|
|
|
Indian Pediatr 2016;53: 631-633 |
 |
Rotavirus Infection in
Children with Acute Gastroenteritis in Aurangabad, Central
Maharashtra
|
|
Ganesh Maher, *Gauri Pradhan,
#Sushmitha Shetty, *Sujata
Ranshing,
Ajit Damle
and *Shobha
Chitambar
From Government Medical College, Aurangabad; *Enteric
Viruses Group, National Institute of Virology, Pune; and #Enterovirus
Research Center, Mumbai; India.
Corresponding to: Dr Shobha Chitambar, National
Institute of Virology, 20-A, Dr Ambedkar Road, Pune-411001, India.
Email: [email protected]
Received: September 03, 2015;
Initial review: December 19, 2015;
Accepted: May 05, 2016.
|
Objective: To determine the prevalence of
rotavirus diarrhea and its genotypes in children from Aurangabad, India.
Methods: Stool samples collected during 2012-2013
from 168 children, aged £3
years, were tested by ELISA to detect rotavirus. Rotavirus strains were
genotyped by multiplex reverse-transcription polymerase chain reaction.
Results: Stool samples from 20 (11.9%) children
tested positive for rotavirus. Rotavirus positivity was higher among the
children aged 0-12 months than those in 13-24 and 25-36 months. Severity
of disease was moderate in both rotavirus-infected and uninfected
children. Genotype G1P[8] combination was detected predominantly in
circulation.
Conclusion: Rotavirus diarrhea was caused mainly
by G1P[8] strains during 2012-2013 in Aurangabad, Central Maharashtra,
India.
Keywords: Acute diarrhea, Epidemiology, Etiology.
|
|
R
otavirus is a major cause of severe diarrhea
among children worldwide [1]. Studies conducted in India have
established rotavirus strain diversity in the study regions [2].
Rotavirus vaccine has now been introduced in the national immunization
program by Government of India. While impact of rotavirus vaccination on
rotavirus disease is yet to be gauged, ongoing rotavirus surveillance
continues to be crucial in pre- and post-vaccination period in India
wherein diversity in climatic conditions and geographic regions is well
known. The present study was performed to estimate the proportion of
diarrhea due to rotavirus, and to identify the rotavirus genotypes among
diarrheal children £3
years from Aurangabad, Central Maharashtra, India.
Methods
The study was conducted from January, 2012 to
October, 2013 in children £3
years, admitted or visiting outpatient department (OPD) for acute
gastroenteritis in a tertiary care Government Medical College Hospital,
Aurangabad, India. Institutional Ethics Committee’s approval, and
informed consent from parents were obtained. A case of acute
gastroenteritis enrolled in the study was defined as the passage of
³3 loose or
watery stools a day with or without associated symptoms such as
vomiting, fever and abdominal pain. Clinical information was obtained
from each patient for assessment of severity of diarrhea [3]. Stool
samples collected from all children (n=168) who fulfilled the
inclusion criteria were transported on ice to National Institute of
Virology (NIV), Pune and processed to detect rotavirus antigen using
commercially available ELISA kit (Generic Assays, Dahlewitz, Germany).
Viral RNA extracted from all ELISA-positive stool
specimens using Trizol (Invitrogen, Carlsbad, CA) was genotyped for VP7
and VP4 genes by multiplex reverse-transcription polymerase chain
reaction (RT- PCR) as described earlier [4,5]. First round PCR products
that remained non-amplified in the second round PCR were sequenced using
ABI-PRISM Big Dye Terminator Cycle Sequencing Kit (Applied Biosystems,
Foster city, CA) and a ABI-PRISM 310 Genetic analyzer (Applied
Biosystems).
Data from case report forms was entered into Excel
2007 (Microsoft, Redmond, WA, USA) for analysis. Tests of proportion
were applied and a P value <0.05 was considered to be
statistically significant.
