|
|
|
Indian Pediatr 2017;54:550-555 |
 |
Designing and
Validation of a Hindi-language Parent Self-report Developmental
Screening Tool
|
|
Rahul Jain, Anshita Arora, Rohit Anand, Shahzadi Malhotra, Medha Mittal
and *Monica Juneja
From Department of Pediatrics, Chacha Nehru Bal
Chikitsalaya, Geeta Colony; and *Child Development Center, Maulana Azad
Medical College and associated Lok Nayak Hospital, Bahadur Shah Zafar
Marg; New Delhi, India.
Correspondence: Dr. Rahul Jain, 61-A, DDA Flats,
Phase 1, Qutab Enclave, New Delhi 110 016, India.
Email:
drrahuljain1980@gmail.com
Received: August 21, 2016;
Initial review: November 4, 2016;
Accepted: March 30, 2017.
|
Aim: To design and validate Hindi-language parent
self-report developmental screening questionnaires for 9-month and
18-month-old Indian children.
Design: Cross-sectional study
Setting: Tertiary-care pediatric hospital from
April 2014 to March 2016
Participants: In each age group (9-month and
18-month), 45 children were enrolled for designing of questionnaires (30
for obtaining parental observations of current development and 15 for
pre-testing). For validation of tool, 100 children (60 low risk and 40
high risk) were enrolled in each age group.
Methods: For designing, observations regarding
current developmental milestones were obtained from parents and a list
of all enumerated milestones was prepared. After detailed discussion by
a team of developmental pediatricians, pediatric resident, clinical
psychologist and language specialist, milestones were chosen for
drafting of questionnaires. In each age group, drafts were pre-tested
and required modifications were done. The final questionnaires contained
20 items each to be scored on a Likert scale (total score ranging from
20 to 60, a lower score indicating a higher risk of developmental
delay). These questionnaires were validated against Developmental
Assessment Scale for Indian Infants (DASII), a gold standard instrument.
Results: On ROC analysis, the 9-month and
18-month screening tool had area under curve of 0.988 and 0.953,
respectively, for detecting developmental delay. Score
£50 on
the 9-months questionnaire had sensitivity of 100% and specificity of
87.2%. Score £49
on the 18-months questionnaire had sensitivity of 91.4% and specificity
of 88.7%.
Conclusions: The new questionnaires have a
promising role in developmental screening of children at the time of
routine immunizations in our country.
Keywords: Diagnosis, Early intervention, Identification,
Indigenous.
|
|
D
evelopmental delay is seen in upto 3% of children
younger than 5 years [1]. Early detection, followed by early
intervention have a positive impact on cognitive and motor outcomes, in
addition to enabling the families to better understand and cope up with
the condition [2-6]. Early
detection relies on continuing developmental surveillance and periodic
developmental screening by primary care physicians; however, these are
infrequently practiced. One of the major reasons behind
under-utilization of developmental screening tools is time-constraint,
as most of the tools require elicitation of the child’s skills and are
cumbersome to use [7,8].
To overcome the shortcomings of traditional screening
tools, some parent-report tools have been developed, supported by
research that showed that parents can provide accurate information about
their child’s development. Large number of studies have subsequently
confirmed that these tools are reliable and valid [9]. The available
Western tools developed in other countries can be translated in Indian
languages for use, but many of their items are culturally inappropriate,
and most of these tools are expensive to use. This study was planned to
design and validate simple, inexpensive, indigenous Hindi language
parent self-report developmental screening tool for 9- and 18-month-old
children, that can be completed during routine visits for vaccination.
Methods
This study was conducted at Chacha Nehru Bal
Chikitsalaya, a pediatric tertiary-care institute in northern India from
April 2014 to March 2016. The study protocol was approved by the
Institutional Ethical Committee of Maulana Azad Medical College. The
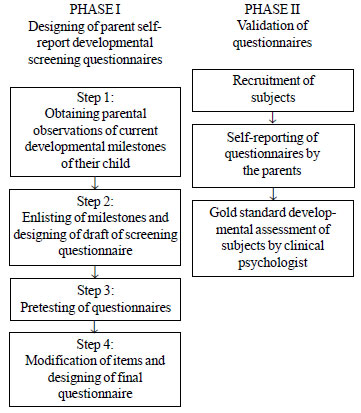
study had two phases, the first was designing of screening
questionnaires and second being validation of questionnaires (Fig
1).
 |
|
Fig. 1 Flow chart of the study
procedure.
