|
|
|
Indian Pediatr 2013;50:
649-653 |
 |
Comparison of Analgesic Effect of Direct Breastfeeding, Oral
25% Dextrose Solution and Placebo during 1 st
DPT Vaccination in Healthy Term Infants:
A Randomized,
Placebo Controlled Trial
|
|
Gaurav Goswami, Amit Upadhyay, Navratan Kumar Gupta,
Rajesh Chaudhry,
*Deepak
Chawla and #V Sreenivas
From the Departments of Pediatrics, LLRM, Medical
College, Meerut, UP, and *Government Medical College, Chandigarh; and
#Department of Biostatistics, All India Institute of Medical Sciences,
New Delhi, India.
Correspondence to: Dr Amit Upadhyay, Head, Department
of Pediatrics, LLRM Medical College, Meerut,UP.
Email: [email protected]
Received: January 14, 2012;
Initial review: February 15, 2012;
Accepted: November 12, 2012.
PII: S097475591200052
|
Objective: To compare analgesic effect of direct breast feeding, 25%
dextrose solution and placebo as we give 1st intramuscular whole cell
DPT injection to 6week - 3month old infants.
Design: Randomized, placebo controlled trial.
Setting: Immunization clinic of Department of
Pediatrics, LLRM Medical College.
Participants: Infants coming for their 1st DPT
vaccination were randomized in to three groups of 40 each.
Outcome measures: The primary outcome variable
was the duration of cry after vaccination. Secondary outcome variables
were Modified Facial Coding Score (MFCS) and latency of onset of cry.
Results: 120 babies were equally enrolled in
breast feed group, 25% dextrose fed group and distilled water fed group.
Median (interquartile range) of duration of cry was significantly lower
in breast fed (33.5 (17-54) seconds) and 25% dextrose fed babies (47.5
(31-67.5) seconds) as compared to babies given distilled water (80.5
(33.5-119.5) seconds) (P<0.001). MFCS at 1 min and 3 min was
significantly lower in direct breast fed and dextrose fed babies.
Conclusions: Direct breastfeeding and 25%
dextrose act as analgesic in young infants undergoing DPT vaccination in
young infants less than 3 month of age.
Keywords: 25% dextrose, Breastfeeding, Duration of cry, DPT
vaccination, Management, Pain, Infant.
|
|
Many newborn babies undergo painful procedures
like heel pricks, venepuncture and intramuscular injection for
immunization. Such procedures inflict distinct physiological, behavioral,
hormonal and metabolic changes [1]. Grunau and Craig have shown that
first cry following pain is most sensitive to noxious stimuli [1]. Great
emphasis is being laid in minimizing pain during these minor procedures
in neonates. Duration of cry has been widely used in various studies as
a marker of severity of pain [1-3].
Dextrose and sucrose in varying concentration have been
shown to relieve pain during venepuncture or intramuscular injection
[4-8]. Evidence is emerging that breastfeed/breastmilk has analgesic
properties [9-13]. We planned a study with the objective to compare the
efficacy of anti-nociceptive effect of breastfeeding and oral 25%
dextrose, 2 minutes before DPT vaccination, using distilled water as
placebo.
Methods
The study was carried out in the immunization clinic
of Department of Pediatrics, LLRM Medical College, Meerut. Healthy term
infants less than three months of postnatal ages, who were on exclusive
or partial breast-feed and attended the immunization clinic for first
DPT vaccine were included. The following babies were excluded: infants
who have required hospital admission for more than 48 hrs, perinatal
asphyxia (5 min Apgar score <5) or delayed cry (> 5min) if born at home,
intra-uterine growth retardation (IUGR) (wt <10th centile for
gestational age), preterm deliveries (<37 week of gestation),
developmental delay (developmental age lags behind post-conceptional age
by 1 months) and previous surgery. The subjects were randomized into
three groups of 40 each through computers generated random numbers and
put in serially numbered opaque sealed envelopes (SNOSE method). The
person generating random numbers and placing them serially in sealed
envelope was not involved in the study.
