|
|
|
Indian Pediatr 2019;56:49-52 |
 |
McIsaac Modification of
Centor Score in Diagnosis of Streptococcal Pharyngitis and
Antibiotic Sensitivity Pattern of Beta-hemolytic Streptococci in
Chennai, India
|
|
Jaishree Vasudevan, Alexander Mannu and G Ganavi
From Department of Pediatrics, Chettinad Hospital
and Research Institute, Chennai, Tamil Nadu, India.
Correspondence to: Dr Jaishree Vasudevan, Professor,
Department of Pediatrics, Chettinad Hospital and Research Institute,
Kelambakkam, Chennai 603 103, India.
Email: [email protected]
Received: January 04, 2017;
Initial review: June 14, 2017;
Accepted: October 18, 2018.
|
Objective: To assess the
validity of modified Centor Score in predicting streptococcal
pharyngitis, and describe the antibiotic sensitivity of streptococcal
strains. Methods: A cross-sectional study of 120 children (age
1-18 y) with signs and symptoms of pharyngitis was undertaken in the
pediatric department of a tertiary care teaching hospital in Chennai
from July 2015 to April 2016. Modified Centor score was calculated for
all children, and streptococcal sore throat was confirmed by throat swab
culture. Predictive validity of Centor score was assessed by Receiver
Operating Curve (ROC) analysis. Results: Streptococcal culture
positivity was 35%. The Area Under the Curve (AUC) value for modified
Centor score was 0.589 (95% CI 0.481 to 0.697, P=0.11) in
predicting streptococcal pharyngitis. Cough had the highest sensitivity
(63.4%), but poor specificity (36.7%) for streptococcal pharyngitis
confirmed by culture. The specificity was 100% for palatine petechiae,
followed by palatine exudates (97.5%) and tender anterior cervical nodes
(88.6%) to diagnose streptococcal pharyngitis. The proportion of
antibiotic resistance was highest for cotrimoxazole (16.7%).
Conclusion: Predictive validity of modified Centor score was not
satisfactory, and resistance to cotrimoxazole, fluoroquinolones and
macrolides was high among S. pyogenes strains.
Keywords: Antimicrobial resistance, Streptococcus pyogenes,
Upper respiratory infection.
|
|
S
treptococcal pharyngitis can lead to a plethora
of suppurative and nonsuppurative complications [1], which can be
prevented by prompt diagnosis and institution of appropriate antibiotic
therapy. However, due to considerable overlap in clinical presentation,
differentiating streptococcal pharyngitis from other causes is
difficult. Non-availability of culture and sensitivity in many of the
healthcare settings in resource-poor countries precludes its routine
use. Delay in diagnosis leads physicians to administer empirical
therapy, leading to overuse of antibiotics, which results in a rise in
drug-resistant bacterial strains [2]. Various alternative diagnostic
methods, including clinical scoring systems [3,4] and rapid antigen
detection testing (RADT) [5] have been developed for diagnosis of
streptococcal pharyngitis. It is important to validate these scores for
effective diagnosis and treatment of GABHS pharyngitis and prevention of
subsequent complications. The present study was conducted to assess the
utility of various clinical manifestations and McIsaac modification of
Centor score in predicting streptococcal pharyngitis in pediatric age
group, and describe the sensitivity pattern of isolated streptococcal
strains.
Methods
This cross-sectional study was undertaken in the
department of pediatrics of a tertiary-care teaching hospital in
Chennai, India, from July 2015 to April 2016. Children aged between 1 to
18 years presenting to the outpatient department with symptoms of
pharyngitis and clinically suspected as streptococcal pharyngitis were
included in the study. Children who presented with obvious signs of
viral respiratory infection (having rhinorrhea, coryza, conjunctivitis,
coughing and/or sneezing) were excluded. Children who were already on
antibiotics were also excluded.
All screened children were recruited by purposive
sampling sequentially, till the sample size was reached. Approval of the
Institute Human Ethics Committee was obtained. Informed written consent
was obtained from the parents or guardians of all the participants.