Results
One hundred sixty-eight children who participated in
the study during 2012-2013, comprised of 125 hospitalized and 43 OPD
patients, with male to female ratio at 1.37:1. Twenty (11.9%) children
showed positivity to rotavirus antigen in the stool samples. Males
showed higher (14/97, 14.4%) positivity than females (6/71, 8.4%) (P=0.34).
TABLE I Characteristics of Rotavirus-infected and Uninfected Children with Acute Gastroenteritis
Variables
|
Rotavirus infected children
(n=20) No. (%) |
Rotavirus uninfected children
(n=148) No. (%) |
P Value
|
|
Male Gender |
14 (70) |
83 (56) |
0.34 |
|
Age (mo), Mean (SD) |
13.1 (8.7) |
16.7 (11.4) |
0.07 |
|
Vomiting |
9 (45) |
55 (37) |
0.66 |
|
Fever |
8 (40) |
28 (18.9) |
0.06 |
|
Diarrhea duration (d), Mean (SD) |
4.8 (1.7) |
4.7 (1.8) |
0.83 |
|
Diarrhea episodes, Mean (SD) |
8.9 (4.6) |
8.2 (2.7) |
0.52 |
|
Vesikari score, Mean (SD) |
9.6 (2.5) |
9.2 (3.2) |
0.54 |
|
Disease severity by Vesikari score |
|
Mild |
0 (0) |
11(7.4) |
0.43 |
|
Moderate |
14 (70) |
89 (60.1) |
0.54 |
|
Severe |
5 (25) |
42 (28.4) |
0.98 |
|
Very Severe |
1 (5) |
6 (4) |
0.69 |
|
Dehydration |
|
None |
11 (55) |
86 (58.1) |
0.98 |
|
Some |
9 (45) |
61 (41.2) |
0.93 |
|
Severe |
0 (0) |
1 (0.67) |
0.23 |
The mean (SD) age of children was 16.6 (11.6) months;
that of rotavirus infected and uninfected children was 13.1 (8.7) and
16.7 (11.4) months, respectively (Table I). Among
rotavirus positive children, age group of 0-12 months showed higher
score (13/20, 65%) as compared to those of 13-24 (5/20, 25%) and 25-36
months (2/20, 10%) (P=0.02 and 0.001, respectively). Rotavirus
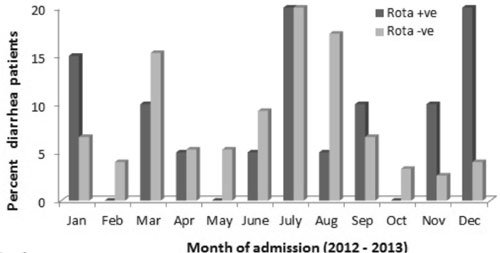
infections were detected in almost all months of the year (Fig.
1).
 |
|
Fig. 1 Month-wise distribution of
rotavirus positivity during 2012-13.
|
Presence of fever, vomiting, duration and number of
episodes of diarrhea and the mean (SD) Vesikari scores did not differ in
rotavirus positive and negative children (Table I), and a
moderate severity of disease were found in both categories.
Infections with G1P[8] (12/20,60%) were most
prevalent as compared to other rotavirus strains (G2P[4] (10%),
mixed:G1G10P[8] (10%)). Two strains with genotype VP4 P[8] remained non-typeable
for VP7 gene, while two strains were non-typeable for both VP7 and VP4
genes.
Discussion
The present study reports moderate level of rotavirus
diarrhea in Aurangabad during 2012-2013. During 1982-2004, 6% to 45%
(median 20.8) rotavirus positivity rates were reported among diarrheal
children from various parts of the country [6]. Another study carried
out by Indian Rotavirus Strain Surveillance Network (IRSN) during
2005-2009 in seven different cities has documented 40% rotavirus
positivity in children hospitalized for diarrhea [2]. Compared to these
data, lower rate noted in our study may be attributed to the moderate
severity of diarrheal disease experienced by most of the enrolled
inpatients and inclusion of OPD patients in our study. The prevalence of
rotavirus infection has been reported to be low in outpatients as
compared to the hospitalized patients [7].
