Dr. S joined postgraduate residency in Pediatrics
just a few months ago. Soon, the head of the department started
receiving complaints regarding him from staff nurses, fellow residents,
and patient attendants. He was reported to be rude and aggressive while
dealing with children and their parents. He often argued and quarrelled
with staff nurses and other subordinates during the work hours. He used
to ignore the instructions given by his seniors. However, he behaved
extremely well in front of the faculty members; it was difficult for the
faculty to believe that he has a problem!
Medical teachers often face situations where students
or trainees are problematic or challenging. All clinical teachers want
their team members to be competent, compassionate, cooperative and
constructive. Medical Council of India (MCI) describes the role of
Indian medical graduates beyond being a clinician, to be a leader,
professional, communicator, and a lifelong learner who is ethical and
committed to excellence [1,2]. Qualities of a ‘great resident’ or a
‘high performing resident’ include being trustworthy, hardworking,
efficient, and self-directed learner [3]. It is, however, not unusual to
encounter trainees with a deficit in knowledge, lack of clinical
judgment, annoying behavior, inappropriate interaction with colleagues,
or being late or absent. All these serve as significant obstacles in the
attainment of the desired competencies [4-8].
Problem behavior of one resident sometimes spoils the
reputation of the entire department and hampers training of fellow
residents. Such a resident often diverts the time and energy of other
fellow residents and faculty members. Improper handling may result in
violent behavior to self or others. It is thus essential to recognize
the problem resident, and institution of remedial measures at earliest.
Definition
Myriads of terms are used for a problem resident:
troublemaker resident, problem learner, difficult resident, the
burned-out resident, disruptive resident, and so on [6-8]. A ‘problem
learner’ has been defined as one whose academic performance is
significantly below performance potential because of a specific
affective, cognitive, structural, or interpersonal difficulty [8].
American Board of Internal Medicine defines problem resident "as a
trainee who demonstrates a significant enough problem that requires
intervention by someone of authority, usually the program director or
chief resident." In simple terms, a problem resident is the one who does
not meet the expectations of the training program owing to the deficit
in knowledge, skill or attitude.
Statement of the Problem
In a study by Reame, et al. [5], the
prevalence of ’resident in trouble’ was estimated to be 9.1%. They
observed psychiatric illness, substance abuse, attitudinal problems,
interpersonal conflicts and insufficient knowledge to be the common
reasons. In another internal medicine residency program, the prevalence
of problem resident was estimated to be 6.9%. The most common
attributable causes included insufficient medical knowledge, poor
clinical judgment, and inefficient use of time [4]. In a nationwide
survey of psychiatry residency program in the United States, it was
observed that 3.3% of residents were terminated in a four-year period
for unacceptable performance [9]. Data from India on this issue are
lacking.
Predisposing Factors
Knowledge Deficit
One of the most common attributable cause of problem
resident is insufficient knowledge [5]. The resident may have poor
baseline subject knowledge or is slow to grasp the basic concepts
leading to an unsatisfactory performance at work (Box I).
The regular internal assessment might detect academic deficiency and
provides an opportunity to rectify the deficit. Lack of organizational
skills and ineffective time management are some of the other hurdles in
acquiring the requisite knowledge.
|
Box 1 Hunt’s Classification of Problem
Learner
Type I (frequent* and
difficult#)
• Bright with poor
interpersonal skill
• Excessively shy,
non-assertive
Type II (frequent* and not
difficult#)
• Poor integration skills
• Overeager
• Cannot focus on important
issue
• Disorganized
• Disinterested
• Poor knowledge
Type III (not frequent* and
difficult#)
• Cannot be trusted
• Psychiatric problem
• Substance abuse problem
• Manipulative
Type IV (not
frequent* and not difficult#)
• Too causal or informal
• Avoids works
• Intellectually inferior
• Avoids patient contact
• Does not show up
• Challenges everything
• Awkward
*How frequently do we
encounter this problem;
#How difficult is the problem to handle.
|
Skill Deficit
Skills required from clinical residents include the
art of history taking, correct method of clinical examination,
interpreting the clinical findings to reach a diagnosis, plan
investigation and managing the patients. One of the most essential
skills is communication of the plan to relatives and ability to discuss
the idea with colleagues and taking constructive criticism.
Communication difficulties, especially of those who travel from other
states to pursue their higher education, might have trouble
communicating in the local language. Majority of residents face problem
in skills during the first few months of residency that tends to improve
with time. Surgical hands-on skills often need constant supervision. The
persistent deficit of skill development despite repeated reinforcement
leads to a problem.
