|
|
|
Indian Pediatr 2014;51:
555-560 |
 |
Body Fat Indices for
Identifying Risk of Hypertension in Indian Children
|
|
NA Kajale, AV Khadilkar, SA Chiplonkar and VV Khadilkar
From Hirabai Cowasji Jehangir Medical Research Institute, Jehangir
Hospital, Pune, Maharashtra, India.
Correspondence to: Dr Anuradha Khadilkar, (Pediatrics), Hirabai
Cowasji Jehangir Medical Research Institute, Jehangir Hospital, 32
Sassoon Road, Pune 411 001, India.
Email:
[email protected]
Received September 02, 2013;
Initial review: December 06, 2013;
Accepted: May 08, 2014.
|
Background: High adiposity is
major risk factor for hypertension. Various anthropometric indices are
used to assess excess fatness.
Objectives: (1) To examine
relationship of body mass index (BMI), waist circumference (WC), waist
to height ratio (WHtR), triceps skin fold thickness (TSFT) and wrist
measurements with blood pressure in children and adolescents 2) to
suggest age- and gender-specific cutoffs for these indices in Indian
children.
Methods: Cross-sectional
school-based study on a random sample of 6380 children (6-18 yr old,
3501 boys) from five major cities in India. Height, weight, waist and
wrist circumference, TSFT, and blood pressure were recorded. Children
with systolic blood pressure (BP) and/or Diastolic BP >95th percentile
were classified as hypertensive.
Results: Prevalence of overweight
and obesity was 23.5% and 9.7%, respectively. Hypertension was observed
in 5.6%. Multiple logistic regression (adjustments: age, gender)
indicated double risk of hypertension for overweight and 7 times higher
odds for obese than normal-weight children. Children with TSFT >95th
centile for US children showed three times risk and with TSFT from 85th
to 95th double risk of hypertension. Higher WC and WHtR exhibited 1.5
times risk and larger Wrist 1.3 times higher risk of hypertension (P<0.001).
Receiver operating curve (ROC) analysis provided age-gender specific cut
offs for the five indices to detect the risk of high BP. Area under ROC
curves (AUC) for five indices were similar and greater in older age
groups indicating equal sensitivity and specificity.
Conclusion: Using age- and
gender-specific cutoffs for BMI, TSFT, WC or WHtR may offer putative
markers for early detection of hypertension.
Keywords: Anthropometry, Blood Pressure, Body
mass index, Waist circumference.
|
|
Children are becoming overweight and obese at
progressively younger ages throughout the world, both in high-income as
well as middle-and low-income populations [1]. Obesity is identified as
the most important risk factor affecting blood pressure (BP)
distribution in children [2,3]. Increasing evidence suggests that adult
BP is correlated with childhood BP and body size [4]. Normal range of BP
in childhood varies with age and gender [5].
Identifying risk of hypertension becomes difficult
for want of easy access to age- and gender-specific values. Considering
the strong correlations of anthropometric parameters such as body mass
index (BMI) and waist circumference (WC) with BP [6], an indirect
assessment of high BP using these indices may be an efficient strategy
in the community setup.
Excess body fat or adiposity is an important
cardio-metabolic risk factor than excess body weight per se.
Since BMI does not differentiate between fat and lean, other surrogate
measures of body fat distribution such as WC, triceps skin fold
thickness (TSFT), waist to height ratio (WHtR) are presently being
evaluated for their association with metabolic risk [7-10]. While WC is
a crude measure of intra abdominal fat, TSFT is predictive of body fat
and metabolic risk in children and adolescents [11-13]. Measurement of
Wrist circumference (WrC) is also an easy-to-detect clinical marker to
identify at risk children [14]. Although there are ethnic-specific
definitions for general and central obesity [15,16], few studies have
compared ability of various adiposity indices and provided age-gender
specific cut offs for screening children and adolescents for the risk of
hypertension.
Therefore, the objectives of the present study were (i)
to investigate relationships of BMI, WC, WHtR, TSFT and Wrist
circumference with BP; and (ii) to provide optimal cut off points
for these indices for detecting hypertension.
Methods
The study was performed in schools from five major
Indian cities (Chennai, Delhi, Kolkata, Pune and Raipur), between July
2011 and January 2012). Schools were randomly selected from the list of
private schools catering to well-off families in each city. The mean
yearly fees of the schools were INR 26,000 (15,000 to 54000). All
apparently healthy children from 6 to 18 years of age from the selected
school were included after informed written consent from parents and
assent from children. The exclusion criterion was children with
pre-existing serious illnesses. The study was approved by the ethics
committee of the Hirabai Cowasji Jehangir Medical Research Institute.
