|
reviews on child health priorities |
|
|
Indian Pediatr 2011;48:
537-546 |
 |
Community Based Newborn Care: A Systematic
Review and Meta-analysis of Evidence: UNICEF-PHFI Series on
Newborn and Child Health, India |
|
Siddhartha Gogia, *Siddarth Ramji, $Piyush Gupta,
#Tarun Gera, $Dheeraj Shah,
**Joseph L Mathew, $$Pavitra Mohan and
##Rajmohan Panda
From Department of Pediatrics, Max Hospital, Gurgaon,
Haryana; *Department of Pediatrics, Maulana Azad Medical College, Delhi;
$Department of Pediatrics, University College of Medical Sciences, New
Delhi; #Department of Pediatrics, Fortis Hospital, Shalimar Bagh,
New Delhi; **Advanced Pediatrics Centre, PGIMER, Chandigarh 160012;
$$UNICEF India, New Delhi, and ##Public Health Foundation of India (PHFI),
New Delhi; India.
Correspondence to: Dr Siddhartha Gogia, Department of
Pediatrics, Max Hospital, Gurgaon, Haryana, India.
Email:
[email protected]
|
Background: The neonatal mortality rate (NMR) in India has remained
virtually unchanged in the last 5 years. To achieve the Millennium
Development Goal (MDG) 4 on child mortality (two thirds reduction from
1990 to 2015), it is essential to reduce NMR. A systematic review of the
evidence on community-based intervention packages to reduce NMR is
essential for advocacy and action to reach MDG-4.
Objective: To assess the effect of community based
neonatal care by community health workers (CHWs) on NMR in
resource-limited settings.
Design: Systematic review and meta-analysis of
controlled trials.
Data sources: Electronic databases and hand search
of reviews, and abstracts and proceedings of conferences.
Results: A total of 13 controlled trials involving
about 192000 births were included in this systematic review. Community
based neonatal care by CHWs was associated with reduced neonatal mortality
in resource-limited settings [RR=0.73 (0.65 to 0.83); P<0.0001].
The identified studies were a heterogeneous mix with respect to the extent
and quality of community based neonatal care provided and the
characteristics of the CHWs delivering the intervention. There was no
consistent effect of training duration of the health workers, type of
intervention (home visitation versus community participatory action and
learning), number of home visits done by CHWs, and provision of only
preventive versus both preventive and therapeutic care. Limited data
suggests that the ideal time for the first postnatal visit is the first
two days of life. The interventions are highly effective when baseline NMR
is above 50/1000 live births [RR=0.64(0.54 to 0.77)]. The interventions
show a significant decrease in efficacy as the NMR drops below 50/1000
live births [RR=0.85 (0.73 to 0.99)], however is still substantial. NMR
gains from home visitation approach are going to materialize only in the
presence of high program coverage of 50% or more.
Conclusion: A significant decrease in NMR is
possible by providing community based neonatal care in areas with high NMR
by community health workers with a modest training duration and ensuring
high program coverage with home visitation on the first two days of life.
Keywords: Action, Advocacy, Newborn, Child health, Community,
Systematic reviews.
|
|
I
ndia contributes to about 20% of
global births with 27 million live births each year [1]. With about 2
million under-five annual deaths, India also accounts for a quarter of the
global child mortality [1]. The infant mortality rate (IMR) has declined
from 139/1000 live births in 1972 to 50/1000 live births in 2009 [2].
There are wide inter and intra state variations in infant and child
mortality; and between rural and urban India. For example, rural IMR is
55/1000 live births as opposed to an urban IMR of 34 per 1000 live births
[2]. A significant proportion of child deaths (over 50% of under-five
mortality and 66% of infant mortality) occur in the neonatal period [2].
According to 2008 estimates, out of the annual 1,829,826 under five
deaths, 1,003,767 (54.8%) occurred in the neonatal period. Early neonatal
mortality (25/1000 live births) accounts for 2/3 of neonatal mortality
[2]. Preterm birth (32.4%), neonatal infections (26.7), and complications
of birth asphyxia/trauma (18.9%) account for most neonatal deaths [3].
With the advent of Janani Suraksha Yojana (cash
incentive scheme for institutional delivery), certain important parameters
of maternal health have shown impressive gains; institutional delivery has
increased to 72.9%, safe delivery by skilled birth attendants has
increased to 76%, and mothers who had 3 or more antenatal check-ups has
also increased to 68.7% [4]. However, 46% of mothers stay for less than or
equal to 1 day at the health facility after childbirth [4]. Majority of
neonatal deaths are occurring at home, within the first few days of life,
against a backdrop of rural poverty, unskilled neonatal care, and probable
suboptimal/absent referral system. Only 22.2% neonatal deaths occur in a
health facility [3].