The name, age, sex, weight, height, and head
circumference were recorded in a pre-structured proforma. Babies were
brought to the room where vaccination was to be done. At recruitment,
one person opened the sealed envelope and administered the allotted
intervention, as above, in all the babies. Breastfeed group:
Babies in breastfeed group were breastfed throughout the intervention,
starting 2 minutes prior to the vaccination; 25% dextrose group:
2 ml of 25% dextrose was given orally by a sterile syringe 2 minutes
prior to intramuscular vaccination; Placebo group: 2 ml distilled
water was given orally by a sterile syringe 2 minutes prior to
intramuscular vaccination. All the babies received the intervention from
one investigator only; another two investigators would then come in the
immunization room. One administered 0.5 ml of wDPT vaccine by a 2 mL
syringe with 23 G 1" needle on anterolateral aspect of thigh
(left/right) after cleaning the skin with spirit. The injection was
given with the baby in the mothers lap, with thigh exposed, after
calling aloud "in" when the needle was inserted, and "out" when the
needle was removed. All events were recorded by the investigator on a
digital video camera (model Sony CCD-TRV238E) for total duration of
three minutes from the removal of the needle. A different investigator
analyzed the outcome variables from the video recording in all our
subjects. All the four investigators performed the same role in all the
enrolled babies. Three investigators were blinded to the pharmacological
intervention given to the baby; however, none was blinded to the
intervention of "breastfeeding".
Outcome variables: Primary outcome variable was
the duration of cry (in seconds) after vaccination. It was defined as
duration of continuous distressed vocalization (cry) after needle
insertion to the period of silence of more than 5 second, excluding
these 5 seconds. As video recording was done only for 3 minutes, the
babies who were still crying even after 3 minutes, the duration of cry
was noted as 180 seconds only. Secondary outcome variables
were the latency of onset of cry and Modified Neonatal Facial Coding
Score (MFCS) [9]. Latency of onset of cry (in seconds) was
defined as the period between insertion of needle, marked by the sound
"in" and the onset of vocalization, in form of cry. The MFCS was
calculated immediately and after 1 and 3 minutes of needle insertion.
This was a composite score obtained from the sum of the following: brow
bulge, eye squeeze, nasolabial furrow, open mouth, chin quiver, and
trunk movement. Each parameter was scored "0" if absent and "1" if
present and the total score was obtained. One observer was responsible
for giving the scores in all the babies. During breastfeeding, only one
half of the face was visible; thus, all facial parameters were based on
the facial side which observer could see. We included only healthy term
infants without any neurological deficits, movements and facial
expression of the face in these babies will be symmetrical, unless
facial nerve palsy is present. However, if for some reason, any
parameter could not be seen on both sides, a zero score was given to
that parameter.
In order to avoid confounding by other pain relieving
methods, the following steps were ensured. All enrolled babies had been
fed within 3 hours prior to the interventions but had not received a
feed in the previous 30 minutes. All babies were held in their mother’s
lap during vaccination. The mothers were allowed to hold, talk to, or
rock the baby during the procedure in all the groups. Since the state of
wakefulness could have modified the response, the procedure was done in
awake babies. If baby was sleeping, he was gently awakened; if he cried,
he was soothed to quite wakefulness before the procedure. Non-nutritive
sucking was not done during the procedure. All the tests were performed
between 10 am to 1 pm to avoid diurnal variation in pain response.
Written informed consent was taken from the parents and the ethical
clearance was taken from Ethical Committee of the College.
Duration of cry was the primary outcome variable and
sample size was calculated for this variable. 40 cases in each group
were required to attain a power of 90% with test significance of 0.05.
Results were analyzed using STATA 9.1 software. Analysis of continuous
data with normal distribution was done by one-way ANOVA test followed by
Bonferroni correction for multiple analyses of data, and non-normally
distributed data by Kruskal- Wallis test. Categorical data was be
analyzed by Chi-square test.
Results
A total of 150 eligible babies were approached, of
which 30 were excluded (25, not meeting exclusion criteria; 5, refusal
to participate). 120 babies were randomized into 3 groups of 40 babies
each. The postnatal age, number of prior injections, sex ratio, time to
last feed, and duration of needle insertion was comparable in all three
groups (Table I).