Rotavirus positivity was noted in the months of
March, July and September along with December-January known for highest
proportion of rotavirus infections [8]. This may be due to the semi-arid
climate described under the Koppen climate classification system for
Aurangabad, central Maharashtra [9]. The high contribution of G1P[8]
strain is consistent with the data reported from other regions of India
recently [2,10].
Our study had a limitation of a small sample size.
However, it highlights rotavirus epidemiology and strain diversity in
Aurangabad, central Maharashtra. Continued surveillance of rotavirus
disease and strains in this region of India would be useful to ascertain
rotavirus prevalence and changing pattern, if any, in the circulating
strains.
Acknowledgements: Dr DT Mourya, Director and Dr
AC Mishra, Ex-Director, NIV, Pune; and Head and the staff of Department
of Pediatrics, Government Medical College Hospital, Aurangabad.
Contributors: GM, SS and SR: conducted and
interpreted the laboratory tests; GM and GP: collected, analyzed the
data and drafted the manuscript; SC: conceived and designed the study;
AD and SC: revised the manuscript for important intellectual content.
The final manuscript was approved by all authors.
Funding: Indian Council of Medical Research, New
Delhi. Competing interest: None stated.
|
What This Study Adds?
• Moderate level (11.9%) of rotavirus disease
with significant (60%) contribution of G1P[8] strains was seen
in children (age £3
years) suffering from acute diarrhea in Aurangabad, Central
Maharashtra.
|
References
11. Tate JE, Burton AH, Boschi-Pinto C, Steele AD,
Duque J, Parashar UD. 2008 estimate of worldwide rotavirus-associated
mortality in children younger than 5 years before the introduction of
universal rotavirus vaccination programs: A systematic review and
meta-analysis. Lancet Infect Dis. 2012;12:136-41.
2. Kang G, Desai R, Arora R, Chitamabar S, Naik TN,
Krishnan T, et al. Diversity of circulating rotavirus strains in
children hospitalized with diarrhea in India, 2005-2009. Vaccine. 2013;
27:2879-83.
3. Ruuska T, Vesikari T. A prospective study of acute
diarrhea in Finnish children from birth to 2½ years of age. Acta
Paediatr Scand. 1991;80:500-7.
4. Tatte VS, Gentsch JR, Chitambar SD.
Characterization of group A rotavirus infections in adolescents and
adults from Pune, India: 1993-1996 and 2004-2007. J Med Virol.
2010;3:519-27.
5. Gentsch JR, Glass RI, Woods P, Gouvea V, Gorziglia
M, Flores J, et al. Identification of group A rotavirus gene 4
types by polymerase chain reaction. J. Clin. Microbiol. 1992;30:1365-73.
6. Ramani S, Kang G. Burden of disease and molecular
epidemiology of group A rotavirus infections in India. Indian J Med Res.
2007;125:619-32./p>
77. Kelkar SD, Purohit SG, Boralkar AN, Verma SP.
Prevalence of rotavirus diarrhea among outpatients and hospitalized
patients: a comparison. Southeast Asian J Trop Med Public Health.
2001;32:494-9.
8. Kang G, Arora R, Chitambar SD, Deshpande J, Gupte
MD, Kulkarni M, et al. Multicenter, hospital-based surveillance
of rotavirus disease and strains among Indian children aged <5 years. J
Infect Dis. 2009;200:S147-53.
9. Climate of Aurangabad. India Meteorological
Department. Available from: http://www.imd.gov.in/doc/climateimp. pdf.
Accessed May 31, 2014.
10. Chitambar SD, Ranshing SS, Pradhan GN, Kalrao
VR, Dhongde RK, Bavdekar AR. Changing trends in circulating rotavirus
strains in Pune, western India in 2009–2012: Emergence of a rare G9P [4]
rotavirus strain. Vaccine. 2014;32:A29-32.
|
|
|
 |
|