The Millennium Development Goal (MDG)-4 on child
mortality for India aims for a two-thirds reduction in IMR from the 1990
level of 84/1000 live births to 28/1000 live births by 2015. The National
Rural Health Mission (NRHM) in India has set itself the goal of reducing
IMR to 30/1000 live births by 2012. However, at the present rate of
decline in IMR, the likelihood of achieving these targets appears
unlikely, given that two-thirds of infant deaths are contributed by
neonatal deaths, wherein the mortality decline has been woefully small.
Since utilization of health facilities for neonatal health is low, there
is a need to review the potential complementary role for community based
newborn care in accelerating the decline in neonatal deaths to achieve the
MDG-4 goals. Recent reviews have evaluated the efficacy and
cost-effectiveness of individual interventions in reducing neonatal
mortality, and packages of interventions have been proposed for wide-scale
implementation [5]. However, there are only a few systematic reviews on
community health interventions for newborn survival [6]. This systematic
review was undertaken to assess the effect of community based neonatal
care interventions on neonatal mortality in resource-limited settings, and
explore its relevance for India.
Methods
Inclusion Criteria for Trials
Type of trials: Trials (randomized or
quasi-randomized) evaluating interventions including community based
neonatal care by community health workers, with individual or cluster
allocation, were eligible for inclusion. Trials evaluating specific
community based interventions e.g. micronutrient supplementation,
vaccination, cord cleansing with a specific disinfectant, kangaroo mother
care, breast feeding counseling, antimalarial treatment etc were excluded.
Participants: Neonates (first 28 days of
life, or the first month of life where not specified in days) born in
resource limited settings.
Interventions: Interventions during
pregnancy could include any one or more of the following: (i)
Promotion of antenatal care; (ii) Health education and/or
counseling regarding desirable practices during pregnancy; or (iii)
Promotion of delivery in a hospital or at home by a skilled birth
attendant; or (iv) Education about safe and/or clean delivery
practices.
Interventions during childbirth could include
implementation of safe delivery practices in case of domiciliary
deliveries and care of the newborn immediately after birth, including
keeping the baby warm, neonatal resuscitation (if required), and early
initiation of breastfeeding.
Interventions during neonatal period could include any
of the following: (i) Promotion of optimal neonatal care practices
such as exclusive breastfeeding, keeping the baby warm and hygienic cord
care; (ii) Education to improve care-giver recognition of
life-threatening neonatal problems and health care seeking behaviors for
them; (iii) Identification of signs of severe neonatal illness by
community health workers and referral to a health facility; or (iv)
Home-based management of neonatal morbidities.
The term ‘community health worker’ included any village
or community based health worker or volunteer, or an auxiliary health
professional working in the community.
Primary outcomes measure: Neonatal
mortality rate.
Search Methods for Identification of Trials
We searched computerized bibliographic medical
databases, including Medline, Cochrane Controlled Trials Register in the
Cochrane Library, EMBASE, HealthSTAR (Health Services Technology,
Administration, and Research), CINAHL, WHO Afrolibrary and clinical trials
websites till March 5, 2011. For PubMed the following search strategy was
used: (newborn OR neonat* OR perinatal OR baby OR babies) AND ("community"
OR home OR domiciliary OR traditional OR village) AND (mortality OR death
OR survival OR birth outcome OR pregnancy outcome).
A lateral search using the reference lists of
identified articles and ‘related articles’ link in PubMed was done. Hand
searching of reviews and related articles along with conference
proceedings/abstracts was also undertaken. Experts in the field were
contacted for ongoing/recently concluded trials and additional data
wherever required. The research questions and search methodology has been
further elucidated in an earlier publication [7].
Data Analysis
Since the studies were expected to be a combination of
individual and cluster randomized controlled trials, the data entry was
done using the inverse variance method in Stata® software version 9.2 (StataCorp
LP, College Station, USA). The presence of bias in the extracted data was
evaluated by visualization of the funnel plot and also with the "metabias"
command. The summary effect size was calculated using the "metan" command.
The effect size of the intervention (summary RR) was calculated by
comparing NMR at the end of each intervention as the baseline and/or
change data were not available for all included trials. We utilized both
random effects and fixed effects model estimates; however, a random
effects model was preferred as substantial heterogeneity was present (I 2 > 50%).
The following pre-specified subgroup analyses were
performed for all-cause neonatal mortality: (i) preventive
interventions vs. preventive and curative interventions (e.g.
antibiotics for neonatal sepsis) to examine the potential effect of adding
curative treatment; (ii) high (>50 deaths per 1000 live births)
versus low ( Ł50
deaths per 1000 live births) baseline neonatal mortality to examine the
possibility of a greater benefit in populations with higher baseline
mortality.
Subgroup analyses can be done only for categorical
variables (hence the need to convert baseline neonatal mortality to a
categorical variable as done above) and that too one variable at a time.
Multivariate meta-regression was performed to study the simultaneous
effect of both categorical and continuous variables: (i)
asphyxia/sepsis treatment; (ii) baseline NMR; and (iii)
program coverage as explanatory variables; and ‘relative risk of
neonatal mortality’ as the outcome variable.