TABLE I Baseline Demographic Characteristics of the Study Subjects, Mean (SD)
|
Parameter |
Direct
|
25%
|
Distilled
|
|
breast |
Dextrose |
water
|
|
feeding
|
(n=40) |
(n=40) |
|
(n=40) |
|
|
|
Age (wks) |
10.2 (2.4) |
10.3 (2.2) |
10.1 (1.8) |
|
Weight (kg) |
4.6 (0.4) |
4.6 (0.5) |
4.4 (0.4) |
|
Time since last feed (min) |
45(8.2) |
39 (4.3) |
47 (9.2) |
|
Duration of needle insertion (s) |
2.9 (0.6)
|
3.0 (0.5) |
2.8 (0.4) |
Median (interquartile range) of duration of cry was
significantly lower in direct breast fed 33.5 (17-54) seconds and 25%
dextrose fed babies 47.5 (31-67.5) seconds as compared to babies given
distilled water 80.5 (33.5-119.5) seconds (P<0.05). Significantly
fewer babies had duration of cry in 0-60 seconds range in the two
interventions groups as compared to placebo group (Table II).
TABLE II Duration of Cry in the three Groups After DPT Vaccination
|
Cry |
Direct |
25% Dextrose
|
Distilled |
P value
|
|
duration |
breast
|
solution |
water |
|
|
(s) |
feeding |
|
|
|
|
0-60
|
33 |
28 |
15 |
<0.001 |
|
61-120
|
5 |
10 |
18 |
<0.05 |
|
121-180
|
2 |
1 |
4 |
>0.05 |
|
>180
|
0 |
1 |
3 |
>0.05 |
|
Median |
33.5 |
47.5 |
80.5 |
<0.05 |
|
(IQR) |
(17-54) |
(31-67.5) |
(33.5-119.5) |
|
The difference in latency of cry in the breast fed,
dextrose and placebo groups were 2.1 (1.2) seconds, 2.2 (1.2) seconds
and 1.8 (0.75) seconds (P>0.05) [WebTable 1] at 1
min and 3 min was significantly lower in direct breast fed and dextrose
fed babies. There was no statistically significant difference in MFCS
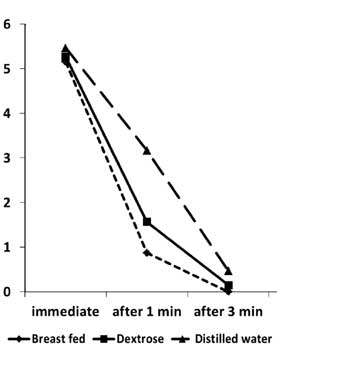
immediately after needle insertion (Fig. 1).
 |
|
Fig. 1 Line diagram depicting Modified
Facial Coding Score.
|
Discussion
Our study demonstrated that babies who were directly
breastfed or given 25% dextrose had significantly shorter duration of
cry, and lower pain score at 1min and 3min after needle insertion, as
compared to placebo.
