|
|
|
Indian Pediatr 2015;52:
579-582 |
 |
Postnatal Lactational Counseling and Neonatal
Weight Pattern
|
|
Noella MD Pereira, Rahul J Verma and *Nandkishor S
Kabra
From the Departments of Neonatology, Holy Spirit
Hospital; and *Surya Children’s Hospital, Mumbai, India.
Correspondence to: Dr Noella Maria D Pereira, ‘Torrefiel’,
127, Carter Road, Opp. Joggers Park, Bandra West, Mumbai 400 050, India.
Email:
[email protected]
Received: February 25, 2013;
Initial review; March 01, 2013;
Accepted: April 28. 2015.
|
Objective: To compare the impact of postnatal lactational counseling
on the weight gain and frequency of mixed feeding in full term neonates.
Design: Observational study.
Setting: Mother-infant pairs were
observed in the maternity section of a multispecialty general hospital
in Mumbai during two time periods.
Participants: 260 mothers who
delivered a full term, healthy, appropriate for gestational age neonate
with birth weight >2.2 kg.
Methods: Between 18 November,
2007 and 4 March, 2008, 126 mothers received unstructured verbal
encouragement to maintain breastfeeding from the maternity staff. From 1
June, 2008 to 16 December, 2008, 134 mothers were counseled about
breastfeeding by the pediatric residents and nurses with the help of
charts, literature and verbal advice. They were supervised and helped
during the first feed and subsequently until discharge.
Main outcome measure: Weight gain
(g/kg/day) of neonate at 28 days of life.
Results: The mean (SD) weight
gain was significantly higher in the counseled group in comparison to
historical control group [9.2 (4.5) g/kg/d vs. 7.9 (5.1) g/kg/d;
P=0.03]. Mixed feeding occurred less frequently in [RR 0.36, 95%
CI 0.13, 0.98; P=0.046] the counseled group (5/134) as compared
to control group (13/126).
Conclusions: Postnatal
lactational counseling leads to higher weight gain, and lesser chances
of mixed feeding in the neonatal period.
Keywords: Breastfeeding, Neonate, Nutrition.
|
|
Early successful breastfeeding is known to be
important in securing effective, long term lactation [1-5]. Early
initiation of breastfeeding and exclusive breastfeeding [6] for six
months or more has many advantages but is only practiced in less than
half of the population in India [7]. Globally over one million newborn
infants could be saved each year by initiating breastfeeding within the
first hour of life [8].
There is some evidence that the implementation of the
‘ten steps to successful breast feeding’ (Baby Friendly Hospital
Initiative) [9] shall lead to an increase in exclusive breastfeeding.
There are several studies [10-15] documenting the benefit of lactational
counseling to secure effective long term lactation. However, there is
paucity of literature documenting the effect of postnatal maternal
lactational counseling on the weight gain and a reduction in mixed
feeding rates amongst term infants.
We carried out this study to assess whether postnatal
lactational counseling of the mother has any positive impact on the
neonatal weight gain or reduction in the frequency of mixed feeding.
Methods
The study was conducted in the maternity section of
the Department of Obstetrics and Gynecology of a multispecialty general
hospital where the annual rate of deliveries is about 800 per year. The
study population consisted of mothers who had delivered a full term ( ³37
to £42 weeks)
healthy singleton appropriate for gestational age (AGA) neonates, with a
birth weight of >2.2 kg. Mother–infant pairs were excluded if the mother
or infant was admitted to an intensive care unit, if the infant was born
with congenital or chromosomal malformations, or those who were not
likely to follow-up due to distance from home to the hospital or likely
migration. The research ethics board of the institution approved the
protocol. Informed consent was taken from the mothers of the enrolled
infants.
During the period between 19th November 2007 and 4th
March 2008, mothers of infants received the usual verbal encouragement
to maintain breastfeeding from the maternity staff. From 5th March 2008
to 31st May 2008, pediatric residents and nursing staff in the maternity
unit were formally trained in postnatal lactational counseling in a
structured format with the use of charts, literature and verbal advice.