Results
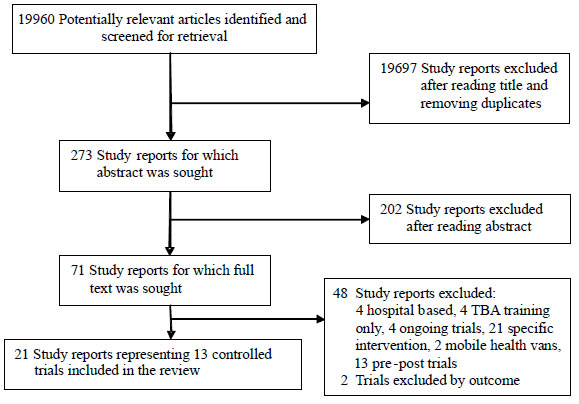
We identified 273 potentially eligible study reports,
202 of which were excluded after reading the abstract. Of the remaining
71, 48 study reports were excluded after reading the full text for reasons
detailed in Fig 1. Two trials were further excluded because
they did not report the outcome of interest. The remaining 21 study
reports (reporting 13 studies) were included in this review [8-28].
 |
|
Fig. 1 Trial flow.
|
Trial characteristics
There were 13 controlled trials [8-28] including 9
cluster randomized trials, 1 quasi randomized trial and 3 non randomized
trials. The controlled trials were primarily from south-southeast Asia (11
trials) and 1 each from Gambia and Greece. The controlled trials involved
populations ranging from 45000 to 1300000 with a baseline NMR from
24.8-57.7 per 1000 live births. The trial characteristics of the included
studies are further detailed in Web Table I.
Intervention package (Web Tables II-III)
The interventions in controlled trials were primarily
of 2 types. Majority of studies involved home visitation by community
health workers with or without community mobilization (9 studies)
[8-22,26,28]. Three studies involved participatory learning and action
cycle by the use of women groups [24-26] and in one study, the
intervention was delivered through trained birth attendants [27]. In
almost all trials the community health worker (CHW) was drawn from the
local community. Majority of studies provided limited data on the level of
education, remuneration and supervision of CHWs. The training of CHWs
varied between 3 days to 36 days and was a combination of both theoretical
as well as practical aspects (Web Table III). Community
mobilization was done in most of the controlled trials but the studies
differed in the quantum and quality of mobilization. The duration of
intervention varied between 14 to 84 months. The interventions were
heterogeneous with respect to content and delivery; and involved some
combination of education about birth and newborn care preparedness,
referrals of high-risk pregnancies, provision of antenatal care, iron/folate
supplementation, nutritional counseling, clean delivery practices,
presence of skilled birth attendants, CHW/TBA training, postnatal visits,
promotion of breastfeeding, neonatal case management, newborn
resuscitation, prevention and management of hypothermia, and referral of
sick newborn (Table I). The number of postnatal home visits
varied between 1 to 5 in all trials (except Bang 2005 which involved ~10
visits) [14-22]. Strategies differed in personnel and content. Bhutta 2008
[10] included referral, as did Darmstadt 2010 [12] and Baqui 2008 [13]
which also included curative care. Strategies were implemented by
different cadres of workers. In Kumar 2008 [11], the strategy involved
community health workers remunerated by the program and local volunteers;
in Baqui 2008 [13], the strategy involved NGO community health workers and
mobilisers; and Bhutta 2008 [10] involved government Lady Health Workers,
TBAs, and community volunteers.