|
Phase 1: Designing of the Parent-report Developmental
Screening Questionnaires
Phase 1 of the study consisted of four steps. In the
first step, observations regarding the current developmental milestones
were obtained from a convenience sample of parents of 30 children each
in the age group of 9-month to 9-month-14-days and 18-month to
18-month-29-days, recruited from the immunization room of pediatric OPD
(10 each from upper, middle and lower socioeconomic strata) [10]. The
inclusion criteria were that the available parent should have primary
education, is living with the child, and the primary language of
communication is Hindi. The exclusion criteria were children with
history of prematurity, low birth weight, perinatal asphyxia, bilirubin
encephalopathy, meningitis/encephalitis and NICU stay > 4 days, known
dysmorphic syndrome or chromosomal anomaly, chronic systemic illness,
and severe acute malnutrition. Children were screened for enrollment by
a pediatric resident. After obtaining informed consent, parents were
invited to a quiet room. In the presence of a developmental pediatrician
and a pediatric resident, parents were requested to provide a detailed
account of the development milestones currently achieved by their child
(the activities that their child is currently doing), in their own words
in Hindi language. To elicit milestones in all the developmental
domains, some clues pertaining to the domains of development were
provided that were missed by the parents i.e. they were asked
about activities that the child can do with his/her hands, what does he
speak etc. The responses were recorded in Hindi language.
In the second step, a list of all the milestones
enumerated by the parents was prepared in Hindi language along with
their frequency. The different sentences/words used to describe the same
milestone by the parents were also listed below the respective
milestone. A meeting consisting of the investigators (2 developmental
pediatricians, a clinical psychologist and a pediatric resident) and a
language specialist was called and all the enumerated milestones were
discussed in details. In each age group, milestones were chosen (by
consensus decision-making based on simple majority) taking into
consideration the appropriateness and frequency of enumeration by the
parents. The simplest language with reading level of 5 th-grade
or less was chosen. Each milestone was converted into a question by
prefixing Hindi translation of ‘Does your child’ to the milestone i.e.
the milestone ‘Understands being scolded’ was converted to ‘Does your
child understand being scolded?’. Thus initial draft of the screening
questionnaires was designed for each age group. Each item was to be
scored on a Likert scale of 1-3 (1-activity has never been observed,
2-activity is sometimes observed or performed with difficulty,
3-activity is frequently observed and easily performed), with a lower
score indicating a higher risk of developmental delay.
In the third step, each questionnaire was pre-tested
in parents of 15 children. The inclusion and exclusion criteria were
same as that of the first step. Each parent was requested to grade the
understandability and relevance of each question on the scale of 1-3
(for understandability, 1-difficult to understand, 2-some difficulty in
understanding, 3-easy to understand; for relevance, 1- not relevant to
my child, 2-some relevance, 3-highly relevant)
In the fourth step, a meeting consisting of
investigators and language specialist was reconvened. All the items
rated to be difficult to understand or irrelevant were modified,
replaced or discarded and the final screening questionnaires were
designed.
Phase 2: Validation of the Questionnaire
Validation was done using Developmental Assessment
Scale for Indian Infants (DASII), a gold standard instrument [11].
A convenience sample of 200 children were enrolled
(100 each in the age group of 9-month to 9-month-14-days and
18-month to18-month-29-days). In each group, sixty children were
recruited consecutively from immunization room of pediatric outpatient
department (referred to as low risk group) and 40 were recruited
consecutively from the follow-ups of high risk neonatal clinic and new
cases referred to child development clinic (referred to as high risk
group). The inclusion criteria were that one of the available parents
has completed primary education, is able to read Hindi language and had
been living with the child. The exclusion criteria were history of
prematurity, acute severe illness and previous diagnosis of
developmental disorder.
Children were screened for enrollment by a pediatric
resident. After obtaining informed consent, a detailed clinical
evaluation was done. The questionnaire was given to the parents for
self-reporting and scored by a pediatric resident involved in the study.
Developmental quotient (DQ) of the child was assessed using Development
Assessment Scale for Indian Infants (DASII) by a clinical psychologist,
preferably on the same day or within next 1 week. The clinical
psychologist was blinded to the scores of the questionnaire.
DASII consists of a mental and motor scale and
provides a corresponding DQ score. A DQ score
£70 (£2SD)
in either scale is considered as failure (developmental delay). In this
study, another criteria was also used for defining developmental delay;
DQ score £85 (£1SD)
in either scale. This group included children with mild/borderline
developmental delay who might also benefit from early intervention.
Parents of children who failed on DASII were counseled and early
intervention services were offered.