A single team led the data collection at each site
and equipments were calibrated daily. Mean inter-observer and
intra-observer coefficients of variation were both < 0.01(1%) for height
(Ht), Weight (Wt), Waist Circumference (WC), Tricep Skin fold Thickness
(TSFT), Wrist circumference and Blood Pressure measurements, and
differences between observers were not statistically significant.
Anthropometric measurements: Standing
height was measured using a portable stadiometer (Leicester Height
Meter, Child Growth Foundation, UK). Weight was measured using
electronic scales (Salter, India) measuring up to 100 g. BMI categories
were defined as (a) Normal weight, (b) Overweight and (c)
Obese using contemporary Indian data [17] and height for age, weight for
age and BMI for age z-scores were computed using Indian reference data
[18]. WC was measured in standing position, by a stretch resistant tape
which was applied horizontally just above the uppermost lateral border
of the right ileum using NHANES protocol [19]. WC above 90th centile of
available reference population [20,21] was considered as Adipose. Waist
to height ratio (WHtR) was computed and Optimal cut-off value of 0.44
WHtR for children and adolescents was used to classify children as
normal or adipose [22]. TSFT was recorded using Harpenden calliper, on
the non-dominant upper arm as per standard protocol [23]. Children were
classified as normal (< 85th centile), moderate (85th -95th) and excess
fat (>95th centile) with respect to references centiles. In absence of
Indian reference data for TSFT, Western cut-Offs were used [24].
Similarly, Wrist circumference was measured using
stretch resistant tape using NHANES protocol [19]. The most prominent
aspect of the radial styloid process was located with the middle or
index finger of the left hand. Firm pressure was applied and the
circumference was recorded to the nearest 0.1 cm [19]. Average of two
readings for all parameters was used for analysis.
Clinical assessments were carried out by
pediatricians. BP was recorded with children sitting and the cubital
fossa supported at heart level, after at least 5 minutes rest. BP was
measured using a mercury sphygmomanometer, with appropriate cuff. In
case of a high reading, BP was measured again after an interval of 10
minutes and also confirmed by another investigator. Systolic BP (SBP)
and/or Diastolic BP (DBP) >90th percentile and <95 th
percentile was considered as pre-hypertension; and SBP and/or DBP >95th
percentile were classified as hypertensive [5]. To account for changes
in anthropometric measures and later growth spurt in boys following age
groups were defined: boys 6-12, 13-15, 16-18yrs; girls 6-9, 10 -14,
15-18 yrs [25].
Children with persistently high BP underwent a
further diagnostic workup for causes of hypertension including familial,
renal, obesity, etc.; children with pre hypertension were managed on
diet and lifestyle changes, while those with blood pressure above the
95th percentile were either advised the same and followed up or were
initiated on therapy with anti-hypertensive treatment [5].
Statistical methods: SPSS version 20.0 (Chicago,
2011) was used for analysis. All results are expressed as mean (SD).
Correlations were estimated (unadjusted and after age adjustment)
separately for both genders to examine association of anthropometric
measurements with BP. Level of significance was set at P<0.05.
Two separate multiple logistic regression models adjusted for age and
gender were used to examine relationship of hypertension with BMI
categories, TSFT classes and Wrist with WC categories in the first
model, and with WHtR categories in the second model to avoid
multi-collinearity. Receiver-operating characteristic (ROC) curve
analysis was performed to evaluate the accuracy of each index (i.e.,
BMI, WC, WHtR, TSFT, WrC) to discriminate between presence or absence of
hypertension. The area under each ROC curve (AUC) and 95% confidence
intervals (CI) were estimated to compare the relative ability of various
anthropometric indices to identify risk of high BP. Optimal cut-off
points for each anthropometric indicator were determined [26,27]. The
differences between area under ROC curves for BMI, WC, WHtR, TSFT and
WrC to determine the best predictor for hypertension was tested [28].
Results
Age-and gender-wise anthropometric characteristics of
children aged 6-18 years (total 6380, 3501 boys) are described in
Table I. In each age group, boys had higher mean values of Ht,
Wt, BMI, WC, WrC and BP than girls (P<0.05) except for TSFT.
