) |
21 (33) |
1 (2) |
<0.001 |
|
Neonates having desaturations (%) |
4 (6) |
5 (8) |
10 (16) |
0.161 |
|
Episodes of desaturations in 8 hr# |
0 (0, 0) |
0 (0, 0) |
0 (0, 0) |
0.249 |
|
SpO2 during observation period (%)* |
98 (2) |
97 (2) |
97 (2) |
0.074 |
|
Heart rate during observation period (beats/min)* |
153 (9) |
154 (10) |
154 (11) |
0.878 |
|
Age of reaching full feeds (d) # |
9 (7, 15) |
10 (8, 14) |
10 (8, 14) |
0.641 |
|
Duration of hospital stay (d)* |
22 (7) |
30 (12) |
30 (14) |
0.162 |
|
Data as *mean (SD) or #median (IQR); $as
a proportion of last feed. |
Discussion
In this study, RL and prone positions were associated
with a significantly lower incidence of gastric residuals as com-pared
to LL position. In contrast, RL position was associated with increased
episodes of regurgitation as compared to LL and PP positions. Vital
signs and other clinical outcomes were comparable between the three
groups.
The limitations of the study were: GER was not
measured and hence it does not provide data for co-existing GER; the
study findings are limited to neonates
£34 weeks gestation;
and the period of observation for each position per baby was relatively
short. The gastric aspirates is at best an intermediate outcome.
Furthermore, it should not be routinely practiced as it can predispose
to gastric mucosal injury. Although we also measured clinical outcomes
like time to full feeds, duration of hospital stay, but the short period
of intervention is unlikely to affect these outcomes.
There is limited literature comparing various nursing
positions in preterm neonates [1]. Victor [6] compared gastric residuals
after 30 minutes of ‘test meal’ (10% glucose with added phenol-red )
between RL, LL, PP and supine positions [6]. The gastric emptying in LL
was significantly less compared to PP and RL. However, the study
findings are difficult to generalize as the handling of ‘test feed’ is
likely to be different from EBM/formula feeds. Moreover residuals after
30 minutes of test-feeds may not be clinically relevant [6]. Cohan,
et al. [4] have compared RL, LL, PP and supine positions in
£34 weeks
neonates [4]. The residuals after three hours of feeds were comparable
between these positions. Sanger, et al. [5] compared RL, LL, PP
and supine positions in preterm neonates 28-36 weeks for two feeds given
on day 4 of life. LL had maximum and RL had least residuals. However,
the absolute amount has not been mentioned in the study. Some authors
[7,8] have compared prone and supine positions, but did not compare
other positions.
We did not study supine position, as in previous
studies, as it was associated with increased gastric residuals and GER
as compared to other positions [5-8]. In addition, we needed a ‘neutral
position’ to be used in wash-off period. We included only preterm
neonates <34 weeks, who are more vulnerable to feed intolerance. In LL
position, the greater curvature of stomach is in dependent position and
the direction of pylorus is vertically upwards. In RL position, the
pylorus is downward which hastens gastric emptying. Therefore the
residuals are likely to be higher in LL as compared to RL position, as
was found in this study, and also reported in literature [4,6].
Nevertheless, the amount of gastric residuals was <10% of previous feed
volume in 75% of all study neonates in LL position. Conventionally
enteral feeds are continued, if the pre-feed residuals are less than 33%
of previous feed volume and abdominal examination is normal [2]. In our
study, no neonate in LL position required interruption of feeds. Hence
the difference in gastric residuals between different positions is
unlikely to be ‘clinically relevant’. In RL position, the pyloric antrum
is in dependent position, which has got a limited capacity to hold feeds
as compared to greater curvature in LL position. Furthermore there is
relative proximity of dependent part to gastro-oesophageal junction in
RL position as compared to LL. The increased risk of regurgitation in RL
position in the present study was associated with significantly
decreased gastric residuals. The relative contribution of anatomical
peculiarity and regurgitation for significantly less gastric residuals
in RL position is not clear. Nevertheless this finding is likely to be
clinically significant, as the episodes of regurgitation may lead to
aspiration and can also be associated with apnea. Our findings are in
agreement with findings of Omari, et al. [10] who showed
significantly increased incidence of gastro-oesophageal reflux in RL as
compared to LL position. Nevertheless episodes of desaturation, heart
rate and oxygen saturation were comparable in three study positions in
our study.