All the children were evaluated by a pediatrician.
Demographic and clinical data were collected from the children. Clinical
examination of the pharynx and tonsils was conducted under flash light
illumination. All the variables related to modified Centor score were
documented and score was calculated for each child. The
clinician collected the sample from pharyngeal wall (after depressing
tongue with tongue depressor) by a sterile cotton swab applied on the
tip of 6-7 inches long swab stick. Cotton swab was rubbed gently against
pharyngeal mucosa. All precautions to avoid contamination were taken and
the samples were immediately transported to the microbiology department
in a sterile test tube at room temperature. Smear was examined by Gram
staining, and Blood Agar was the culture media used for culture.
Any growth observed on culture medium was assessed for morphology (smear
examination), colony characteristics and biochemical tests. Isolates
were subjected for antibiotic sensitivity as per CLSI guidelines.
Throat swab culture positivity was considered as the
primary outcome variable. Various sociodemographic, lifestyle related
parameters were considered as exploratory variables. The children with
and without culture positive infection were compared with respect to
demographic, clinical variables and modified Centor score. The
association between the symptoms, signs and modified Centor score with
culture positivity was assessed by cross tabulation and chi-square test.
IBM SPSS version 21.0 was used for statistical analysis. P <0.05
was considered statistically significant.
Results
A total of 120 participants were included in the
analysis. About 35% in the study population had streptococcal sore
throat. Only one child had throat swab culture positive for
Staphylococcus aureus. The streptococcal positivity was 28% among 1
to 5 year, 40% in both 6 to 10 year and more than 11-year-old age
groups. The proportion of streptococcal pharyngitis increased with
increasing Centor score category. Among the symptoms, cough, throat
pain, painful swallowing and difficulty in swallowing showed
statistically significant difference among streptococcal and
nonstreptococcal pharyngitis (Table I).
TABLE I Factors Associated with Streptococcal Pharyngitis in the Study Population (N=120)
|
Parameter |
Culture positive (n=42), n(%) |
Culture negative (n=78), n(%) |
P value |
|
Male gender |
21 (38.9) |
33 (61.1) |
0.42 |
|
Centor score |
|
|
|
|
-1 to +1 |
9 (23.7) |
29 (76.3) |
0.14 |
|
2 to 3 |
13 (34.2) |
25 (65.8) |
|
|
4 to 5 |
15 (41.7) |
21 (58.3) |
|
|
Above 5 |
5 (62.5) |
3 (37.5) |
|
|
Symptoms |
|
|
|
|
Cough |
26 (34.2) |
50 (65.8) |
0.81 |
|
Throat pain |
28 (43.7) |
36 (56.2) |
0.03 |
|
Fever |
26 (40.6) |
38 (59.4) |
0.16 |
|
Rhinorrhea |
16 (32) |
34 (68) |
0.57 |
|
Painful swallowing |
19 (54.3) |
16 (45.7) |
0.004 |
|
Difficulty in swallowing Signs |