TABLE I Characteristic of Study Population According to Age Groups
|
Boys |
(6-12 yrs ) (1731) |
(13-15 yrs) (1417) |
(16-18 yrs)(375) |
All (6-18yrs) (3501) |
|
Age (years) |
9.1 ± 1.7 |
13.8 ± 1.1a |
16.7 ± 0.6b,c |
11.8 ± 3.1 |
|
Height (cm)
|
132.4 ± 11.4 |
159.6 ± 10.2a
|
170 ± 6.7b,c |
147.4 ± 18.3* |
|
Weight (kg)
|
29.6 ± 9.2 |
49.8 ± 12.9a |
60.2 ± 12.4b,c |
40.9 ± 16.1* |
|
BMI (kg/m2) |
16.5 ± 3 |
19.3 ± 3.8a |
20.8 ± 3.7b,c |
18.1 ± 3.8 |
|
Height for age Z score |
-0.2 ± 1.1 |
-0.1 ± 1 |
-0.7 ± 0.9
|
-0.2 ± 1 |
|
Weight for age Z score |
-0.2 ± 1.4 |
0 ± 1.3 |
-0.5 ± 1.4
|
-0.2 ± 1.3 |
|
BMI for age Z scores |
-0.2 ± 1.5 |
0 ± 1.5
|
-0.1 ± 1.4
|
-0.1 ± 1.5 |
|
Waist (cm) |
65.1 ± 8.4 |
78 ± 9.2a |
82 ± 8.6b,c |
72.1 ± 11.2 |
|
Waist to height Ratio (WHtR) |
0.5 ± 0.1 |
0.5 ± 0.1 |
0.5 ± 0.1 |
0.5 ± 0.1 |
|
Wrist (cm) |
12.5 ± 1.2 |
14.3 ± 1.2a |
14.9 ± 0.9b,c |
13.5 ± 1.6* |
|
Tricep Skin Fold Thickness (mm) |
10.6 ± 5 |
11.9 ± 6.4a |
11.0 ± 5.7 |
11.1 ± 5.7* |
|
Systolic BP (mm/Hg)
|
98.5 ± 10.5 |
109.6 ± 10.5a |
115.1 ± 9.4b,c |
104.8 ± 12.2 |
|
Diastolic BP (mm/Hg)
|
66.2 ± 7.8 |
72.2 ± 7.8a |
75.4 ± 6.6b,c |
69.6 ± 8.4 |
|
Girls |
(6-9 yrs)(811) |
(10- 14 yrs) (1199) |
(15-18 yrs) (869) |
All (6-18 yrs) (2879) |
|
Age (years) |
7.9 ± 1.1 |
12 ± 1.2 a |
15.6 ± 1.1 b,c |
11.9 ± 3.1 |
|
Height (cm)
|
125.1 ± 8.3 |
148.1 ± 9.3 a |
156.4 ± 6.1 b,c |
144.1 ± 14.9 |
|
Weight (kg)
|
25.1 ± 6.7 |
40.9 ± 10.1 a |
50.9 ± 9.8 b,c |
39.4 ± 13.5 |
|
BMI (kg/m2) |
15.8 ± 2.9 |
18.4 ± 3.3 a |
20.7 ± 3.6 b,c |
18.4 ± 3.8 |
|
Height for age Z score |
-0.2 ± 1.1 |
-0.2 ± 1.0 |
-1.0 ± 1.0 b |
-0.4 ± 1.1 |
|
Weight for age Z score |
-0.4 ± 1.4 |
-0.1 ± 1.2 |
-0.6 ± 1.3 b |
-0.4 ± 1.3 |
|
BMI for age Z scores |
-0.4 ± 1.4 |
-0.1 ± 1.3 |
0 ± 1.3 |
-0.2 ± 1.4 |
|
Waist (cm) |
61.9 ± 7.6 |
73.5 ± 8.7 a |
79.6 ± 8.7 b,c |
72.1 ± 10.8 |
|
Waist to height Ratio (WHtR) |
0.5 ± 0.1 |
0.5 ± 0.1 |
0.5 ± 0.1 |
0.5 ± 0.1 |
|
Wrist (cm) |
11.7 ± 1 |
13.2 ± 1.1 a |
13.5 ± 1 b,c |
12.8 ± 1.3 |
|
Tricep Skin Fold Thickness (mm) |
11 ± 4.4 |
14.0 ± 5.4 a |
15.9 ± 5.7 b,c |
13.7 ± 5.6* |
|
Systolic BP (mm/Hg)
|
95.6 ± 9.7 |
105.7 ± 10.3 a |
110.7 ± 9.4 b,c |
104.4 ± 11.5 |
|
Diastolic BP (mm/Hg)
|
64.6 ± 7.5 |
70.2 ± 7.9 a |
73.5 ± 7 b,c |
69.6 ± 8.3 |
|
!Values are expressed as mean ± SD. * significantly
different than other age matched gender, p<0.05; aGroup
II significantly higher than group I , p<0.05; bGroup
III significantly higher than group I, p<0.05; cGroup
III significantly higher than group II. p<0.05. |
A significant positive association (r=0.85) was
observed between BMI and WC in boys and girls within each age group (P<0.001).