Although, prone position was associated with lesser
gastric residuals and less episodes of regurgitation, it is reported to
be associated with increased risk of sudden infant death syndrome, and
hence cannot be recommended [11].
To conclude, LL position was associated with
increased but clinically acceptable pre-feed gastric residuals as
compared to RL position among £34
weeks preterm neonates receiving 50-150 mL/kg/day of enteral feeding. RL
was associated with significantly increased regurgitation episodes as
compared to LL and PP.
Contributors: VK: designed the data collection
instruments, enrolled the patients, collected the data, drafted the
initial manuscript, and approved the final manuscript as submitted; RK:
helped in designing the data collection instruments, supervised the data
collection, helped in data analysis, reviewed the manuscript, and
approved the final manuscript as submitted; SSS: conceptualized and
designed the study, coordinated and supervised data collection,
performed the data analysis, critically reviewed and revised the
manuscript and approved the final manuscript as submitted
Funding: None; Competing interest: None
stated.
|
What is Already Known?
• Among preterm neonates receiving
enteral feeds, left lateral position is associated with
significantly higher gastric residuals as compared to right
lateral position.
What This Study Adds?
•
Among preterm neonates receiving enteral nutrition, left lateral
position is associated with increased yet clinically acceptable
pre-feed gastric residuals. Right lateral position was
associated with significantly increased episodes of
regurgitation as compared to left lateral position.
|
References
1. Elser HE. Positioning after feedings: what is the
evidence to reduce feeding intolerances? Adv Neonatal Care.
2012;12:172-5.
2. Ng SC, Gomez JM, Rajadurai VS, Saw SM, Quak SH.
Establishing enteral feeding in preterm infants with feeding
intolerance: A randomized controlled study of low-dose erythromycin. J
Pediatr Gastroenterol Nutr. 2003;37: 554-8.
3. Henry SM. Discerning differences: Gastroesophageal
reflux and gastroesophageal reflux disease in infants. Adv Neonatal
Care. 2004;4:235-47.
4. Cohen S, Mandel D, Mimouni FB, Solovkin L,
Dollberg S. Gastric residual in growing preterm infants: Effect of body
position. Am J Perinatol. 2004;21:163-6.
5. Sangers H, deJong PM, Mulder SE, Stigter GD, van
den Berg CM, te Pas AB, et al. Outcomes of gastric residuals
whilst feeding preterm infants in various body positions. J Neonatal
Nurs. 2013;19:337-41.
6. Victor YH. Effect of body position on gastric
emptying in the neonate. Arch Dis Child. 1975;50:500-4.
7. Chen SS, Tzeng YL, Gau BS, Kuo PC, Chen JY.
Effects of prone and supine positioning on gastric residuals in preterm
infants: A time series with cross-over study. Int J Nurs Stud.
2013;50:1459-67.
8. Malhotra AK, Deorari AK, Paul VK, Bagga A, Singh
M. Gastric residuals in preterm babies. J Trop Pediatr. 1992;38:262-4.
9. van Wijk MP, Benninga MA, Dent J, Lontis R,
Goodchild L, McCall LM, et al. Effect of body position changes on
postprandial gastroesophageal reflux and gastric emptying in the healthy
premature neonate. J Pediatr. 2007;151: 585-90.
10. Omari TI, Rommel N, Staunton E, Lontis R,
Goodchild L, Haslam RR, et al. Paradoxical impact of body
positioning on gastroesophageal reflux and gastric emptying in the
premature neonate. J Pediatr. 2004;145:194-200.
11. Task Force on Sudden Infant Death Syndrome, Moon
RY. SIDS and other sleep-related infant deaths: Expansion of
recommendations for a safe infant sleeping environment. Pediatrics.
2011;128:1030-9.
|
|
|
 |
|