Statistical analysis: The data was
analyzed using SPSS version 16 and STATA version 12. The results of
screening questionnaires were obtained as continuous variables between
20 to 60. The results of DASII was in form of pass or fail. Receiver
operating characteristic (ROC) analysis was done for validation of
questionnaires and defining appropriate cut-off values on the
questionnaires to classify screen positives. Area under curve (AUC) was
used as the measure of validity. Various coordinate points on ROC curve
were studied and optimal cut-off values on the tool was identified,
keeping in consideration that the cut-off value should yield high
sensitivity with reasonable specificity. Psychometric properties of the
tool (sensitivity, specificity and positive and negative predictive
values) at the identified cut-off values were reported.
Results
In the designing phase, in 9-months and 18-month age
group, 28 and 26 milestones, respectively were enumerated by five or
more parents. Twenty milestones were chosen in 9-month age group and 21
in 18-months age group, for designing the initial draft of
questionnaire. On pretesting, 4 and 5 items, were rated as difficult to
understand/irrelevant in the 9- and 18-month questionnaires,
respectively. They were modified, replaced or discarded. The final
questionnaires consisted of 20 items for each age group.
For validation, the questionnaires were given to
parents of 100 children in each age group for self-reporting. It took
around 10 minutes for parents to complete the questionnaire. The
socio-demographic and other characteristics of participants are shown in
Webtable I. Table I shows the results of
DASII evaluation in the study subjects.
TABLE I Result of DASII in the Study Population (N=100)
|
DASII results |
Low risk |
High risk |
Total |
|
group (n=60) |
group (n=40) |
|
|
9-month group |
|
Score ≤70 |
3 (5) |
19 (47.5) |
22 (22) |
|
Score ≤85 |
7 (11.7) |
23 (57.5) |
30 (30) |
|
18-month group |
|
Score ≤70 |
4 (6.6) |
31 (77.5) |
35 (35) |
|
Score ≤85 |
6 (10) |
32 (80) |
38 (38) |
|
Values in n (%), DASII: Developmental assessment scale for
Indian infants. |
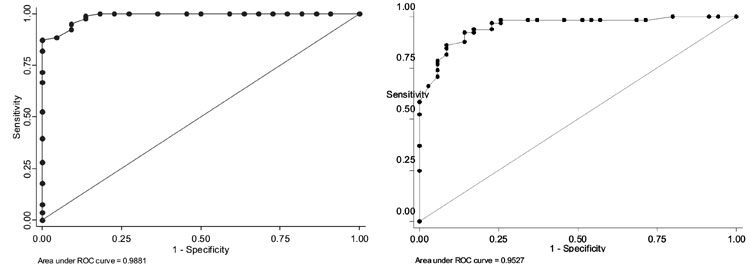
Using DASII score
£70 to define
developmental delay, the 9-month questionnaire had an AUC of 0.988 (95%
CI 0.972-1.004), (Fig. 2). In high-risk and low-risk
group, the AUC was 0.977 (95% CI 0.943-1.012) and 1.000, respectively.
Using DASII score £85
to define developmental delay, the AUC was 0.948 (95% CI 0.898-0.998).
In high risk and low risk group, AUC was 0.909 (95% CI 0.820-0.998) and
0.987 (95% CI 0.959-1.014), respectively.
The 18-month questionnaire had an AUC of 0.953 (95%
CI 0.914 to 0.992), using DASII score
£70 to define
developmental delay (Fig. 2). In high-risk and low- risk
group, the AUC was 0.901 (95% CI 0.749-1.054) and 0.924 (95% CI 0.843 to
1.005), respectively. Using DASII score
£85 to define
developmental delay, the AUC was 0.939 (95% CI 0.889-0.989). In
high-risk and low-risk group, AUC was 0.846 (95% CI 0.652-1.040) and
0.943 (95% CI 0.879-1.007), respectively.
 |
|
Fig. 2 ROC analysis of recruited
9-month (a) and 18-month children (b), using DASII score
£70
to define developmental delay.
|
On 9-month and 18-month questionnaire score
£50 and score
£49, respectively
were suggested as appropriate cut-off for detecting developmental delay
(DQ £70). For
detecting developmental delay along with mild/borderline developmental
delay (DQ £85),
score £52 was
suggested as appropriate cut-off on both the questionnaires. The
psychometric properties of the questionnaires at the suggested cut-offs
are shown in Table II and Table III.