Numerous non-pharmalogical intervention have been
tried to reduce pain of vaccination and minor procedures. Ingestion of
sucrose decreases pain in term and preterm infants [4-8]. A systematic
review reported that 25% sucrose was effective in alleviating minor
procedural pain in neonates [5]. Upadhyay, et al. [9] and Uyan,
et al. [10] have earlier demonstrated that expressed breast milk
given 2 minutes prior to venepuncture significantly reduced pain in term
infants. Osinaike, et al. [11]. have demonstrated that
breastfeeding reduces pain in neonates during venepuncture. Singh, et
al. [12] have shown that exclusively breastfed babies
perceive lesser pain during intramuscular injection than partially or
non breastfed babies, even without any physiological or medical
intervention during vaccination. This is probably because babies who are
exclusively breast fed are better developed neurologically and
physically. They probably can tolerate noxious stimuli better as
compared to top fed infants. Uga, et al. have evaluated analgesic
effect of breastfeeding during heel puncture in newborn [13]. Others
have demonstrated analgesic effects of skin-to-skin contact in
procedural pain in healthy term neonates [17, 18]. Efe and Ozer
hypothesized that following mechanisms could be attenuating the pain
response while direct breastfeeding the baby during the painful
procedure [19]. Firstly, suckling at the breast stimulates the infant’s
oropharyngeal tactile and mechanoreceptor and focuses attention on the
mouth, reducing outside influences. Secondly, the sweet flavour of milk
stimulates the release of opioids in midbrain of infant which act on
receptor that decrease the perception of pain. Thirdly, breastfeeding
involves maternal skin to skin contact which stabilizes blood glucose
level, body temperature and respiratory rate and reduces release of
stress hormone [20]. Finally, breastfeeding involves intimate social
interaction between mother and child and may release antistress hormone,
oxytocin [21]. The mechanism of relaxation and analgesia probable works
synergistically [22, 23]. During breastfeeding, only half of face is
visible but facial scores can be interpreted due to symmetry of facial
response.
Previous studies have demonstrated pain relief with
dextrose in varying concentrations, but no other previous study has
directly compared analgesic effect of breastfeeding and dextrose.
Skogsdal, et al. [14] reported reduction in crying time by 75% in
babies receiving 30% glucose compared to no treatment group and the
effect was lesser with 10% glucose. Ramenghi, et al. [15] found
hydrogenated glucose solution as effective as 25% or 50% sucrose in
reducing crying time and duration of first cry. A recent Cochrane review
has also concluded that if available, breastfeeding or breastmilk should
be used to alleviate procedural pain in neonates undergoing a single
painful procedure compared to placebo, positioning or no intervention
[23].
One of the limitations of our trial design is the
lack of blinding. In breastfeeding studies, it is not possible to
"blind" subjects as it is quite evident during video recording. In this
case, a potential bias in the pain score evaluation could be introduced.
Other limitation is that we have not taken physiological parameter of
pain assessment (heart rate, respiratory rate, oxygen saturation) into
account. However, previous studies have also used pure behavioral scales
in older children. We avoided use of physiological parameters because
pulse oxymeters often do not give readings in crying and vigorous baby
and attaching chest leads to healthy babies in immunization rooms can be
intimidating and stressful the parents.
Though MFCS has been reported to be used only in
neonatal age group, we extrapolated its use in early infancy, as the
physiological characteristics of babies in this age group are similar.
However, it should have been validated for ages beyond neonatal period.
We also used other parameters of pain assessment (duration of cry),
which showed correlation to the MFCS.
Direct breastfeeding and oral dextrose have
antinociceptive effect during intramuscular whole cell DPT vaccination.
This effect is probably more for direct breastfeeding during vaccination
than oral feeding of 25% dextrose 2 minutes before vaccination.
Contributors: AU: planned, supervised the study
and reviewed manuscript. He will act as guarantor of study; GG, NG and
RC: conducted study, collected data, reviewed literature and prepared
manuscript; VS and DC: data analysis, critically revised the manuscript
for important intellectual content
Funding: None; Competing interest: None
stated.
|
What is Already Known?
• Breastmilk, breastfeeding, and sweet
solutions have pain relieving effects in minor outpatients
procedures and injections.
What This Study Adds?
• Breastfeeding during and before
intramuscular DPT injection is as good as 25% dextrose as an
analgesic in infants younger than three months.
|
References
1. Grunau RVE, Graig KD. Pain expression in neonates;
facial action and cry. Pain. 1987;28: 395-410.
2. Barr RG. Reflections on measuring pain in infants:
Dissociation in responsive systems and "honest signaling". Arch Dis
Child Fetal Neonatal Ed. 1998;79:F 152-6.
3. Anand KJ. International Evidence-Based Group for
Neonatal Pain. Consensus statement for the prevention and management of
pain in the newborn. Arch Pediatr Adolesc Med. 2001;155:173 –80.
4. Stevens B, Yamada J, Ohlsson A. Sucrose for
analgesia in newborn infants undergoing painful procedures. Cochrane
Database Syst Rev. 2010;1:CD001069.
