|
|
|
Indian Pediatr 2019;56: 74- 75 |
 |
Influenza Virus Among
Children with Acute Respiratory Infections in Chennai, India
|
|
Anusha Hindupur, Prabu Dhandapani and *Thangam Menon
Department of Microbiology, Dr ALM
Post Graduate, Institute of Basic Medical
Sciences, University of Madras,
Taramani, Chennai, India.
Email: [email protected]
|
Influenza is a major public health concern.
Information on the prevalence of influenza virus in respiratory tract
infections in Indian children is very sparse. In the present study, 267
nasal swabs were collected from children with acute respiratory
infections in Chennai, India, out of which 22 (8.2%) and 6 (2.3%)
samples were positive for influenza A and B virus respectively.
Keywords: Epidemiology, Etiology, Pneumonia.
|
|
I
n developing countries, 30% of all childhood
deaths are attributed to acute respiratory infections (ARIs) [1]. Due to
its ability to cause frequent epidemics and periodic pandemics,
influenza virus has a major public health implications. We enrolled 267
children aged 45 days to 16 years visiting the outpatient department of
various hospitals and presenting with symptoms of ARI such as cough,
fever, sore throat, rhinorrhea, nasal congestion, headache, myalgia,
wheezing and dyspnea between April 2016 and March 2018. Children with
chronic respiratory infections and other co-morbidities were excluded
from the study. The study was approved by the Institutional Human Ethics
Committee. Nasal swabs were collected using sterile flocked nylon swabs,
which were inserted 2-3 cm deep inside the nostril and rotated 2–3
times. They were transported in a viral transport medium (HiMedia,
India) to the laboratory maintaining cold chain. The vials were briefly
vortexed, and RNA was extracted from the swabs using the NucleoSpin RNA
virus kit (Macherey Nagel, Germany) according to manufacturer’s
instructions. The extracted RNA was converted to cDNA using RevertAid
first strand cDNA synthesis kit (Thermo Fisher Scientific, USA), and
stored at –20 ºC.
cDNA was subjected to real time Reverse-transcriptase
Polymerase chain reaction (RT-PCR) for the detection of influenza A and
Victoria and Yamagata lineages of influenza B virus using hybridization
probes according to WHO protocol [2]. Real time RT-PCR was carried out
in StepOnePlus real time PCR system (Applied Biosystems, USA).
Appropriate positive and negative controls were included in each run. Ct
value of £40
cycles was considered to be positive. The association between influenza
positivity and demographic/epidemiological data was determined using
two-tailed chi square test.
The mean (SD) age of the patients was 45.9 (38.5)
months. The most common symptoms observed among the patients with ARI
were cough (83.1%), rhinorrhea (60.3%) and nasal congestion (57.7%). The
influenza A virus was detected in 22 (8.2%) samples, and 6 (2.3%)
samples were positive for influenza B virus, of which three samples
belonged to Victoria lineage and 3 belonged to Yamagata lineage of
influenza B virus. The majority of influenza A virus positive patients
had fever as the major symptom (17, 77.2%) followed by cough (16,
72.7%). Seven patients with influenza A virus had myalgia. Among the
patients positive for influenza B virus (Victoria lineage), fever was
the most common symptom, while cough was the frequent symptom associated
with influenza B virus Yamagata lineage positive patients. The mean (SD)
age of patients positive for influenza A and B virus was 49.9 (35.4)
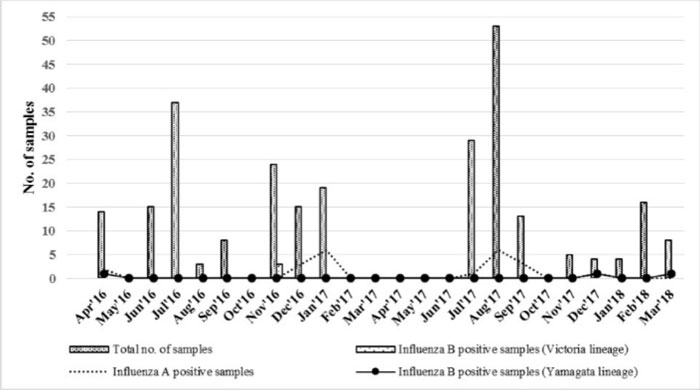
months and 68.2 (37.4) months, respectively. Influenza A showed highest
rates of detection in the months of January and August 2017 (Fig.
1).
 |
|
Fig. 1 Seasonal distribution of acute
respiratory infections and influenza B infection in Chennai,
India.
|
In the present study infection with influenza A virus
was more common when compared with infection with influenza B virus.
Previous studies from the region have shown similar results [3,4]. In an
earlier study carried out in Chennai, 30 out of 240 (12.5%) children
with ARI were positive for influenza viruses [5]. Fever and cough were
the predominant symptoms among positive influenza A and B cases, similar
to previous studies from India [4,6]. Studies on seasonal trends of
respiratory viruses are very useful in predicting etiological agent
during outbreaks. In our study, detection of influenza A virus peaked in
the months of January and August. Studies from other parts of India
reported detection of influenza A during autumn and winter seasons
[7,8].
Limitation of the study was that samples were
collected only from children with ARI, and not influenza-like-illness.
The subtypes of circulating strains of influenza A virus were also not
determined in the study.
The present study suggests influenza virus to be an
important cause of ARI among children in Chennai, India. Large
population-based studies using appropriate molecular methods are
required to determine the prevalence of influenza viruses in children
with ARI from different regions of India so that preventive strategies
could be prioritized.
Contributors: AH: design and
implementation of the study, data analysis and writing of the
manuscript; PD, TM: critical inputs into study design, interpretation of
data and manuscript writing.
Funding: None; Competing Interest: None
stated.
References
1. Hinman AR. Global progress in infectious disease
control. Vaccine. 1998;16:1116-21.
2. World Health Organization. Information for
Molecular Diagnosis of Influenza Virus – Update. Available from:
http://www.who.int/influenza/gisrs_laboratory/molecular_diagnosis_influenza_virus_humans_update_
201403.pdf. Accessed May 22, 2018.
3. Rasul CH, Bakar MA, Mamun AA, Siraz MS, Zaman RU.
Burden and outcome of human influenza in a tertiary care hospital of
Bangladesh. Asian Pac J Trop Med. 2011;4:478-81.
4. Roy S, Patil D, Dahake R, Mukherjee S, Athlekar
SV, Deshmukh RA, et al. Prevalence of influenza virus among the
paediatric population in Mumbai during 2007-2009. Indian J Med Microbiol.
2012;30:155.
5. Priya P, Sheriff AK. Influenza activity among the
paediatric age group in Chennai. Indian J Med Res. 2005;121:776-9.
6. Yeolekar LR, Damle RG, Kamat AN, Khude MR, Simha
V, Pandit AN. Respiratory viruses in acute respiratory tract infections
in Western India. Indian J Pediatr. 2008;75:341.
7. Bharmoria A, Vaish VB, Chaurasia A, Tahlan AK. The
emergence and consistency of influenza strains causing influenza like
illness in Himachal Pradesh, India. Virus Disease. 2016;27:130-5.
8. Panda S, Mohakud NK, Suar M, Kumar S. Etiology, seasonality, and
clinical characteristics of respiratory viruses in children with
respiratory tract infections in Eastern India (Bhubaneswar, Odisha). J
Med Virol. 2017;89:553-8.
|
|
|
 |
|