TABLE II Test Characteristics of Screening Questionnaire for Detecting Developmental Delay*
|
Sensitivity |
Specificity |
Positive predictive |
Negative predictive |
|
(%) |
(%) |
value (%) |
value (%) |
|
9-months questionnaire, at cut off score of
≤50 |
|
|
|
|
|
Overall |
100 |
87.2 |
68.8 |
100 |
|
High risk group |
100 |
81 |
82.6 |
100 |
|
Low risk group |
100 |
89.5 |
33.3 |
100 |
|
18-months questionnaire, at cut off score of
≤49 |
|
|
|
|
|
Overall |
91.4 |
88.7 |
80.0 |
95.4 |
|
High risk group |
93.5 |
77.8 |
93.5 |
77.8 |
|
Low risk group |
75 |
90.3 |
33.33 |
98.2 |
|
*Developmental delay defined as DAS II Score <70. |
Discussion
These Hindi language parent self-report
questionnaires, labelled New Delhi – Development Screening Questionnaire
(ND-DSQ), are free to use, besides being highly valid. Conventionally, a
new screening tool is designed by selecting items from existing
screening or diagnostic tools; however, in this study the items were
chosen from the parental observations of the representative population
making it an ideal self-report tool. This tool tapped some new
milestones, which are probably pertinent only to the Indian population.
With twenty items directed towards a single age-level, it is a
comprehensive tool. It can be reported by parents while waiting for
immunizations. They can also be administered via email or through
a computer-based program. For parents who cannot read, the
questionnaires can be administered by a health worker or family member.
Overall, these questionnaires appear to have a promising role in
developmental screening in our country.
The major limitations of this study were the small
sample size for designing and validation of questionnaires. Moreover
these questionnaires were applicable to narrow age ranges. In our
setting, as many children present late for immunization, the screening
questionnaires should be applicable to a wide age-ranges and ideally
should exist for all possible age-ranges.
The conventional Indian screening tools like
Trivandrum Development Screening Chart (TDST), and Baroda Development
Screening Test (BDCT) have only moderate sensitivities and
specificities, and require a trained health-worker for administration
[12]. INCLEN Neurodevelopmental Screening Test is a new addition to
these tools; however, it’s a broad screener tool for multiple type of
disabilities and is applicable for 2-9 old children only [13]. Recently,
a 27-item parent report tool was developed at Lucknow for infants aged
6-24 months. The sensitivity and specificity were 95.9% and 73.1%,
respectively [14].
Ages and Stages Questionnaire (ASQ) is the most
widely studied parent report tool in the West. It consists of 19
questionnaires (30-items each) spanning the age of 4-60 months, with an
overall sensitivity of 75% and specificity of 86% [15]. ASQ has been
studied in high-risk populations like follow-ups of hypoxic ischemic
encephalopathy and prematurity, with good results [16,17]. It has been
also found useful for detecting mild/borderline developmental delays
[16,18,19]. Parent’s Evaluation of Development Status (PEDS) is another
parent report tool available in English language [20]. It is applicable
from birth to eight years of age. A study on PEDS from Indonesia on 170
infants aged 3-12 months, showed sensitivity of 83.9%, and specificity
of 81.3% [21]. In an Indian study, PEDS was used to screen children aged
24-60 months, the sensitivity was 75% and specificity was 74% [22].
As compared to these tools, the present tool has
better psychometric properties.
To conclude, these Hindi parent self-report
questionnaires have a promising role in developmental screening in our
country. Further studies are required to assess the properties of this
tool when used for wider age ranges, including community-based studies.
Further, similar questionnaires need to be developed for all possible
age ranges, to implement a comprehensive developmental screening
program. These questionnaires may be a useful adjunct to the recently
launched Rashtriya Bal Swasthya Karyakram (RBSK), a child health
screening and early intervention program under National heath mission
[23].
Contributors: RJ: conceptualized the study. All
the authors were involved in designing the study. AA: collected the data
for 9-months age group and RA collected the data for 18-months age
group; RJ, AA, RA, SM and MM: were involved in designing of screening
questionnaires; SM: did the gold standard developmental assessment; RJ,
AA and RA: drafted the manuscript; RJ, MM and MJ: revised the manuscript
for important intellectual contents. The final manuscript was approved
by all authors. All authors will be accountable for all aspects of the
work.
Funding: None; Competing interest: None
stated.
|
What is Already Known?
•
Parental reports developmental
screening tools are reliable and valid.
What This Study Adds?
•
New parent self-report developmental screening tool has been
designed in Hindi language and validated for use in 9-month and
18-month-old children.
|
References
1. Shevell M, Ashwal S, Donley D, Flint J, Gingold M,
Hirtz D, et al. Practice Parameter: Evaluation of the Child with
Global Developmental Delay: Report of the Quality Standards Subcommittee
of the American Academy of Neurology and The Practice Committee of the
Child Neurology Society. Neurology. 2003;60:367-80.
2. Blauw-Hospers CH, Hadders-Algra M. A systematic
review of the effects of early intervention on motor development. Dev
Med Child Neurol. 2005;47:421-32.