5. Carbajal R, Chauvet X, Couderc S, Olivier-Martin
M. Randomised trial of analgesic effects of sucrose, glucose, and
pacifiers in term neonates. BMJ. 1999;319:1393-7.
6. Bucher HU, Baumgartner R, Bucher N, Seiler M,
Fauchère JC. Artificial sweetener reduces nociceptive reaction in term
newborn infants. Early Hum Dev. 2000;59:51-60.
7. Harrison D, Stevens B, Bueno M, Yamada J,
Adams-Webber T, Beyene J, et al. Efficacy of sweet solutions for
analgesia in infants between 1 and 12 months of age: a systematic
review. Arch Dis Child Fetal Neonatal Ed. 2010;95:406-13.
8. Stevens B, Taddio A, Ohlsson A, Einarson T. The
efficacy of sucrose for relieving procedural pain neonates- a systemstic
review and metaanalysis. Acta Pediatr. 1997;86:837-42.
9. Upadhyay A, Aggarwal R, Narayan S, Joshi M, Paul
VK, Deorari AK. Analgesic effect of expressed breast milk in procedural
pain in term neonates: a randomized, placebo-controlled, double-blind
trial. Acta Paediatr. 2004;93:518-22.
10. Uyan ZS, Ozek E, Bilgen H, Cebeci D, Akman I.
Effect of foremilk and hindmilk on simple procedural pain in newborns.
Pediatr Int. 2005;47:252-7.
11. Osinaike BB, Oyedeji AO, Adeoye OT, Dairo MD,
Aderinto DA. Effect of breastfeeding during venepuncture in neonates.
Ann Trop Paediatr. 2007;27:201-5.
12. Singh VB, Mishra SK, Singh T, Upadhyay A.
Antinociceptive effect of exclusive breastfeeding in healthy term
infants during vaccination. Early Human Development. 2008;84: 50-1.
13. Uga E, Candriella M, Perino A, Alloni V,
Angilella G, Trada M, et al. Heel lance in newborn during
breastfeeding: an evaluation of analgesic effect of this procedure. Ital
J Pediatr. 2008; 34:3.
14. Skogsdal Y, Erricson M, Schollin. Analgesia in
newborns given oral glucose. Acta Pediatr. 1997;86:217-20.
15. Ramenghi LA, Wood CM, Griffith GC, Levene MI.
Reduction of pain response in premature infants using intraoral sucrose.
Arch Dis Child Fetal Neonatal Ed. 1996;74:F126-8.
16. Gonsolves S, Mercer J. Physiological correlates
of painful stimulation in preterm infants. Clin J Pain. 1993;9:88-93.
17. Gray L, Watt L, Blass EM. Skin-to-skin contact is
analgesic in healthy newborns. Pediatrics. 2000;105:252-7.
18. Okan F, Ozdil A, Bulbul A, Yapici Z, Nuhoglu A.
Analgesic effects of skin-to-skin contact and breastfeeding in
procedural pain in healthy term neonates. Ann Trop Paediatr.
2010;30:119-28.
19. Efe E, Ozer ZC. The use of breast-feeding for
pain relief during neonatal immunization injections. Appl Nurs Res.
2007;20:10-6.
20. Phillips RM, Chantry CJ, Gallagher MP. Analgesic
effects of breast-feeding or pacifier use with maternal holding in term
infants. Ambul Pediatr. 2005;5:359-64.
21. Gray L, Miller LW, Philipp BL, Blass EM.
Breastfeeding is analgesic in healthy newborns. Pediatrics.
2002;109:590-3.
22. Codipietro L, Ceccarelli M, Ponzone A.
Breastfeeding or oral sucrose solution in term neonates receiving heel
lance: A randomized, controlled trial. Pediatrics. 2008;122:716-21.
23. Shah PS, Aliwalas L, Shah V. Breastfeeding or
breast milk to alleviate procedural pain in neonates: a systematic
review. Breastfeed Med. 2007;2:74-82.
|
|
|
 |
|