Correlations of BMI with TSFT and WHtR were 0.78 to 0.80, respectively
across age groups in both genders (P<0.001). BMI showed higher
correlation with Wrist (r= 0.70) in younger age group which reduced to
0.6 and then to 0.45 in older groups (P<0.001). WC was positively
correlated with TSFT (r = 0.67 - 0.74, P<0.001) and Wrist (r=
0.41 - 0.78, P<0.001) in both genders across all groups (Data not
shown).
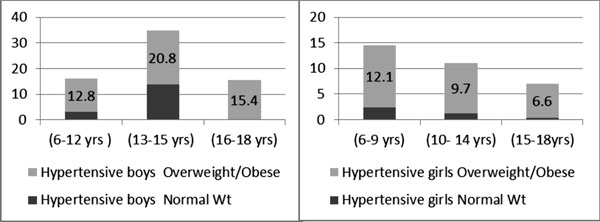
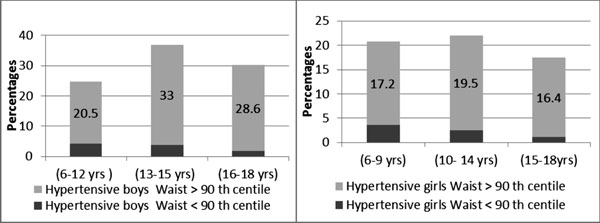
Overall prevalence of hypertension was higher in boys
(6.7%) than girls (4.2%) (P<0.05) with higher percentage in the
younger age groups than older age group. Prevalence was also higher in
overweight/obese than normal girls (P<0.05) which decreased with
increasing age. In boys, prevalence of hypertension amongst
overweight/obese was higher from 13-15yrs (Fig. 1 and 2).
 |
|
Fig. 1 Prevalence of hypertension
across BMI category in boys and girls.
|
 |
|
Fig. 2 Prevalence of hypertension
across the waist centile categories in boys and girls.
|
Gender wise correlations between SBP, DBP and
anthropometric indices are presented in Table II. All
correlations were positive and significant (P<0.001). In both
genders, correlation coefficients for BMI and WC with SBP were around
0.5 (P<0.001). WHtR showed a low correlation with SBP and DBP in
both genders.
TABLE II Correlation Between Systolic BP (Diastolic BP) and Anthropometric Indices in Boys and Girls
|
Anthropometric
|
Boys |
Girls |
|
Index |
6-12 yr |
13-15 yr |
16-18 yr |
6-9 yr |
10-14 yr |
15-18 yr |
|
BMI |
0.53 (0.34) |
0.57 (0.45) |
0.59 (0.46) |
0.45 (0.29) |
0.57 (0.41) |
0.47 (0.42) |
|
Waist |
0.58 (0.39) |
0.52 (0.41) |
0.48 (0.35) |
0.46 (0.28) |
0.55 (0.40) |
0.40 (0.33) |
|
WHtR |
0.31 (0.21) |
0.31 (0.29) |
0.42 (0.29) |
0.28 (0.17) |
0.41 (0.29) |
0.34 (0.28) |
|
TSFT |
0.47 (0.30) |
0.37 (0.29) |
0.52 (0.34) |
0.45 (0.31) |
0.48 (0.35) |
0.27 (0.30) |
|
Wrist |
0.52 (0.37) |
0.46 (0.35) |
0.28 (0.24) |
0.42 (0.31) |
0.41 (0.32) |
0.25 (0.24) |
|
P<0.001 for all comparisons. |
Multiple logistic regression model 1 (adjustment:
age, gender) indicated that odds ratios (OR) for BMI categories, waist
centile classes, TSFT centile classes, and Wrist against high BP were
statistically significant (P<0.001) (Web Table I).