They were trained by Infant and Young Child Feeding (IYCF)-certified
lactational consultants at our hospital. They received several lectures,
talks and one-to-one discussions on benefits of breastfeeding,
positioning, attachment, and the management of problems faced while
breastfeeding. Mothers of infants born between 1st June 2008 to 16th
October 2008 were individually counseled postnatally from day 1 of life
about breastfeeding by the pediatric residents and nurses with the help
of charts, literature and verbal encouragement. These mothers were
supervised and helped during the first feed and subsequently till
discharge. They were empowered with the knowledge of breastfeeding – its
benefits, demonstration of correct positioning, attachment – on and
duration of each feed. Approximately 4-5 counseling sessions were
conducted, each lasting for 45-60 minutes. They were encouraged to
exclusively breastfeed their infants for 6 months or more. They were
counseled at their bedside in the comfort of their room with adequate
privacy for the mother.
The weights of the infants in both groups were
recorded on day 1 and 3 while in the hospital, and on day 7, 14 and 28
during the follow-up visits. Mothers in the intervention group were
counseled and encouraged to continue breastfeeding. The mothers in both
the groups were asked about the details of feeding at the end of 28 days
from birth. Infants were weighed naked on an electronic weighing scale
(Eagle Model No. EUT30) with minimum reading of one gram.
Baseline socio-demographic, maternal and birth
details were recorded. The primary outcome was the assessment of weight
gain (g/kg/day) at day 28 of life. The secondary outcomes were: weight
on day 3, day 7 and day 14; the frequency of mixed feeding (defined by
use of animal/formula milk in addition to breast milk).
The baseline characteristics for both mothers and
infants were analyzed by the unpaired ‘t’ test for continuous variables.
This test was also used to analyze the weight change on day 3, 7, 14 and
28. Adjusted analysis using linear regression was performed for primary
outcome measure to assess the impact of the baseline maternal
characteristics that were not equally distributed in the two comparison
groups. Chi–square test was used for the categorical outcome of mixed
feeding and relative risk was used as a measure of association. A P
value of <0.05 was considered statistically significant. IBM SPSS
version 21 was used for statistical analysis.
Results
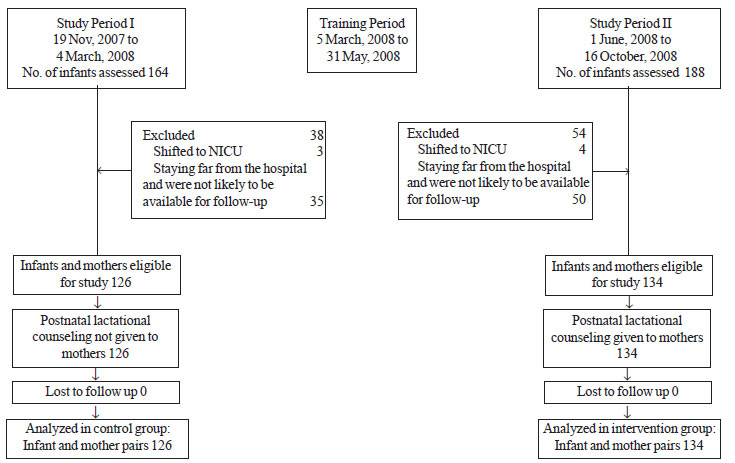
The flow of the participants in study is shown in
Fig. 1. Between 19 November, 2007 and 4 March, 2008, the
control group comprising 126 mothers of 126 infants did not receive
structured postnatal lactational counseling. Between 1 June, 2008 and 16
October, 2008, 134 mothers of 134 infants received postnatal lactational
counseling. The baseline maternal and infant characteristics of
both groups are presented in Table I.
 |
|
Fig. 1 Flow chart of study subjects.
|
TABLE I Characteristics of the Study Population
|
Control |
Intervention |
P |
|
group |
group |
value |
|
(n=126) |
(n=134) |
|
|
Mother’s characteristics |
|
*Age, y |
27.4 (4.5) |
27.4 (4.6) |
0.97 |
|
Prior breastfeeding experience, No. (%) |
50 (40) |
49 (37) |
0.61 |
|
Socioeconomic class |
|
|
<0.01 |
|
I |
34 (27) |
43 (32) |
|
|
II |
52 (41) |
79 (59) |
|
|
III |
38 (30) |
9 (7) |
|
|
IV |
2 (2) |
3 (2) |
|
|
Education |
|
|
0.005 |
|
Below SSC |
15 (12) |
28 (21) |
|
|
SSC |
27 (21) |
17 (13) |
|
|
HSC |
7 (6) |
20 (15) |
|
|
Graduate |
60 (48) |
46 (34) |
|
|
Post Graduate |
17 (13) |
23 (17) |
|
|
Mode of delivery |
|
|
0.68 |
|
Vaginal |
64 (51) |
75 (56) |
|
|
LSCS |
46 (36) |
45 (34) |
|
|
Vacuum |
16 (13) |
14 (10) |
|
|
Analgesia received |
46 (37) |
45 (34) |
0.70 |
|
Infant characteristics |
|
*Birthweight, g |
2969 (382) |
2959 (347) |
0.82 |
|
*Gestational age, wk |
38.7 (1.1) |
38.9 (1.1) |
0.09 |
|
*Values in mean (SD). |
The weight gain pattern at day 28 in the two groups
is shown in Table II. The weight gain at day 28 was
significantly higher in the group who received lactation counseling.