13 (56.5) |
10 (43.5) |
0.02 |
|
Erythematous pharynx |
30 (46.1) |
35 (53.8) |
0.005 |
|
Erythematous tonsils |
31 (48.4) |
33 (51.6) |
<0.001 |
|
Enlarged anterior cervical nodes |
21 (58.3) |
15 (41.7) |
<0.001 |
|
Tender anterior cervical nodes |
13 (59) |
9 (40.9) |
0.009 |
|
Enlarged tonsils |
12 (50) |
12 (50) |
0.08 |
|
Tonsilar exudates |
3 (75) |
1 (25) |
0.09 |
|
Palatal petechiae |
2 (100) |
0 (0) |
0.05 |
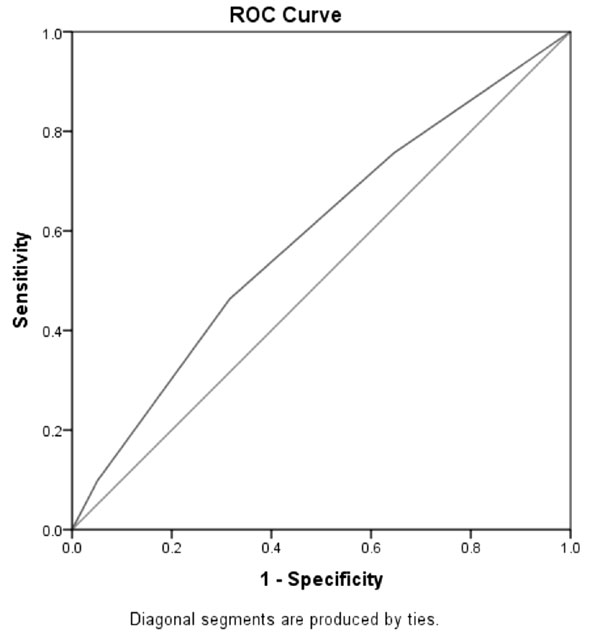
The area under the curve value for modified Centor
score was 0.589 with a P value 0.11 and 95% CI was 0.481 to
0.697, respectively in the study population. Among symptoms, cough had
the highest sensitivity (63.4%), but poor specificity (36.7%). Palatine
petechiae had 100% specificity, but very poor sensitivity (4.9%). Tender
anterior cervical nodes and palatine exudates also had very high
specificity (88.6% and 97.5%, respectively) but poor sensitivity (Table
II).
TABLE II Sensitivity and Specificity of various Clinical findings in Diagnosis of Streptococcal Pharyngitis
|
Factors |
Sensitivity |
Specificity |
Positive predictive value |
Negative predictive value |
|
Cough |
63.4% |
36.7% |
34.2% |
65.9% |
|
Tender anterior cervical nodes |
31.7% |
88.6% |
59.1% |
71.4% |
|
Palatine petechiae |
4.9% |
100% |
100% |
66.9% |
|
Tonsillar exudates |
4.9% |
97.5% |
50.0% |
66.4% |
|
Modified centor score |
12.2% |
96.2% |
62.5% |
67.9% |
The proportion of antibiotic resistance was highest
for Cotrimoxazole (16.7%), followed by tetracycline (9.5%).
Ciprofloxacin and Ofloxacin resistance was seen in 7.1% of the study
population. Erythromycin resistance was seen in 4.8% of the strains.
Intermediate resistance was found for Erythromycin (4.8%), Azithromycin
and Ofloxacin (2.4%).
Modified Centor score of 4 had a poor sensitivity
(12.2%, 95% CI 4.8% to 26.2%), but very high specificity (96.2%, 95% CI
89.3% to 99.2%) in predicting streptococcal pharyngitis. The overall
diagnostic accuracy was 67.5% (95% CI 58.4% to 75.8%). Even though the
positive likelihood ratio was 3.21, the 95% confidence interval ranged
from 0.81 to 12.77. The negative likelihood ratio was 0.91 (95% CI 0.81
to 1.03).
Discussion
In this study, the overall predictive validity of
modified Centor score, as assessed by Area under ROC curve was poor.
Palatine petechiae, tonsillar exudates and tender anterior cervical
lymph nodes had high specificity and positive predictive value in
diagnosis of streptococcal pharyngitis. Streptococcus pyogenes
strains were sensitive to penicillin. However, resistance to
Cotrimoxazole (16.7%), tetracycline (9.5%), fluoroquinolones and
macrolides was high.
 |
|
Fig. 1 ROC analysis of predictive
validity of modified Centor score in predicting streptococcal
pharyngitis.
|
The AUC reported in the original 1981 study by Centor
[3] was 0.78, which is considerably higher compared to our study.