Attitude or Personal Problems
Attitude or personality problems stem from a deficit
in motivation. The problem resident often has a poor interpersonal
relationship and is not dependable for independent patient care (Box
2). Residents with attitude problems are the most difficult ones to
handle.
|
Box 2: Case Scenarios of Fictitious
Problem Residents
Fictitious Dr. Y
• She is very hard working, comes early to
wards, leaves very late.
• Unfortunately scores poor on assessment.
She takes many hours to analyze a patient’s history and still
does not make any sensible plan for individual patients.
• She does not understand the instructions of
seniors at one go. They need to repeat it multiple times.
• She often writes wrong doses of drugs or
sends false samples of a patient.
• She is never able to understand the
rationale behind the choice of investigation and management.
• Owing to this, She is considered
disorganized at work and faculty prefers not to assign any vital
work to him.
Fictitious Dr. K
• He often reports late to his duty or may be
absent without any prior information, and he usually keeps his
mobile phone switched off.
• There are frequent complaints from other
supportive staff regarding his rude behavior with patients and
his colleagues.
• He tends to fight, use abusive language,
and gets into confrontation mode when into an argument.
• He is often lazy, avoids works, gives lame
excuses and tends to blame others for his non-performance.
• He passes on his share of work to next
relieving resident.
• He is often spotted chatting over his
mobile phone during the working hours. He shows little interest
during the clinical rounds and is often seen wandering away from
the wards during his duty hours.
|
Problems pertaining to residents
Personal problems like bereavement from loss of loved
ones, struggle in the family, or difficulties in personal relations may
affect the performance of residents. Poor interpersonal relationships
lead to prejudiced work atmosphere and impair learning. Psychiatric
illness and substance abuse among residents needs early identification
and correction. These problems often result in stress, depression, low
self-esteem, and fear of failure.
Many students choose a medical or surgical specialty
based on their score rather than their interest. Such discordance may
result in a problem during the early days of residency. Few residents
have adjustment issues considering the latency of 2-3 years after
completion of medical school before they get into a specialty. In a
study by Hunt, et al. [10], it was observed that most common
problem learners were those with cognitive issues and poor interpersonal
relationship.
Problems pertaining to teachers
Faculty members with unrealistic expectations,
stressful personal life, or working in an unsatisfactory workplace often
vent out their anger and frustrations at the resident. The behavior may
initiate or exacerbate problems in the resident. An excellent role model
faculty produces better professional behavior among residents [11,12]. A
problematic faculty; however, is more likely to produce a problem
resident.
The teacher is often assigned the dual role of
clinician and teacher, and a few fail to live up to the expectations.
Few teachers may become oblivious to the problem resident altogether so
as to avoid direct confrontation and few may vent out their anger by
scolding the resident. On the other hand, few faculty members suddenly
become soft, primarily to avoid any possible personal litigations.
Often, faculty members are reluctant to provide an honest assessment of
the residents, and mark them as satisfactory despite being problematic
[13]. This only aggravates the situation.
Problems pertaining to system
Workplace learning varies widely between different
institutions, depending on opportunity, motivation, and capabilities
[14]. In government facilities, barriers to effective workplace learning
might include deficient infrastructure, deficient manpower, and
unmanageable patient load [15]. In addition, lack of access to peer,
lack of management support, lack of access to technology, lack of
funding, and unsupportive staff attitude are other barriers to workplace
learning [14]. Certain institutions despite having excellent
infrastructures may lack expertise and teaching exposure required during
residency training [16]. Many students migrate from one state to another
state for pursuing postgraduate residency. Relocation to a new
institution often invites financial concerns, isolation, and social
problems leading to resident stress and adjustment issues [17]. All
these factors may contribute to the making of a problem resident.
Unprofessional Behavior
Some of the professional etiquettes expected from
residents include being courteous to your colleagues and seniors, being
on time to work, wearing appropriate clothes to the hospital, showing
appropriate gestures while speaking to patients, and most importantly to
keep one’s grudges and egos away while dealing in a professional
atmosphere. Unprofessional blogs and social media posts such as binge
drinking, posting sexually appealing photos, sharing patient videos on
social media, posting raw or confidential data of institute, and
personal comments on faculty members or peer colleagues are some of the
commonly encountered problems [18,19]. Fabricating patient reports to
meet preoperative criteria, and verbal or physical abuse of junior
doctors are some of the extreme behaviors encountered among few
residents [20]. There is rising intolerance about relations of doctors
with pharmaceutical companies or private laboratories for some financial
or other favorable incentives [21].
Addressing A Problem Resident
The first step in the evaluation of a problem
resident is to be sure about the diagnosis [7]. A single adverse
incident, personal grudges, and overheard conversation may end up in
wrongly labelling a resident as a problem resident. Residents obviously
do not like to be outcasted as a problem resident [22]. It affects their
relations with peers, patients and teachers. A resident erroneously
blamed for any wrong happenings results in denial, anger and loss of
self-confidence [6].