Table I
Components of Community Based Interventions in Included Studies
|
Study |
Community |
Home |
Home |
|
|
mobilization |
visitation |
based neonatal |
|
|
|
|
care and treatment |
| Azad 2010 |
Y |
|
|
| Bang 1999 |
Y |
Y |
Y |
| Baqui 2008 |
Y |
Y |
|
| Baqui 2009 |
Y |
Y |
Y |
| Bhutta 2008 |
Y |
Y |
Y |
| Darmstadt 2010 |
Y |
Y |
|
| Bhutta 2010 |
Y |
Y |
Y |
| Greenwood 1990 |
Y |
|
|
| Jokhio 2005 |
Y |
|
|
| Kafatos 1991 |
Y |
|
|
| Kumar 2008 |
Y |
Y |
|
| Manandhar 2004 |
Y |
|
|
| Tripathy 2010 |
Y |
|
|
Quantitative data synthesis
A funnel plot suggested possible publication bias;
however statistical tests did not confirm this (Begg-Mazumdar: Kendall’s
tau = -0.179487; P=0.37 and Egger: bias =-1.366229 (95%
CI-3.980767-1.248308), P=0.27). Due to the presence of significant
heterogeneity, ‘Random effects’ model has been used throughout this review
for reporting of effect estimates. The risk of bias in included studies is
depicted in Web Table IV. Out of 13 controlled trials
included in the review, 9 had adequate sequence generation
(randomization). Allocation concealment was not an issue in these trials
as these were all cluster randomized trials in which all clusters are
randomized at once. Blinding of the participants was impossible due to the
nature of the intervention; however, 4 trials included blinding of
personnel assessing the effect of intervention. Incomplete outcome data
was present in 2 trials and was deemed "unclear’ in 5 more studies. The
studies were usually free of selective reporting with 2 having an
‘unclear’ status. There was significant heterogeneity among the pooled
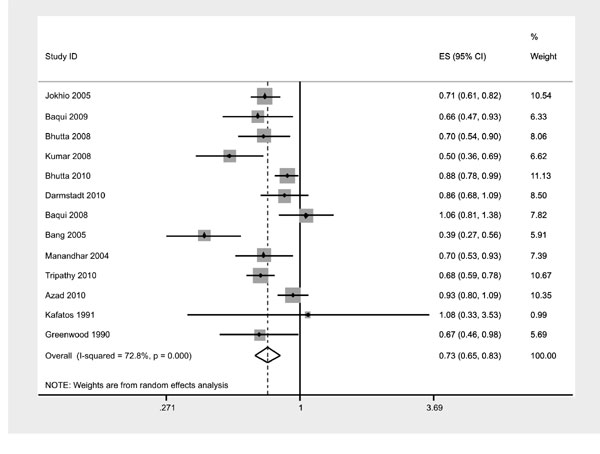
studies (I˛=72.8%). However the estimates from these controlled community
intervention trials pooled together revealed a significant decrease in
neonatal mortality [RR 0.73 (0.65-0.83); P<0.0001] (Fig.
2). In view of the heterogeneity amongst studies, the effect of
baseline NMR and program coverage on neonatal mortality were analyzed.
 |
|
Fig.2 Effect estimate for all trials. |
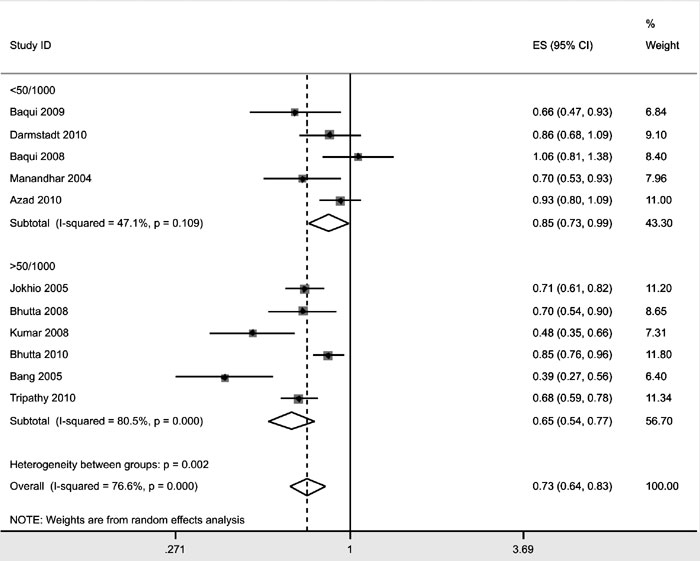
Effect of baseline NMR: To assess the effect of
baseline NMR, subgroup analysis was performed stratifying studies with
baseline NMR less than or greater than 50. In trials with a baseline NMR
less than 50/1000 live births, relative risk of neonatal mortality was
0.85 (0.73-0.99); while in trials with a baseline NMR of more than 50/1000
live births, RR was 0.65 (0.54-0.77) (Fig.3).
 |
|
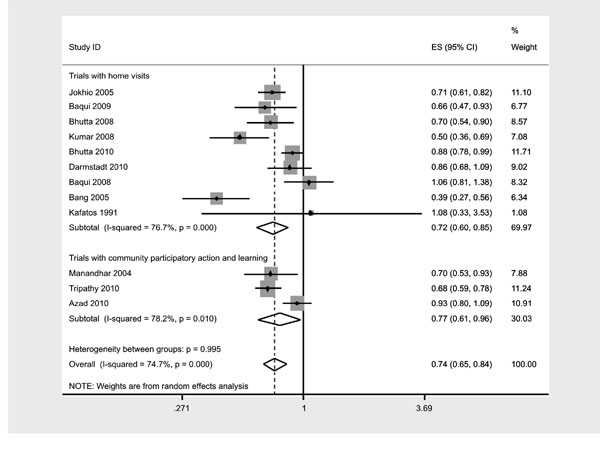
Fig. 3 Subgroup analysis according to the
type of inter-vention. |
Effect of program coverage: Program coverage could
be an explanatory variable explaining the heterogeneity between trials (Web
Table V). The trial with the lowest program coverage [13] reported
the least effect on NMR, while that with the highest program coverage
[14-22] reported the most reduction in NMR. Program coverage was observed
to be an independent determinant of neonatal mortality even when adjusted
for type of intervention and baseline NMR (vide infra).
 |
|
Fig.4 Subgroup analysis by provision of
asphyxia/sepsis treatment in trials with home visits. |
Type of intervention: Subgroup analysis by the type
of intervention i.e. home visits with/without community mobilization (RR
0.71 (0.60-0.84)), vs community participatory action and learning
(RR 0.77 (0.61-0.96)) indicate that both intervention strategies resulted
in similar relative risk for reduction of neonatal mortality (Fig.