Overweight children showed double risk of hypertension and obese
children 7 times higher risk than normal weight children. TSFT >95th
centile showed almost 3 times risk and between 85th-95th double risk
than normal weight children. Higher WC (>90th centile) also exhibited
1.5 times risk and larger Wrist 1.26 times higher risk of hypertension.
The model 2 (WHtR in place of WC) showed that estimated risk of
hypertension was similar as 1.5 times in children with high WHtR (>0.44)
than normal WHtR (<0.44) children (P<0.0001). Thus all these
indices showed ability to predict risk of hypertension.
Table III describes the age- and
gender-specific optimal cut-off values and for each of the five
anthropometric indices in detecting the risk of high BP. With growing
age, all the body measurements showed increasing trend which is
reflected in higher cut offs for BMI, WC, WHtR, TSFT and WrC in older
age groups in both genders. Sensitivity and specificity of all the
indices were similar ranging from 60 to 90%. The Area under curve was
also significantly high, different from 0.5 for BMI, WC, WHtR, TSFT and
Wrist for both genders (Web Table II) indicating the
ability of these anthropometric indices for detecting the risk of high
BP. Overall comparison of the five indices in different age-gender
groups suggests that BMI, WC and TSFT are better indicators of risk of
hypertension.
Table III Cut-off Values of Anthropometric Indices for Prediction of Hypertension in Children
|
Anthropometric |
Group I |
Group II |
Group III |
|
Index |
Boy |
Girls |
Boys |
Girls |
Boys |
Girls |
|
BMI (kg/m2) |
17.5 |
16.1 |
21.8 |
19.2 |
26.1 |
22.7 |
|
Waist (cm) |
68 |
62 |
81 |
77 |
90 |
87 |
|
WHR |
0.50 |
0.51 |
0.53 |
0.51 |
0.53 |
0.55 |
|
TSFT (mm) |
10.6 |
13.3 |
14.5 |
16.8 |
17.4 |
18.4 |
|
Wrist (cm) |
12.9 |
12.1 |
14.8 |
13.5 |
15.9 |
13.7 |
|
Group I: 6-11 yr boys & 6-9 yr girls; Group II: 12-15 yr boys
& 10-14 yr girls: Group III: 16-18 yr boys & 15-18 yr girls.
|
Discussion
All five indices showed significant positive
association with BP and indicated that obese children were seven times
at risk of hypertension than normal-weight children. We have also
proposed age-gender specific cut-off values for these five
anthropometric indices. For boys, BMI, WC and TSFT showed similar
predictive power while in girls all five indices performed equally well.
The prevalence of hypertension in our study was
higher than that reported previously [9].
Further, the prevalence of high blood pressure was more
in boys than in girls, which is also reported by other studies [9].
Similar to earlier studies we also found that pubertal subjects had
higher prevalence of hypertension than pre-pubertal subjects [29].
Though studies describing prevalence of hypertension in various age
groups similar to ours are scarce, studies in obese children have shown
that cardiovascular risk factors worsen at onset of puberty and improve
in later puberty, a result similar to that seen in the current study
[30].
In the present study, we have provided cut-off values
for various anthropometric indices i.e. BMI, waist circumference,
WHtR, TSFT and for the first time for Wrist circumferences for detecting
risk of hypertension in Indian children. In a study on Brazilian
adolescents, cut-offs for BMI were in line with our cut-offs for girls
(14-18 yrs), though they were lower for boys [31]. For Iranian
adolescents, cut-offs for boys and girls were lower than those reported
in our study [32].
A limitation of the study is that children were
classified in age groups on consideration of conventional pubertal
development years. It was not possible to assess Tanner staging for each
child in the present study due to logistic reasons. Second limitation of
the study was non-availability of biochemical measurements, therefore
examining utility of these indices for screening other cardio-metabolic
risk factors was not possible. Thirdly we did not record family history
of hypertension, which may have some effect on the BP status of
children. Although even after adjusting for parental influence the risk
in children would be significant [33]. However, for community surveys,
screening for hypertension with non-invasive body measurements would go
a long way in prevention of risk of cardiovascular disease in adulthood.