Adjusting for baseline differences in maternal weight, socioeconomic and
educational status did not change these results. The weight loss pattern
on day 3 and 7 and weight gain patterns on day 14 were also favorable in
group that received lactation counseling (Table II).
TABLE II Weight Pattern in Neonates in Two Group
|
Weight gain |
Control group |
Intervention group |
Mean difference |
P |
|
(g/kg/d) |
(Lactational counseling |
(Lactational counseling |
(95% CI) |
value |
|
not given) (n= 126) |
given) (n=134) |
|
|
|
Day 28, Mean (SD) |
7.9 (5.1) |
9.2 (4.5) |
1.30 (0.12, 2.48) |
0.030 |
|
*Day 3, Mean (SD) |
26.9 (10.2) |
23.2 (10.8) |
–3.67 (–6.23, –1.10) |
0.005 |
|
*Day 7, Mean (SD) |
4.9 (7.5) |
2.7 (7.4) |
–2.17 (–3.99, –0.34) |
0.020 |
|
Day 14, Mean (SD) |
3.4 (5.4) |
5.1 (5.3) |
1.73 (0.42,3.04) |
0.010 |
|
* weight loss. |
Mixed feeding occurred less frequently (RR 0.36, 95%
CI 0.13, 0.98; P=0.046) in the intervention group (5/134; 3.7%)
as compared to control group (13/126; 10.3%).
Discussion
Our study demonstrated the beneficial impact of
postnatal lactational counseling on the weight gain at day 28 of life.
It also demonstrated that mothers who received postnatal lactational
counseling of were less likely to practice mixed feeding.
The limitations of our study were: an observational
design with historical control, and infants were not followed up beyond
28 days of life. Moreover, there was a difference in the level of
education and socio-economic status in the two groups that might have
influenced the outcome to some extent. However, adjusted analysis for
maternal weight, socio-economic class and education status did not
change direction of the results.
Our study supplements the findings of other studies
by showing that specific instructions directed at early initiation of
breastfeeding are effective not just in changing maternal behavior but
also resulting in better infant weight gain. It has been suggested that
early initiation of suckling is correlated with a prolonged duration of
breastfeeding [16]. Our results are comparable to earlier studies
[10-12] that demonstrated peer counseling promotes exclusive
breastfeeding and can effectively increase the initiation and duration
of exclusive breastfeeding. Randomized controlled trials [13,14]
conducted in Haryana, India demonstrated that community-based
intervention of promotion of exclusive breastfeeding until age 6 months
through existing primary health-care services is feasible, reduces the
risk of diarrhea, and does not lead to growth faltering. Our study
complements the above studies by demonstrating the beneficial impact of
postnatal lactational counseling on the weight-gain during neonatal
period and on decreasing the proportion of mixed feeding. Thakur, et
al. [15] demonstrated that nutrition education given to mothers on
breastfeeding helped increase the weight and length in low birth weight
babies. Our study replicated these results in term infants.
We conclude that postnatal lactational counseling
improves weight-gain in term infants and decreases the rate of
mixed-feeding.
Acknowledgements: Dr. Claudette Vora, Head of
Department of Pediatrics, late Dr. Mrs. Meenakshi M. Shah (former Head
of Department), Dr M B Shah, Medical Director, Sister Lissy, Executive
Director and the Pediatric nursing staff, Holy Spirit Hospital, Mumbai.
Contributors: NMDP: data collection and
manuscript writing; RJV: conceived and designed the study and revised
the manuscript for important intellectual content; NSK: provided inputs
regarding the design, analyzed the data and helped in manuscript
writing. The final manuscript was approved by all the authors.