4). Differences in baseline NMR, population coverage, ratio of health
worker to beneficiary and duration of the intervention could be potential
explanatory variables that could mask the lack of difference between the
two types of intervention strategy. However, no differences in effect
estimate of NMR were noted between the two types of interventional
strategies after controlling for baseline NMR by metaregression (Table
II). The population covered ranged from 45,000-1,300,000; the ratio of
health worker to population ranged from almost 1: 500 up to 1:4000; and
the duration of intervention ranged between 14-84 months. There was no
consistent effect of these variables to neonatal mortality rate; except
that in trials involving only community participation the reduction in
neonatal mortality was greater when the ratio of health worker to
population improved.
Table II
Effect of Asphyxia and Sepsis Treatment, Baseline Nmr and Programme Coverage
on Neonatal Mortality (Log Relative Risk)
|
Variables |
exp(b) |
Std. Error |
t |
P>|t| |
95% CI |
|
Asphyxia/sepsis treatment |
0.91 |
0.112 |
-0.79 |
0.489 |
0.61-1.34 |
|
Baseline NMR |
0.98 |
0.006 |
-2.98 |
0.058 |
0.96-1.00 |
|
Programme coverage |
0.99 |
0.002 |
-5.25 |
0.013 |
0.98-0.99 |
Meta-regression Number of
studies
= 7
Fit of model without heterogeneity (tau2=0): Q (3 df)
= .175762
Prob > Q = 0.981
Proportion of variation due to heterogeneity I-squared
= 0.000
REML estimate of between-study variance: tau2
= 0.0000 |
Effect of number of home visits:
Web Table
VI provides a comparison of the number of home visits and NMR in
trials involving home visitation. While the trial by Bang, et al.
with the most number of home visits [14-22] documented the largest
reduction in NMR, the trial by Baqui, et al. with the least number
of visits reported the least effect on NMR. However in the remaining
trials wherein the number of home visits were intermediate to these two
trials, the effect on NMR was inconsistent with the number of home visits.
 |
|
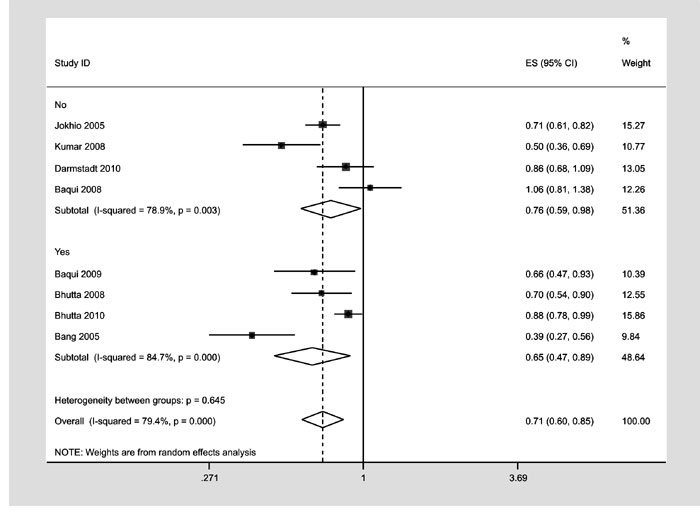
Fig.5 Subgroup analysis according to
Baseline NMR. |
Effect of asphyxia/sepsis management: Analysis of
trials of home visitation with and without asphyxia/sepsis management
indicate that the addition of asphyxia/sepsis management in the
intervention package resulted in a lower relative risk for neonatal
mortality (RR 0.65 (0.47-0.89)) compared to those which did not include
them ((RR 0.76 (0.59-0.98)) (Fig.5). On metaregression,
controlling for type of intervention (home visitation without and with
management of asphyxia and/or sepsis), baseline NMR, and program coverage;
it was observed that program coverage had a significant impact on
mortality reduction (P=0.013), baseline NMR had some impact (P=0.058)
and interventions including asphyxia/sepsis management had no independent
influence on mortality risk reduction (Table II).
Effect of timing of first postnatal visit: The
effect of timing of postnatal home visitation was provided by a single
trial [9]. Among infants who survived the first day of life, neonatal
mortality was 67% lower in those who received a visit on day one than in
those who received no visit (adjusted hazard ratio 0.33, 95% CI
0.23-0.46). For those infants who survived the first two days of life,
receiving the first home visit on the second day was associated with a 64%
lower neonatal mortality than in those who did not receive a visit
(adjusted hazard ratio 0.36, 0.23-0.55). First home visit on any day after
the second day of life was associated with a non-significant reduction in
neonatal mortality.