3. Spittle A, Orton J, Anderson P, Boyd R, Doyle LW.
Early developmental intervention programmes post-hospital discharge to
prevent motor and cognitive impairments in preterm infants. Cochrane
Database Syst Rev. 2012;12:CD005495
4. Shonkoff JP, Hauser-Cram P. Early
intervention for disabled infants and their families: a quantitative
analysis. Pediatrics. 1987;80:650-8
5. Sharkey MA, Palitz ME, Reece LF, Rutherford BL,
Akers JP, Alvin BL, et al. The effect of early referral and
intervention on the developmentally disabled infant: evaluation at 18
months of age. J Am Board Fam Pract. 1990;3:163-70.
6. Bailey DB Jr, Hebbeler K, Scarborough A, Spiker D,
Mallik S. First experiences with early intervention: a national
perspective. Pediatrics. 2004;113:887-96.
7. Earls MF, Hay SS. Setting the stage for success:
implementation of developmental and behavioral screening and
surveillance in primary care practice—the North Carolina Assuring Better
Child Health and Development (ABCD) Project. Pediatrics.
2006;118:e183-8.
8. Sices L, Feudtner C, McLaughlin J, Drotar D,
Williams M. How do primary care physicians identify young children with
developmental delays? A national survey. J Dev Behav Pediatr.
2003;24:409-17.
9. Rydz D, Srour M, Oskoui M, Marget N, Shiller M,
Birnbaum R, et al. Screening for developmental delay in the
setting of a community pediatric clinic: a prospective assessment of
parent-report questionnaires. Pediatrics. 2006;118:e1178-86.
10. Bairwa M, Rajput M, Sachdeva S. Modified
Kuppuswamy’s Socioeconomic Scale: Social researcher should include
updated income criteria, 2012. Indian J Community Med. 2013;38:185-6.
11. Phatak P. Manual for using Development Assessment
Scales for Indian Infants (DASII): Based on revised Baroda norms. Pune:
Anand Agencies; 1997.
12. Mukherjee SB, Aneja S, Krishnamurthy V,
Srinivasan R. Incorporating developmental screening and surveillance of
young children in office practice. Indian Pediatr. 2014;51:627-35.
13. Silberberg D, Arora N, Bhutani V, Durkin M,
Gulati S. Neuro-developmental disorders in India – An INCLEN study.
Neurology.02013;80:IN6-2.001.
14. Bhave A, Bhargava R, Kumar R. Development and
validation of a new Lucknow Development Screen for Indian children aged
6 months to 2 years. J Child Neurol. 2010;25:57-60.
15. Squires J, Bricker D, Potter L. Revision of a
parent-completed development screening tool: Ages and Stages
Questionnaires. J Pediatr Psychol. 1997;22:313-28.
16. Lindsay NM, Healy GN, Colditz PB, Lingwood BE.
Use of the Ages and Stages Questionnaire to predict outcome after
hypoxic-ischaemic encephalopathy in the neonate. J Paediatr Child
Health. 2008;44:590-5.
17. Skellern CY, Rogers Y, O’Callaghan MJ. A
parent-completed developmental questionnaire: follow up of ex- premature
infants. J Paediatr Child Health. 2001;37:125-9.
18. Juneja M, Mohanty M, Jain R, Ramji S. Ages and
Stages Questionnaire as a screening tool for developmental delay in
Indian children. Indian Pediatr. 2012;49:457-61.
19. Gollenberg AL, Lynch CD, Jackson LW, McGuinness
BM, Msall ME. Concurrent validity of the parent-completed Ages and
Stages Questionnaires, 2nd Ed. with the Bayley Scales of Infant
Development II in a low-risk sample. Child Care Health Dev.
2010;36:485-90.
20. Glascoe FP. Parent’s Evaluation of Developmental
Status (PEDS). Nashville, TN: Ellsworth & Vandermeer Press; 1997.
21. Gustawan WI, Machfudz S. Validity of parents’
evaluation of developmental status (PEDS) in detecting developmental
disorders in 3–12 month old infants. Paediatr Indones. 2010;50:6-10.
22. Malhi P, Singhi P. Role of parents evaluation of
developmental status in detecting developmental delay in young children.
Indian Pediatr. 2002;39:271-5.
23. Rashtriya Bal Swasthya Karyakram, National
Health Mission. Ministry of health and family welfare, Government of
India. Available from: http://nrhm.gov.in/images/pdf/programmes/RBSK/Fo_more_
information.pdf. Accessed December 20, 2016.
|
|
|
 |
|

