|
|
|
Indian Pediatr 2009;46: 625-627 |
 |
Letrozole as a Booster Therapy in Growth
Hormone Deficiency |
|
KVS Hari Kumar, Muthukrishnan Jayaraman, Abhyuday Verma* and Kirtikumar D
Modi
From the Departments of Endocrinology and Pediatric
Endocrinology*, Medwin Hospitals, Nampally, Hyderabad, AP, India.
Correspondence to: Dr Hari KVS Kumar, Department of
Endocrinology, Medwin Hospitals, Chirag Ali Lane, Nampally, Hyderabad 500
001, AP, India.
Email: hariendo@rediffmail.com
Manuscript received: April 1, 2008;
Initial review: April 23, 2008;
Accepted: July 4, 2008.
|
|
Abstract
A 13 year old boy presented to us with short stature.
Evaluation revealed growth hormone (GH) deficiency. He was treated with
GH replacement for 10 months and to further boost up the growth
potential, an aromatase inhibitor Letrozole was added to GH therapy.
After one year of combination therapy, patient had significant
improvement in predicted adult height without a negative impact on
pubertal progression.
Key Words: Aromatase inhibitors, Estrogen, Growth hormone,
Letrozole.
|
|
E
strogen is an essential regulator
of bone maturation, growth plate fusion, and cessation of longitudinal
growth(1). Therefore, an increase in adult height may be achieved in short
children by blocking estrogen biosynthesis. Aromatase is the key enzyme
for estrogen biosynthesis and aromatase inhibitors (AI) have been used
primarily in women with breast carcinoma. The use of aromatase inhibitors
may provide a means to delay skeletal maturation and increase final height
in children with short stature(2).
Use of aromatase inhibitors to improve the final height
has been extensively reported in idiopathic short stature or
constitutional delay in puberty(3). However, the addition of aromatase
inhibitor therapy to growth hormone (GH) in patients of GH deficiency is
not widely studied(4). This combination may augment the growth potential
and final height achieved in cases of GH deficiency. We report the pattern
of growth in a child after addition of letrozole to GH therapy in a case
of idiopathic growth harmone deficiency.
Case Report
A male child was first seen for evaluation of short
stature at the age of 13 years 8 months. He was a product of
nonconsanguineous marriage with a birthweight of 3.2 kg, delivered after
full term. He was treated for pulmonary tuberculosis at the age of 1 yr.
His motor, mental milestones and scholastic performance in the school were
normal. He was always amongst short children in the class but never sought
any medical consultation. Parents denied noticing development of secondary
sexual characteristics. There were no siblings and parents denied family
history of delayed puberty. Anthropometry revealed: height – 140 cm (<5th
centile), weight 48 kg (75th centile), upper/lower segment ratio 0.9, arm
span – 142 cm, and puberty (Tanners grading) Stage 1 with prepubertal
testes and bilateral lipomastia. His mid-parental height (MPH) was 173.5
cm. Examination revealed no midline defects, goiter or evidence of
systemic disease. Estimated bone age was 11 yr by Greulich-Pyle method and
his initial hematological and biochemical evaluation including
thyroid/renal/ hepatic tests were normal. He was observed for 6 months and
due to poor growth velocity (2 cm increase in 6 months) he was tested for
GH deficiency after adequate priming. The peak GH levels following
stimulation with clonidine was 0.26 ng/mL and GH deficiency was confirmed
by low IGF1 - 50.3 ng/mL (131-718) and IGFBP3 – 809.7 ng/mL (1700-6940).
His LH – 0.4 IU/L, FSH – 0.8 IU/L and testosterone – 120 ng/dL were
prepubertal. He was initiated on GH therapy at the age of 14 yrs with a
dose of 0.3 mg/kg/week. After 10 months of GH therapy, in view of height
centile below his target height centile, the use of additional therapy to
augment growth was planned and Letrozole was started at a dose of 2.5 mg
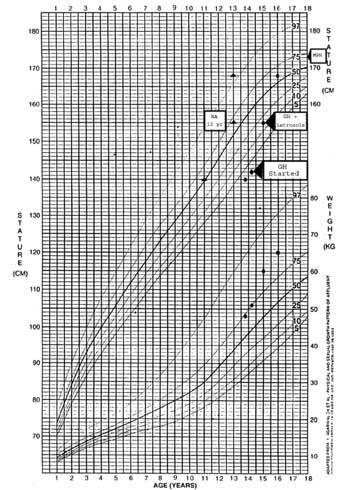
daily along with GH therapy. The height improvement is shown in growth
chart (Fig. 1) and other clinical details are given in
Table I. Due to significant improvement in stature without bone
age advancement, we discontinued both GH and Letrozole after 1 year. The
height velocity after therapy is about 13.5 cm per year over past 2 years
with use of GH and Letrozole. The liver function tests and glycemic levels
were normal throughout the period of observation. However, we did not
evaluate any markers of bone turnover during the entire period of
observation.