Discussion
This review involving 13 controlled trials indicates
that community based neonatal care interventions by community health
workers is associated with reduced neonatal mortality in resource-limited
settings, when conducted along with community mobilization activities.
Baseline NMR and program coverage appear to influence the effect size of
mortality reduction that could be achieved with these interventions – high
baseline NMR and program coverage being associated with greater reduction
in neonatal mortality. While it appears logical that trials with more
number of home visits should result in greater mortality reduction, this
association was not consistently observed across all trials. Some studies
suggest that home visits during the first 2 days of life are likely to
yield the largest dividends. While addition of asphyxia and/or sepsis
management does result in greater mortality reduction, the effect appears
to have been confounded by high baseline NMR and program coverage.
The effect of community neonatal interventions appears
to decline as baseline NMR decreases and as NMR gets to below 50,
community interventions possibly need to be supported by facility based
interventions to impact further mortality decline. Program coverage
appears to significantly influence the observed effect size. Since Baqui
2008 [13] involved community mobilization and home visitation implemented
at scale using existing government infrastructure through an integrated
nutrition and health program in eight states of India; it suggests that
this approach would be successful only if there is high coverage. The
effect is also dependent on the ratio of health worker to population.
Azad’s trial which had 1 community worker per 1414 population [23]
documented less reduction in NMR compared to trials with a better ratio
[24,25]. This suggests that population coverage and the proportion of
newly pregnant women enrolled in groups might need threshold levels to
have an effect on birth outcomes (perhaps of the order of one group per
450-750 population, and between 30% and 50% of newly pregnant women
attending groups, respectively) [23]. The enrolment of newly pregnant
women is likely to be a key determinant of the effectiveness of
interventions involving women’s groups. It is important to understand that
as the NMR decreases in an area, the cause specific mortality due to
sepsis decreases, asphyxia probably remains unchanged, and proportion of
mortality due to preterm birth (as well as absolute number) increases.
Whether addition of sepsis treatment with oral or injectable antibiotics
can decreases the cause specific mortality further is not clear. Besides,
there are legal and ethical issues of allowing these health workers to
treat newborns with antibiotics which must be resolved before this
component of the home based intervention can be taken to scale. The issue
of whether mortality due to asphyxia can be decreased by providing
training and equipment to a community health worker has produced equivocal
results [14-22, 29]. Since CHWs are likely to encounter asphyxia
sporadically; continued training for maintenance of skills to manage
asphyxia may be a challenging task.
Overall completeness and applicability of evidence
The studies were conducted in participants and settings
directly relevant to the review. A total of 13 controlled trials involving
about 192000 births were included in this systematic review; the
identified studies thus sufficiently addressed the main question of the
review. Most of the reviewed studies did not report the complete
description and characteristics of intervention as well as the training,
supervision, remuneration and motivation of CHWs. This information would
be of great importance in under-standing if and how these factors affect
the performance of CHWs in operational settings. The heterogeneity and
paucity of studies prevented assessment of each component of the
intervention package (health education, community mobilization, home
visits, curative care etc) and its corresponding effect on neonatal
mortality. The review did not include assessment of effect of community
based neonatal care on early or late neonatal mortality and cause specific
neonatal mortality rates. With a sudden increase in number of
institutional deliveries due to Janani Surakha Yojana, it would be
worth-while to assess the need to modify the community based neonatal care
interventions to maximize the gains in neonatal survival.
Quality of the evidence
Assessment of risk of bias in included studies suggests
adequate sequence generation in majority of studies. Allocation
concealment is usually not an issue in cluster randomized intervention
trials as all the clusters are randomized at once. Given the type of
intervention, trials cannot possibly involve blinding of the participants.
Similarly, with mortality as the primary outcome, blinding of outcome
assessors is desirable but its absence cannot downgrade the strength of
evidence. The risk of bias in the included trials is largely from an
inability to address incomplete outcome data. The included studies are
largely free of selective reporting.
Potential biases in the review process
The main conclusion regarding neonatal mortality
remained stable over the spectrum of pre-specified subgroup analyses.
Analysis of 13 trials did not indicate evidence of publication bias.
Cluster and individually randomized trials were appropriately combined by
using generic inverse variance method of data entry, thus allowing the
pooling of effects of cluster randomized trials and other controlled
trials. Diligent efforts were made to include all relevant trials. The
issue of significant heterogeneity among the trials was addressed by doing
subgroup analysis and metaregression using pre-specified variables.
However, due to the small number of trials for meta-regression analysis,
the statistical power was limited.
Conclusions
Community newborn care through home visitation
with/without community mobilization and community participatory action and
learning interventions decrease NMR, but their impact appears to be
highest when baseline NMR are high and program coverage is high (>50%).