Sharing all concerns over a faculty meeting is
essential [23]. A group consensus on a resident being a problem resident
is necessary before proceeding to determine the problem and its remedial
measure. Once the problem is identified, it would be useful to determine
how frequently do we encounter this problem, how difficult is it to
handle this problem, and how much is it affecting the ongoing learning
of the student and his/her peers [10]. For example, a resident who is
frequently absent from his duties owing to excessive alcohol abuse is
not a frequent but quite a difficult problem to handle. Likewise, a
disorganized first year with poor knowledge base is quite a common
problem, but it improves with interventions (Box 2).
Talk to the resident
The resident should be called for a meeting with the
program director who should list the concerns without criticizing or
discriminating the resident [23]. Perception of the problem by resident
and its possible remedial measures that he/she perceives should be
considered. Enquire about personal problems of the resident, including
those from family.
Talk to colleagues
Feedback from other supportive staff including peers,
nurses, support staff, and patient attendants might help [12]. It is
essential to identify the occurrence and frequency of problem and
situations where such a problem emerges. History of drug or alcohol
abuse needs to be ascertained from the peers [24]. Inter-resident
scoring cards are used to assess a resident as perceived by their peers
in an objective manner.
Designing remedial measures
Fictitious Dr. Y was disorganized and had a gross
deficit in knowledge and skills (Box 2). Owing to repeated
complaints from casualty team members, she was rotated to the general
pediatric ward. She was tagged to a mentor faculty and chief resident
who would intensely monitor his progress. They would conduct one to one
tutorial, assign her the additional reading task with fixed timelines,
and supervise her examination skills at the bedside. Her analytical
skills were sharpened by use of simple methods like one-minute preceptor
model [25]. Considering the hard-working nature of Dr. Y, she had an
excellent performance at the end of 3 months and then was rotated back
to the casualty team. She was tagged to a senior shadow peer for next
two months before she was assigned independent duties.
Fictitious Dr K had a major problem in attitude that
led to a negative and unprofessional workplace environment (Box
2). He was called for a meeting with the program director and all
faculty members. Problems encountered were enlisted, and justification
for the same was sought. A verbal warning was given, failing which a
written memorandum was issued. His parents were informed of the minutes
of the meeting. His responsibilities during clinical postings were
delineated, and he was not allowed to switch on his mobile phone during
work hours. His interactions with patients, peers and nurses were video
recorded. He became conscious of his actions being recorded. These video
records were reviewed in a subsequent meeting with the resident, and
corrective measures were suggested to him. A timeline was provided for
correction of his actions, failing which he was warned of possible
termination of his candidature for the program. He was tagged to a role
model teacher and peer with whom he worked for next three months. His
behavior improved dramatically. He was more polite, respectful and
considerate in his actions at the workplace. He would finish all his
work before leaving the ward.
Teaching medical professionalism is challenging, but
essential part of medical training. One of the most effective ways to
teach professionalism to residents is to foster faculty role modeling
[23]. Residents often look up to a positive role model to imitate
his/her professionalism. Majority of problem residents improve with
appropriate and timely remedial measures. Remedial measures must define
the deficiency, provide a pathway for its rectification, set minimal
benchmark goals or expectations in an acceptable timeline, and
evaluation based on set goals [13].
Broad identification of problem into cognitive,
behavioral or a combination of both is essential to design specific
cures. Majority of attitudinal problems require extensive close
monitoring and feedback, and, in some situations, require psychological
help. The structured reading session can be planned for those with the
poor knowledge base (Table I). The Problem Resident needs
to be involved in identifying the problems and designing their remedies,
based on his/her priorities.
Table I Remedial Measures for Problem Residents
|
Deficit domain |
Remedial measures |
|
Knowledge deficit |
One to one mentorship, faculty tutorials, creating reading
assignments with the timeline, peer support, increased frequency
of formal meeting with program director during the first year of
residency, regular reassessment, increased faculty advisor
meetings, identifying the best teacher or role model who could
probably sail through the tough time. |
|
Skill deficit |
Skill training, hands-on training, peer mentorship, supervised
or tagged resident, formal mentorship program tagging them to
likeminded faculty members, increased supervision by case
discussion, review of patient management problems, faculty
mentor to periodically monitor the gain of skills. |
|
Psychiatric issues |
Psychological and psychiatric consultation, appropriate
documentation of all meetings, the involvement of family members
is essential, consultation and remedial measures in a temporary
file can be helpful; medical clearance before the resident can
be brought back to work; can extend the training period for 3-6
months till health is returned. |
|
Adjustment issues |
Time is an effective healer. Majority respond and adjust to new
environment. Peer and faculty support helps. Providing easy
rotation in the beginning, monthly off days. providing leave of
absence, home sickness resolves with time once they start
enjoying residency, bringing parents to the hostel to spend some
more time till he gets adjusted. |
|
Attitude problem |
The probationary period during the residency program would be a
useful addition to observe for behavior and attitudes. Direct
observation of good patient-doctor interaction, video recording
the session and correcting the mistakes (videotape reviews).