 |
|
Fig.1 Growth chart of the patient. |
TABLE I
Clinical Details of Patient Before and After Therapy with GH and Letrozole
|
Parameter |
Pre treatment |
On GH treatment alone |
On
GH + Letrozole therapy |
| Duration
of Observation |
6 months |
10 months |
12
months |
| Height
gain (cm) |
2 |
13 |
13 |
| Height
centile |
< 5th centile |
15th centile |
65th
centile |
| Growth
velocity (cm/yr) |
4 |
14 |
13 |
| Bone age
|
11 yrs |
11 to 13 yrs |
Static |
| Predicted
adult height* (cm) |
170 |
174 |
181 |
| Pubertal
status |
Tanner stage 1 |
Tanner stage 3 |
Tanner
stage 4 |
|
* As
per Bailey & Pinneau charts. |
Discussion
Our case demonstrates the beneficial effect of
letrozole along with GH therapy in augmenting the final adult height in a
case of GH deficiency. The predicted adult height improved significantly
while pubertal maturation proceeded unimpeded. Growth charts account for
spontaneous pubertal progression and our patient demonstrated growth
velocity of 13.5 cm per year, higher than seen with onset of spontaneous
puberty in GH deficient indivi-duals(5,6).
Growth response to therapy with GH is dependent on
various factors(6). The available options to augment the growth response
and final adult height are simultaneous use of gonadotropin-releasing
hormone analogs (GnRHa) or aromatase inhibitors. The GnRHa therapy is
associated with significant detrimental effects on metabolism and bone
mineral density(7). These effects make the use of these analogs unsuitable
for long term use. Thus, the use of AI offers the advantage of continued
virilization and maintenance of pubertal body composition in boys while
potentially delaying skeletal maturation. Our patient had a height
increment of 13 cm during 10 months of GH therapy and combination therapy
of GH and letrozole resulted in height increment of 13 cm in 12 months.
This suggests that letrozole improves the final height in GH deficiency
and augments the response to GH therapy as demonstrated by earlier
observations(4).
Letrozole was well tolerated by our patient. Potential
adverse effects of aromatase inhibitors are decreased bone matrix
accumulation and delayed pubertal progression. However, we did not
estimate bone mineral density in the child because of letrozole use for
one year only and lack of standardization of dual energy X-ray
absorptiometry scan in pediatric age group(8).
Contributors: KVS, JM, AV worked up the patient
clinically. KVS, JM reviewed the literature and drafted the manuscript
initially. KVS, KDM co drafted and revised the manuscript. KDM will act as
the guarantor and the final manuscript was approved by all authors.
Funding: None.
Competing interests: None stated.
References
1. Grumbach M, Auchus RJ. Estrogen: consequences and
implications of human mutations in synthesis and action. J Clin Endocrinol
Metab 1999; 84: 4677-4694.
2. Cernich J, Jacobson JD, Moore WV, Popovic J. Use of
aromatase inhibitors in children with short stature. Pediatr Endocrinol
2004; 2: 2-7.
3. Hero M, Wickman S, Dunkel L. Treatment with the
aromatase inhibitor letrozole during adolescence increases near-final
height in boys with constitutional delay of puberty. Clin Endocrinol 2006;
64: 510-513.
4. Zhou P, Shah B, Prasad K, David R. Letrozole
significantly improves growth potential in a pubertal boy with growth
hormone deficiency. Pediatrics 2005; 115: e245-248.
5. Grumbach MM. Estrogen, bone, growth and sex: a sea
change in conventional wisdom. J Pediatr Endocrinol Metab 2000; 13 [Suppl
6]: 1439-1455.
6. Wit JM, Kamp GA, Rikken B. Spontaneous growth and
response to growth hormone treatment in children with growth hormone
deficiency and idiopathic short stature. Pediatr Res 1996; 39: 295-302.
7. Yanovski JA, Rose SR, Municchi G, Pescovitz OH, Hill
SC, Cassorla FG, et al. Treatment with a luteinizing
hormone-releasing hormone agonist in adolescents with short stature. N
Engl J Med 2003; 348: 908-917.
8. Binkovitz LA , Henwood MJ. Pediatric DXA: technique and
interpretation. Pediatr Radiol 2007; 37: 21-31.
|
|
|
 |
|