When community participatory action and learning approach is the key
intervention, population covered and the proportion of newly pregnant
women enrolled in community groups appears to require threshold levels to
have an effect on birth outcomes. Social mobilization should probably be
an integral component of any community neonatal health intervention as it
is likely to have a more sustaining effect on outcomes. The addition of
asphyxia treatment and antibiotics for management of sepsis as components
of the intervention package may not necessarily result in large
augmentation in neonatal mortality decline, besides it would also require
legal and ethical issues of treatment by CHW to be resolved. It also
appears that when taken to scale, impact of community based newborn care
interventions is lower than when implemented at smaller scale. The
decrease in effectiveness is possibly due to difficulties in ensuring
adequate coverage, supervision and quality of care when interventions are
scaled up. In India, community based newborn care is recognized as an
important strategy for child health. Frontline health workers, ASHAs
(accredited social health activists) and AWWs (anganwadi workers)
are being trained and mandated to visit newborns at their households to
provide newborn care under the Integrated Management of Newborn and
Childhood Illnesses (IMNCI) strategy and ASHA training programs. The
evidence presented here further validates the investments made by India on
community based newborn care and provide additional insights and evidence
to strengthen the implementation, and make a decisive impact on neonatal
mortality. Firstly, the fact that high program coverage is essential to
make a significant impact on neonatal mortality makes a strong case for
monitoring the coverage and identifying ways to reach out to larger
numbers of newborns. Secondly, the fact that the first home visitation has
the most significant impact on neonatal mortality when conducted within
first two days of birth highlights the importance of reaching the newborns
early. This would be especially challenging among home deliveries, which
still constitute more than a quarter of all births. Thirdly, the fact that
community participatory action and learning through community based
facilitators also have a significant and sustained impact on neonatal
mortality indicates possibilities of engaging strong cohesive women’s
groups in settings where such groups exist.
Knowledge gaps
However, there are still gaps with regards to issues
related to scale up of community newborn health interventions and the
magnitude of their impact on neonatal survival. The areas include optimal
training, supervision, remuneration and accountability of community health
workers; optimal size of population to be covered by the CHW, timing and
number of home visits that are achievable within the system constraints
and integrating maternal and newborn survival interventions in unified
package for CHW.
Lastly, the fact that in most scaled up interventions,
the impact was lower than in small scale studies highlight the need for
ensuring the elements that tend to get neglected when scaling up: quality
of training, presence of supportive supervision and motivation of the
frontline workers. With an adequate emphasis on the above factors,
Community based Newborn Care has a potential to make India inch closer to
achieving MDG-4.
Contributors: The contributions of all authors are
described in detail in a previous publication [7].
Conflict of interest: PM is a staff member of
UNICEF that supports community based neonatal care. All other authors:
None stated.
Funding: UNICEF.
Disclaimer: The views expressed in the paper
are the authors’ own and do not necessarily reflect the decisions or
stated policies of the institutions/organizations they work in/with.
References
1. WHO Country Cooperation
Strategy 2006-2011. http://www.searo.who.int/LinkFiles/WHO_Country_
Cooperation_ Strategy_-_ India_ Health_Development_ Challenges.pdf.
Accessed on May 1, 2011.
2. SRS Bulletin January 2011. http://www.censusindia.gov.
in. Accessed on May 14, 2011.
3. The Million Death Study Collaborators. Causes of
neonatal and child mortality in India: a nationally representative
mortality survey. Lancet 2010:376;1853-60.
4. National_Fact_Sheet_CES_2009. UNICEF. http://www.unicef.org/india/National_Fact_Sheet_CES_
2009.pdf. Accessed on May 1, 2011.
5. Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker
N, de Bernis L. Evidence-based, cost-effective interventions: how many
newborn babies can we save? Lancet. 2005;365:977-88.
6. Gogia S, Sachdev HS. Home visits by community health
workers to prevent neonatal deaths in developing countries: a systematic
review. Bull World Health Organ. 2010;88:658-66.
7. Mathew JL, Shah D, Gera T, Gogia S, Mohan P, Panda
R, et al. UNICEF-PHFI Series on Newborn and Child Health, India:
Methodology for Systematic Reviews on Child Health Priorities for Advocacy
and Action. Indian Pediatr. 2011;48:183-9.
8. Jokhio AH, Winter HR, Cheng KK. An intervention
involving traditional birth attendants and perinatal and maternal
mortality in Pakistan. N Engl J Med. 2005; 352:2091-9.
9. Baqui AH, El-Arifeen S, Darmstadt GL, Ahmed S,
Williams EK, Seraji HR, et al. Effect of community-based
newborn-care intervention package implemented through two service-delivery
strategies in Sylhet district, Bangladesh: a cluster-randomised controlled
trial. Lancet. 2008;371:1936-44.
10. Bhutta ZA, Memon ZA, Sooi S, Salat MS, Cousens S,
Martines J. Implementing community-based perinatal care: results from a
pilot study in rural Pakistan. Bull World Health Organ. 2008;86:452–9.
