Children with a solitary hydronephrotic kidney are
uncommon. We report a patient with severe hypertension associated with a
normally functioning solitary kidney, which showed features of
hydronephrosis.
Case Report
An 8-year-old boy presented with history of headache
for the past eight days and vomiting, fever and neck stiffness for the
past one day. There was no preceding history of seizures, diaphoresis,
palpitations or blurring of vision. The patient was conscious with
minimal neck stiffness, left hemiparesis and blood pressure of 240/160
mm Hg. Fundus examination showed grade 4 hypertensive changes with
papilledema. The blood counts were normal and differential revealed
lymphocytosis. Blood urea level was 36 mg/dL and creatinine was 0.8 mg/dL.
CSF revealed no pleocytosis, normal proteins and no hypoglychorrachia.
Contrast enhanced computed tomography showed minimal meningeal
enhancement with no exudates and a small infarct in the region of right
external capsule. This infarct was a probable sequale of long standing
hypertension.
Hypertension was treated with a combination of
nifedipine (2 mg/kg/day), propranolol (2 mg/kg/day), clonidine (20
µg/kg/day) and furosemide (2 mg/kg/day). His chest skiagram was normal
and ECG showed evidence of left ventricular hypertrophy. Abdominal
ultrasound showed absent left kidney with mild hydronephrosis of the
right kidney; Doppler study showed no evidence of renal artery stenosis.
An intravenous urogram confirmed adequate function of the right kidney.
Plasma renin estimation (4.8 ng/mL/hr) was within normal limits.
Selective renal angiographic study with estimation of renal vein renin
(4 ng/mL/hr) was essentially normal. A DTPA-renal scan showed normal
renal function on the right side with no function on the left. Diuretic
renography done simultaneously, confirmed the presence of nonobstructive
hydronephrosis. Voiding cystourethrogram done did not show evidence of
vesicouretral reflux.
DMSA scan done subsequently had shown no evidence of
scarring consequent to a preexisting reflux. Twenty four hour urinary
catecholamines and I131 MIBG (metiodo-benzyl guanidine) scintigraphy
were normal. CT of the abdomen failed to demonstrate the contralateral
kidney. Cystoscopy done revealed ureteric orifices on both sides. On
laprotomy a dysplastic atrophic kidney (Fig. 1) was identified on
the left side, which was removed. This however failed to ameliorate the
hypertension. Immunoturbidometric examination of the urine showed micro-albuminuria
(24 mg/g creatinine).
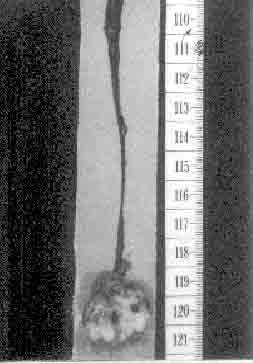 |
| Fig. 1.
Grossly atrophic kidney removed on laprotomy. |
Discussion
Severe hypertension posed a diagnostic dilemma.
Ultrasound, Doppler study plasma renin levels, urinary catecholamines
and MIBG scan ruled out renovascular hyper-tension and pheochromocytoma.
Imaging modalities suggested a solitary functioning right kidney with
agenesis of the left kidney. CT failed to pick up any renal tissue on
the left side. Diuretic renogram ruled out pelvi-uretcric obstruction
causing right hydro-nephrosis. Presumably, volume overload on the
solitary functioning kidney resulted in hydronephrosis. Vesico-ureteric
reflux was ruled out on imaging studies. Therefore, the right kidney did
not have a "surgically treatable" cause of hypertension. This left us
with one important question - was the left kidney really absent or
present but dysplastic? A faint suggestion came up on the angiography
that showed a small beaking from the left side of the aorta at the usual
location of the ostium of the left renal artery. Cystoscopy contributed
by visualizing the left ureteric orifice. This settled the issue of
agenesis verses dysplasia. On surgical exploration the lower part
of the ureter was identified and followed upwards leading to the
dysplastic kidney. Looking at the specimen grossly being just 1.5 cm and
disorganized, it is not surprising that CT and ultrasound could not pick
it up pre-operatively. The dysplastic left kidney was removed because
hypertension, infection, hemorrhage and malignant change are known
complica-tions of renal dysplasia(1). There have been reports of
improvement in hypertension following nephrectomy of the dysplastic
kidney. The chances of complete regression of hypertension after
nephrectomy are low, the possibility of reduction in the doses of
antihypertensive drugs is a definitive goal.
Bachmann has presented case reports wherein blood
pressure normalized after removal of the small kidney and in few where
hypertension persisted(2). He emphasized that nephrectomy of the small
kidney should only be performed, if the integrity of the contralateral
kidney is certain.
Hypertension in patients with solitary kidney have
appeared in literature. Lan, et al. collected data on 14 children
with unilateral renal agenesis defined by cystoscopy of which 21% had
hydronephrosis.They observed that this group had increased prevalence of
hyper-tension, proteinuria and renal insufficiency to the tune of 29%,
43% and 36%, compared to the uninephrectomized group. In their study the
incidence of the congenital solitary kidney (CSK) was 1 in 1,496. They
observed that these complications were common in the age group of 30 to
60 years, unlike our patient who presented in the first decade(3).
The cause of hypertension in a child with solitary
kidney has been extrapolated from animal studies and later confirmed in
humans. Laboratory studies show that a marked reduction (11/12) in renal
mass results in progressive glomerulosclerosis of the residual tissue,
manifested by azotemia, proteinuria and hypertension. Glomerular
destruction appears to be due to augmented trans capillary hydraulic
pressure difference (DP) and glomerular plasma flow, a process of
chronic hyperfilteration that leads to altered charge and size selective
permeability, increased trans capillary protein flux, mesangial
overloading and sclerosis(4). CSK is an experiment of nature, in which
the stimulus exists in fetal life, the remnant kidney being enlarged.
The first suggestion that the solitary kidney might be prone to focal
glomerulosclerosis (FGS) was provided by Kiprov, et al.(5). A
foreunner of FSGS is microalbuminuria. The renal function may however
remain stable for a long time.
It is also important to follow up these children,
prevent protein overloading and retard the development of FGS(6). The
incidence of finding a grossly atrophic kidney in a child is as high as
1 in 1400, therefore it is important that such children are identified
and followed up stringently.
Contributors: Sk and UJ were involved in patient
care, analysis of the case and drafting the manuscript. SKM was the
overall incharge of the patient management. SKA operated upon this
patient and helped in drafting the manuscript. UJ will act as guarantor
for the paper.
Funding: None.
Competing interests: None stated.