McIssac, et al. [4] modified the score, and reported high (83.1%)
sensitivity. Few other studies from the West have reported AUC value
higher than 0.7, indicating good predictive validity [6]. Another study
had reported an area under the ROC of 0.633 [7]. A study had reported a
strong positive association between tonsillar exudates and culture
positive Group A streptococcal (GAS) sore throat [7]. But there are
other studies, which have documented sensitivity as low as 3.9% for a
modified Centor score of 4, with a high specificity of 96%, as in
current study [8]. Similar pattern of low sensitivity and higher
specificity has been demonstrated by few other studies [9,10]. Lowering
the cut-off level of modified Centor score, has shown to increase the
sensitivity, but at the cost of specificity, which may result in
increase in unnecessary antibiotic prescription [6].
The reasons for such a wide variation in reported
predictive validity needs to be evaluated. The key differences in the
demographic characteristics, differences in the clinical presentation,
and quality of clinical assessment may be responsible for these
differences. The same factors may determine the clinical utility of
modified Centor score.
The limited sample size in the study was a major
limitation that did not allow for controlling for the effect of
confounding or detailed analysis of factors associated with culture
positive infection. Exclusion of possible viral etiology on clinical
grounds alone was another limitation that can affect generalizability of
these results.
We conclude that the predictive validity of Centor
score for diagnosis of streptococcal pharyngitis is poor, and its
utility as screening tool is questionable. Considering very low
sensitivity, high proportion of streptococcal sore throat may be missed,
if modified centor score is used a screening tool.
Contributors: JV: had conceptualized the
idea, prepared the study proposal, engaged in data compilation, analysis
and preparation of all the drafts of the manuscripts; AM,GG: have
fine-tuned the study proposal, engaged in data collection, reviewed all
the drafts and provided their inputs. They have compiled, verified and
approved the final draft. All authors have contributed, designed
and approved the study.
Funding: None; Competing interest: None
stated.
|
What This Study Adds?
• Presence of
palatine petechiae, tonsillar exudates and tender anterior
cervical lymph nodes may guide in starting antibiotic therapy in
children with pharyngitis, but McIssac modification of Centor
Score does not seem to perform satisfactorily.
|
References
1. Gerber MA. Group A Streptococcus. Nelson Textbook
of Pediatrics: Elsevier; 2011. p. 914-25.e1.
2. Ayanruoh S, Waseem M, Quee F, Humphrey A, Reynolds
T. Impact of rapid streptococcal test on antibiotic use in a pediatric
emergency department. Pediatr Emerg Care. 2009;25:748-50.
3. Centor RM, Witherspoon JM, Dalton HP, Brody CE,
Link K. The diagnosis of strep throat in adults in the emergency room.
Med Decis Making. 1981;1:239-46.
4. McIsaac WJ, White D, Tannenbaum D, Low DE. A
clinical score to reduce unnecessary antibiotic use in patients with
sore throat. CMAJ. 1998;158:75-83.
5. Kundu R. Rapid diagnostic tests in childhood
infections. Indian Pediatr. 2018;55:233-7.
6. Fine AM, Nizet V, Mandl KD. Large-scale validation
of the Centor and McIsaac scores to predict group A strepto-coccal
pharyngitis. Arch Intern Med. 2012;172:847-52.
7. Atlas SJ, McDermott SM, Mannone C, Barry MJ. The
role of point of care testing for patients with acute pharyngitis. J Gen
Intern Med. 2005;20:759-61.
8. Orda U, Mitra B, Orda S, Fitzgerald M, Gunnarsson
R, Rofe G, et al. Point of care testing for group A streptococci
in patients presenting with pharyngitis will improve appropriate
antibiotic prescription. Emerg Med Australas. 2016;28:199-204.
9. Palla AH, Khan RA, Gilani AH, Marra F. Over
prescription of antibiotics for adult pharyngitis is prevalent in
developing countries but can be reduced using McIsaac modification of
Centor scores: a cross-sectional study. BMC Pulm Med. 2012;12:70.
10. Regoli M, Chiappini E, Bonsignori F, Galli L, de
Martino M. Update on the management of acute pharyngitis in children.
Ital J Pediatr. 2011;37:10.
|
|
|
 |
|