To conclude, all five measures of adiposity were
significantly associated with risk of hypertension in a multi-centric
sample of Indian children and adolescents. Age-gender specific optimal
cutoffs for BMI, TSFT, WC, wrist circumference and WHtR measurements
presented in the study may be useful in screening for risk of
hypertension.
Acknowledgment: We thank Dr Archana Arya, Dr
Sanwar Agarwal, Dr Anjan Bhattacharya, Ms Veena Ekbote, Ms Lavnya
Parthasarathy and Mrs Surbhi Shah Kulkarni for their help throughout the
study. We acknowledge the help from the school authorities, and the
parents and students.
Contributors: NAK: designed the data collection
instruments and coordinated and supervised data collection at the sites,
carried out the analysis, drafted the initial manuscript; AVK:
conceptualized and designed the study, coordinated and supervised data
collection, carried out the initial analyses, reviewed and revised the
manuscript. She will act as guarantor of the study; SAC: conceptualized
and designed the study, carried out the analyses, reviewed and revised
the manuscript; VVK: conceptualized and designed the study, critically
reviewed the manuscript. The final manuscript was approved by all
authors.
Funding: Novo Nordisk India Pvt. Ltd.
Competing interests: None stated.
|
What is Already Known?
• Anthropometric parameters are positively
correlated with blood pressure.
What This Study Adds?
• Age- and gender-wise cutoffs are provided
for simple anthropometric indices such as BMI, Waist
Circumference, Waist to Height ratio, Tricep Skinfold thickness
and Wrist circumference for screening for risk of hypertension
in Indian children.
|
References
1. WHO Fact Sheet No. 311; Sept 2006. Obesity and
overweight. Geneva: World Health Organisation, 2006.
2. Urrutia-Rojas X, Egbuchunam CU, Bae S, Menchaca J,
Bayona M, Rivers PA, et al. High blood pressure in school
children: prevalence and risk factors. BMC Pediatr. 2006;6:32.
3. Srinivasan SR, Myers L, Berenson GS. Changes in
metabolic syndrome variables since childhood in pre hypertensive and
hypertensive subjects: the Bogalusa Heart Study. Hypertension.
2006;48:33-9.
4. Ho TF. Cardiovascular risks associated with
obesity in children and adolescents. Ann Acad Med Singapore.
2009;38:48-9.
5. National High Blood Pressure Education Program
Working Group on High Blood Pressure in Children and Adolescents. The
fourth report on the diagnosis, evaluation, and treatment of high blood
pressure in children and adolescents. Pediatrics. 2004;114:555-76.
6. Genovesi S, Antolini L, Giussani M, Pieruzzi F,
Galbiati S, Valsecchi MG, et al. Usefulness of waist
circumference for the identification of childhood hypertension. J
Hypertens. 2008;26:1563-70.
7. Santos R, Moreira C, Ruiz JR, Vale S, Soares-Miranda
L, Moreira P, et al. Reference curves for BMI, waist
circumference and waist-to-height ratio for Azorean adolescents
(Portugal). Public Health Nutr. 2012;15:13-9.
8. Yang X, Telama R, Viikari J, Raitakari OT. Risk of
obesity in relation to physical activity tracking from youth to
adulthood. Med Sci Sports Exerc. 2006;38:919-25.
9. Beck, Cristina C, et al. Cardiovacular risk
factors in adolescents from a town in the Brazilian South: prevalence
and association with sociodemographic variables. Revista Brasileira de
Epidemiologia. 2011;36-49.
10. Plachta-Danielzik S, Landsberg B, Johannsen M,
Lange D, Müller MJ. Association of different obesity indices with blood
pressure and blood lipids in children andadolescents. Br J Nutr.
2008;100:208-18.
11. Bedogni G, Iughetti L, Ferrari M, Malavolti M, Poli
M, Bernasconi S, et al. Sensitivity and specificity of body mass
index and skinfold thicknesses in detecting excess adiposity in children
aged 8-12 years. Ann Hum Biol. 2003;30:132-9.
12. Freedman DS, Dietz WH, Srinivasan SR, Berenson
GS. The relation of overweight to cardiovascular risk factors among
children and adolescents: the Bogalusa Heart Study. Pediatrics.
1999;103:1175-82.
13. Hansen SE, Hasselstrøm H, Grønfeldt V, Froberg K,
Andersen LB. Cardiovascular disease risk factors in 6-7-year-old Danish
children: the Copenhagen School Child Intervention Study. Prev Med.
2005;40:740-6.