Funding: None; Competing interests: None
stated.
|
What Is Already Known?
• Early successful breastfeeding is important
in securing effective, long term lactation.
What This Study Adds?
• Postnatal lactational training helps in
better weight gain in neonatal period and reduces the frequency
of mixed feeding.
|
References
1. National Guidelines on Infant and Young Child
Feeding. Ministry of Women and Child Development (Food and Nutrition
Board). Second edition 2006; p.13. Available from:
http://wcd.nic.in/publication/infantandyoung childfeed.pdf. Accessed
October 25, 2014.
2. Physiologic Impact of Breastfeeding. In:
Lawrence RA, Lawrence RM. Breastfeeding: A Guide for Medical
Professionals. 5th ed. Missouri: Mosby, Inc.; 1999. p.197-216
3. How Breastfeeding Should Begin. In: King
F.S. Helping mother’s to Breastfeed. Revised Edition. Indian Adaptation
by RK Anand, Mumbai: Association for Consumers Action on Safety and
Health (ACASH); 1992.
4. Recommendations of the Special Committee of Indian
Academy of Pediatrics on Breastfeeding. Indian Pediatr. 1988;25:873-4.
5. American Academy of Pediatrics Work Group on
Breastfeeding. Breastfeeding and the Use of Human Milk. Pediatrics.
1997;100:1035-9.
6. Infant and Young Child Feeding Chapter, Indian
Academy of Pediatrics. Infant and Young Child Feeding Guidelines: 2010.
Indian Pediatr. 2010;47:995-1004.
7. The World Breastfeeding Trends initiative (WBTi).
Are our infants falling through the Gap? The State of Policies and
Programme Implementation of the Global strategy for Infant and Young
Child Feeding in 51 Countries. BPNI/ IBFAN Asia. Dec 2012. Available
from:
http://www.worldbreastfeedingtrends.org/report/WBTi-India-2012.pdf .
Accessed October 25, 2014.
8. Lauer JA, Betran AP, Barros AJ, De Onis M. Deaths
and years of life lost due to suboptimal breast feeding among children
in the developing world: A global ecological risk assessment. Public
Health Nutr. 2006;9:673-85.
9. Protecting, Promoting and Supporting
Breastfeeding: The Special Role of Maternity services. A Joint
WHO/UNICEF Statement. Geneva. WHO; 1989. Available from:
http://apps.who.int/iris/bitstream/10665/39679/1/9241561300.pdf.
Accessed October 25, 2014.
10. Marrow A, Guerrero M, Shults J, Calva J, Lutter
C, Bravo J, et al. Efficacy of home-based peer counseling to
promote exclusive breastfeeding: A randomized controlled trial. Lancet.
1999; 353:1226-31.
11. Haider R, Ashworth A, Kabir I, Hutty S. Effect of
community-based peer counselors on exclusive breastfeeding practices in
Dhaka, Bangladesh: A randomized controlled trial. Lancet. 2000;
356:1643-47.
12. Valdes V, Perez A, Labbok M, Pugin E, Zambrano I,
Catalan S. The impact of a hospital and clinic-based breastfeeding
promotion programme in a middle class urban environment. J Trop Pediatr.
1993;39:142-51.
13. Morrow A. Case studies of community based
Breastfeeding promotion and support. In: Community Based
Strategies for Breastfeeding Promotion and Support in Developing
Countries. Geneva. WHO. 2003. p.17-19. Available from:
http://apps.who.int/iris/bitstream/10665/42859/1/9241591218.pdf
Accessed October 25, 2014.
14. Bhandari N, Bahl R, Mazumdar S, Martines J, Black
RE, Bhan MK, and Infant Feeding Study Group. Effect of community based
promotion of Exclusive breastfeeding on diarrhoeal illness and growth: A
cluster randomized controlled trial. Lancet. 2003;361:1418-23.
15. Thakur SK, Roy SK, Paul K, Khatun M, Khatum W,
Sarker D. Effect of nutrition education on exclusive breastfeeding for
nutritional outcome of low birth weight babies. Eur J Clin Nutr.
2012;66;376-81.
16. Salariya EM, Easton PM, Cater JI. Duration of
breastfeeding after early initiation and frequent feeding. Lancet.
1978;2:1141-3.
|
|
|
 |
|