|
|
Unprofessional behavior |
Stringent punitive action like a warning, issue of the
memorandum, seeking a written explanation for misbehavior,
temporary suspension from the program, the involvement of legal
cell of the institution to decide a plan of action. |
|
Problems at the faculty level |
Faculty orientation workshops on dealing with Problem
Residents, increased incentives for faculty involved in
teaching, effective feedback from students. |
|
Problems at the system level |
Decreasing work hours, providing conducive workplace, setting up
problem box in each department in which residents can
confidentially give honest feedbacks, feedback to system
director regarding the work environment. |
Three golden rules for correction include "act early,
maintain confidentiality, and document everything" [7,22]. The plan
should be individualized. Set up achievable goals and devise a timeline
for each of the desired goals. It is essential to identify the red flag
signs that require psychiatric consultation, including suicidal
tendency, harm to patient, and substance- or alcohol- abuse. Finally,
ensure that a problem resident graduates out of the department sans
his/her problems.
Prevention
Can we predict at the outset that a resident will be
problem resident? Robust educational system ideally should have rigorous
screening mechanism for recruiting residents for the teaching program. A
problem resident is often recognized within the first year of residency,
or more often they come to attention when a resident has poor
performance in the ongoing assessments. Periodic assessment of residents
should ideally include core medical knowledge, interpersonal skills and
communication, practice-based learning, and professionalism [23].
Few problems come to attention following a complaint
about the resident in some adverse event like fights with colleagues or
patient or when there is gross mismanagement for any patient. Indian
system recruits medical postgraduates through common written entrance
examination that often lacks personality assessment [26]. Moreover, with
the advent of online admission sessions, while allotting postgraduate
seats, institutions have no control over the recruitment of students.
Even resident with adverse remarks on the conduct certificate during
graduation years can safely land in prestigious institutions solely
based on cognitive abilities [27]. The selection procedure for residency
should not only look for core medical knowledge, but also the past
performance during the undergraduate course, the opinion of teachers and
peers. Screening for personality traits, motivation, character,
affective domains and communication skills need to be incorporated in
the selection process [28].
Once a resident is inducted into the system, an
orientation plan should be in place. It should include orientation to
the clinical postings and their expectations from residents. Importance
of socialization should be emphasized. They should go to movies, go to
dine outside, and have regular birthday parties even at the workplace –
during the lunch hours. Mentoring a resident is an essential aspect of
medical training [29]. It shapes the personal and professional
development of the resident. Effective incorporation of mentorship
program during residency could avert emergence of problem resident.
Mentors selected by free choice have been shown to be better than
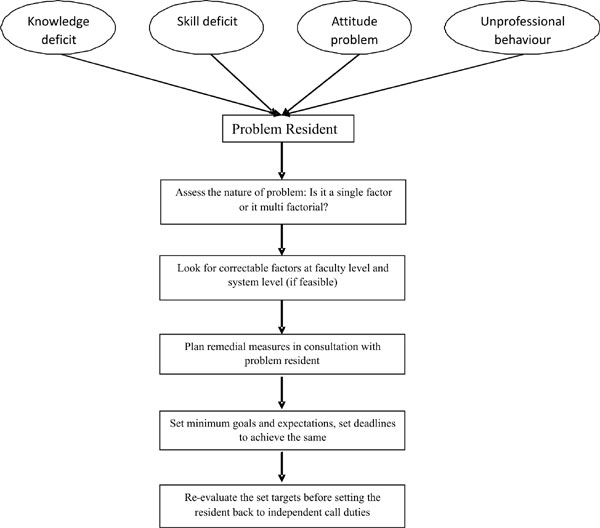
assigned mentors [30]. A broad approach to handling a problem resident
has been summarized in Fig. 1.
 |
|
Fig. 1 Approach to a problem
resident.
|
Conclusion
Resident doctors face a variety of professional and
personal problems, including deficits in knowledge, skills or problems
with attitude. Faculty members and institutional heads must be
sensitized to handle these problems. Remedial measures need to be
individualized and must be framed with the involvement of affected
resident. One-to-one faculty mentorship, peer support, psychological
consultation, rotating the resident out of difficult workplace,
stringent monitoring of their behavior, and providing effective feedback
are some of the remedial measures to handle a problem resident.
Providing enjoyable learning experiences should be the goal of every
residency program.