14. Capizzi M, Leto G, Petrone A, Zampetti S, Papa
RE, Osimani M, et al. Wrist circumference is a clinical marker of
insulin resistance in overweight and obese children and adolescents.
Circulation. 2011;123:1757-62.
15. Alberti, K. George MM, Paul Z, Shaw J. The
metabolic syndrome–a new worldwide definition. Lancet. 2005;366:
1059-62.
16. Eckel RH, Grundy SM, Zimmet PZ. The metabolic
syndrome. Lancet. 2005; 365(9468):1415-28.
17. Khadilkar VV, Khadilkar AV, Borade AB, Chiplonkar
SA. Body mass index cut-offs for screening for childhood overweight and
obesity in Indian children. Indian Pediatr. 2012;49:29-34.
18. Khadilkar VV, Khadilkar AV, Cole TJ, Sayyad MG.
Cross-sectional growth curves for height, weight and body mass index for
affluent Indian children, 2007. Indian Pediatr. 2009; 46:477-89.
19. National Center for Health Statistics. Plan and
operation of the Third National Health and Nutrition Examination Survey,
1988-94. Series 1: programs and collection procedures. Vital Health
Stat. 1994;32:1-3,18, 20-22.
20. National Health and Nutrition Examination Survey
(NHANES) Anthropometry Procedures Manual. Waist circumference and
waist–hip ratio: report of a WHO expert consultation, Geneva, 8-11,
2008.
21. Fernández JR, Redden DT, Pietrobelli A, Allison
DB. Waist circumference percentiles in nationally represen-tative
samples of African-American, European-American, and Mexican-American
children and adolescents. J Pediatr. 2004;145:439-44.
22. Ribeiro RC, Coutinho M, Bramorski MA, Giuliano
IC, Pavan J. Association of the waist-to-height ratio with
cardiovascular risk factors in children and adolescents: The three
cities heart study. Int J Prev Med. 2010;1:39-49.
23. Harrison G, Buskirk E, Carter J Johnston F,
Lohmant T, Pollock M, et al. Skinfold Thickness and Measurement
Technique. In: Lohman T, Roche AF, Martorell R, eds.
Anthropometric standardization reference manual. Champaign, IL: Human
Kinetics Books, 1988.
24. Addo OY, Himes JH. Reference curves for triceps
and subscapular skinfold thicknesses in US children and adolescents. Am
J Clin Nutr. 2010;91:635-42.
25. Desai MP, Colaco P. Growth Hormone Deficiency and
Insensitivity. In: Desai MP, Menon PSN, Bhatia V, eds. Pediatric
Endocrine Disorders. 2nd ed. Hyderabad, Universities Press (India) Pvt.
Ltd; 2008:188-92.
26. Van der Schouw YT, Verbeek AL, Ruijs JH. ROC
curves for the initial assessment of new diagnostic tests. Fam Pract.
1992;9:506-11.
27. Farr BM, Shapiro DE. Diagnostic tests:
distinguishing good tests from bad and even ugly ones. Infect Control
Hosp Epidemiol. 2000;21:278-84.
28. DeLong ER, DeLong DM, Clarke-Pearson DL.
Comparing the areas under two or more correlated receiver operating
characteristic curves: a nonparametric approach. Biometrics.
1989;44:837-45.
29. Liang Y, Mi J. Pubertal hypertension is a strong
predictor for the risk of adult hypertension. Biomed Environ Sci.
2011;459-66.
30. Reinehr T, Toschke AM. Onset of puberty and
cardiovascular risk factors in untreated obese children and adolescents:
a 1-year follow-up study. Arch Pediatr Adolesc Med. 2009;163:709-15.
31. Beck CC, Lopes A, Pitanga F. Anthropometric
indicators as predictors of high blood pressure in adolescents. Arq Bras
Cardiol. 2011;96:126-33.
32. Kelishadi R, Gheiratmand R, Ardalan G, Adeli K,
Mehdi Gouya M, Mohammad Razaghi E, et al. Association of
anthropometric indices with cardiovascular disease risk factors among
children and adolescents: CASPIAN Study. Int J Cardiol. 2007; 2;340-8.
33. Khadilkar AV, Chiplonkar SA, Pandit DS, Kinare
AS, Khadilkar VV. Metabolic risk factors and arterial stiffness in
Indian children of parents with metabolic syndrome. J Am Coll Nutr.
2012;31:54-62.
|
|
|
 |
|