11. Kumar V, Mohanty S, Kumar A, Misra RP, Santosham M,
Awasthi S, et al. Effect of community-based behaviour change
management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a
cluster-randomised controlled trial. Lancet. 2008;372:1151-62.
12. Darmstadt GL, Choi Y, Arifeen SE, Bari S, Rahman
SM, et al. Evaluation of a cluster-randomized controlled trial of a
package of community-based maternal and newborn interventions in Mirzapur,
Bangladesh. 2010 PLoS ONE 5(3):e9696. doi:10.1371/journal.pone.0009696.
13. Baqui AH, Williams EK, Rosecrans AM, Agrawal PK,
Ahmed S, Darmstadt GL, et al. Impact of an integrated nutrition and health
program on neonatal mortality in rural northern India. Bull WHO.
2008;86:796-804.
14. Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmukh
MD. Effect of home-based neonatal care and management of sepsis on
neonatal mortality: field trial in rural India. Lancet. 1999;354:1955-61.
15. Bang AT, Reddy HM, Deshmukh MD, Baitule SB, Bang
RA. Neonatal and infant mortality in the ten years (1993 to 2003) of the
Gadchiroli field trial: effect of home-based neonatal care. J Perinatol
2005;25(Suppl 1):S92-107.
16. Bang AT, Bang RA, Baitule SB, Reddy HM, Deshmukh
MD. Management of birth asphyxia in home deliveries in rural Gadchiroli:
the effect of two types of birth attendants and of resuscitating with
mouth-to-mouth, tube-mask or bag-mask. J Perinatol. 2005;25(Suppl
1):S82-91.
17. Bang AT, Baitule SB, Reddy HM, Deshmukh MD, Bang
RA. Low birth weight and preterm neonates: can they be managed at home by
mother and a trained village health worker? J Perinatol. 2005;25(Suppl
1):S72-81.
18. Bang AT, Bang RA, Stoll BJ, Baitule SB, Reddy HM,
Deshmukh MD. Is home-based diagnosis and treatment of neonatal sepsis
feasible and effective? Seven years of intervention in the Gadchiroli
field trial (1996 to 2003). J Perinatol. 2005; 25(Suppl 1):S62-71.
19. Bang AT, Bang RA, Reddy HM, Deshmukh MD, Baitule
SB. Reduced incidence of neonatal morbidities: effect of home-based
neonatal care in rural Gadchiroli, India. J Perinatol. 2005;25(Suppl
1):S51-61.
20. Bang AT, Bang RA. Background of the field trial of
home-based neonatal care in Gadchiroli, India. J Perinatol. 2005;25(Suppl
1):S3-10.
21. Bang AT, Bang RA, Reddy HM, Deshmukh MD. Methods
and the baseline situation in the field trial of home-based neonatal care
in Gadchiroli, India. J Perinatol. 2005; 25(Suppl 1):S11-7.
22. Bang AT, Bang RA, Reddy HM. Home-based neonatal
care: summary and applications of the field trial in rural Gadchiroli,
India (1993 to 2003). J Perinatol 2005;25 (Suppl 1):S108-22.
23. Azad K, Barnett S, Banerjee B, Shaha S, Khan K,
Rego AR, et al. Effect of scaling up women’s groups on birth
outcomes in three rural districts in Bangladesh: a cluster-randomised
controlled trial. Published Online March 8, 2010;
doi:10.1016/S0140-6736(10)60142-0.
24. Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi
J, Rath S, et al. Effect of a participatory intervention with
women’s groups on birth outcomes and maternal depression in Jharkhand and
Orissa, India: a cluster-randomised controlled trial. Published online
March 8, 2010; doi: 10.1016/S0140-6736(09)62042-0.
25. Manandhar DS, Osrin D, Shrestha BP, Mesko N,
Morrison J, Tumbahangphe KM, et al. Effect of a participatory
intervention with women’s groups on birth outcomes in Nepal: cluster-randomised
controlled trial. Lancet. 2004;364:970-9.
26. Bhutta ZA, Soofi S, Cousens S, Mohammad S, Memon ZA,
Ali I, et al. Improvement of perinatal and newborn care in rural
Pakistan through community-based strategies: a cluster-randomised
effectiveness trial. Lancet. 2011;377:403-12
27. Greenwood A, Bradley A, Byass P. Evaluation of a
primary health care program in The Gambia. I. The impact of trained
traditional birth attendants on the outcome of pregnancy. J Trop Med Hyg.
1990;93:58-66.
28. Kafatos AG, Teltoura S, Pantelakis SN, Doxiadis SA.
Maternal and infant health education in a rural Greek community. Hygiene.
1991;10:32-7.
29. Carlo WA, Goudar SS, Jehan I, Chomba E, Tshefu A, Garces A, et
al, and the First Breath Study Group. Newborn-Care Training and
Perinatal Mortality in Developing Countries. N Engl J Med.
2010;362:614-23.
|
|
|
 |
|

