|
|
|
Indian Pediatr 2019;56:41-44 |
 |
Wrist Deformity in Children and
Adolescents with b-thalassemia
on Oral Iron Chelation Therapy
|
|
Rashid H Merchant 1,
Ameya Kulkarni2,
Pezad N Doctor1,
Amitkumar Choudhari2
and
Deepak P Patkar2
From Departments of 1Pediatrics and 2Radiology,
Nanavati Super Speciality Hospital, Vile Parle East, Mumbai,
Maharashtra, India.
Correspondence to: Dr Pezad N Doctor, Department of
Pediatrics, Nanavati Super Speciality Hospital, Mumbai, India.
Email: [email protected]
Received: December 30, 2017;
Initial review: May 04, 2018;
Accepted: November 01, 2018
|
Objective: To describe a novel wrist deformity in
b-thalassemia
major patients, and their radiographic and magnetic resonance imaging
findings. Methods: 30 patients with
b-thalassemia
major who were noticed to have ulnar deviation at wrist joint were
evaluated for previous history of medications, serum ferritin levels,
presence of pain and swelling at the wrist joint, and the duration of
iron chelation therapy. Radiographs of wrist and limited magnetic
resonance imaging (MRI) sequences were obtained in 30 and 15 patients,
respectively. Results: Radiographs revealed varying severity of
distal ulnar shortening, distal radial slanting and presence of soft
tissue distal to the ulna. MRI showed similar deformities along with
abnormal marrow signal at distal ulnar ends; in 8 patients, a soft
tissue distal to the distal end of ulna was noted.Conclusion:
Varying severity of radiological abnormalities, predominantly affecting
the distal ulna, are present in children and adolescents with
b-thalassemia
receiving oral chelation therapy.
Keywords: Arthropathy, Bone deformity, Deferiprone, Growth
plate.
|
|
Iron overload in
b-thalassemia major patients due to repeated blood
transfusions requires administration of iron chelation therapy in the
form of parenteral Desferioxamine (DFO) or oral iron chelators such as
Deferiprone (DFP) or Deferasirox (DFX). Mild arthropathy occurs with the
use of DFP that usually resolves either on its own, with the use of
non-steroidal anti-inflammatory drugs, or by temporary withdrawal of
therapy [1-3]. The long-term outcome of DFP-related arthropathy is not
known, and is not adequately documented in literature [4,5]. We aimed to
describe radiographic findings in children who were receiving DFP at
some point during their treatment course.
Methods
At a thalassemia day care center in Mumbai, during
the period from February 2014 to March 2017, records of 155
b-thalassemia major
patients were evaluated. Thirty of these patients, aged 12 to 18 years,
were noted to have bilateral wrist deformity with ulnar deviation (Fig.
1). Iron chelation therapy had been initiated after receiving 20
units of packed red blood cells (PRBCs) or when serum ferritin levels
were above 1000 µg/L. Change in drugs for chelation therapy was made
when serum ferritin exceeded 2500 µg/L, intolerance to the drug, or
non-response to a single agent.
 |
|
Fig. 1 Bilateral ulnar deviation at
wrist joint in a 13-year-old boy with
b-thalassemia
receiving oral iron chelation.
|
These 30 patients with asymptomatic wrist joint
deformity were further evaluated with reference to their bony
abnormality. Informed consent was obtained from the parents for
radiological investigations and clinical photographs. Ethical approval
for the study was obtained from Ethics Committee of Dr Balabhai Nanavati
Hospital, Mumbai, India.
Radiographs of wrist of all 30 children were
evaluated by a single reader (AK) who was not blinded to the clinical
deformity. MRI coronal T-1 and T-2 weighted sequences of wrist were
obtained using a 3 Tesla, Discovery 750W scanner (GE healthcare,
Milwaukee, USA). MRI findings were evaluated by two readers (AC and DP).
Serum calcium, phosphorous, alkaline phosphatase and 25-hydroxy Vitamin
D3 levels were done along with serum ferritin levels in all patients.
Results
In 30 patients (21 boys) noted to be having bone
deformity, the median (IQR) age was 15 ( 2.25) years, and the duration
of deferiprone therapy ranged from 1.5 to 16 years with a median (IQR)
of 8.25 (5.75) years. There was no history of trauma, skeletal
dysplasia, prior surgical intervention of the wrist joint or any other
skeletal deformities.
The median (IQR) serum ferritin level when the wrist
deformity was diagnosed was 2350 (1690) ng/dL. The serum calcium,
phosphorous, alkaline phosphatase and 25-hydroxy Vitamin D3 were normal
in all patients. All children had received DFP in doses ranging from
75-100 mg/kg/day at the initiation of iron chelation between ages of 2
to 8 years. Twenty of these were presently on oral DFX in doses ranging
from 30-40 mg/kg/day as a single agent, four were receiving a
combination of DFX and DFP, four were receiving injectable DFO in doses
30-40 mg/kg/day and DFP, while two were on DFO and DFX. Ten patients on
DFP developed severe arthralgia in knee joint with no wrist pain,
necessitating shift of therapy to DFX. At the time of evaluation, only
eight were receiving DFP in combination with another iron chelator.
Radiographic changes observed included shorte-ning of
distal ulna at wrist in 17 (Fig. 2), shortening of ulna
with rotation of scaphoid, and distal radial slant in 4, shortening of
ulna with deformity at wrist along with degenerative changes at
radio-carpal joint and abnormal shortening of ulnar third of the radial
epiphysis in 7, and shortening of ulna with rotation of scaphoid and
scapho-lunate dislocation with a positive Terry Thomas sign in 2 [6]. No
patient had pain, swelling or restricted movement of the wrist joint or
any other joint swelling or deformity.
 |
|
Fig. 2 Radiograph of both wrist shows
shortening of distal ulna. Scaphoid bones show abnormal
orientation bilaterally with scapho-lunate dislocation (arrow).
|
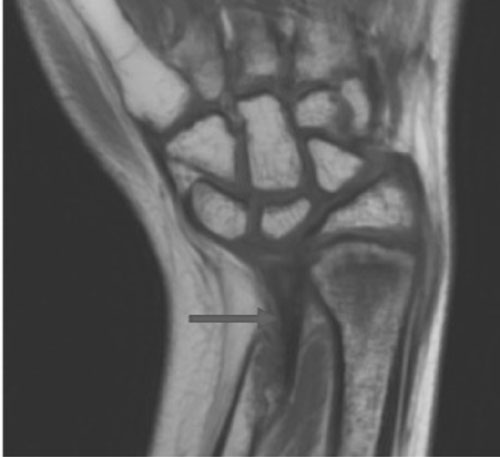
MRI coronal T-1 and T-2 weighted images obtained in
15 randomly selected patients showed similar deformities as those seen
on radiographs along with abnormal marrow signal at distal ulnar end. In
eight cases with significant ulnar shortening, there was a soft tissue
present distal to the distal end of ulna, likely to be due to abnormal
fibrous tissue in the region of distal radio-ulnar joint (Fig.
3). Osteonecrosis of scaphoid was seen in one case.
 |
|
Fig. 3 Coronal T1-weighted MRI of
right wrist shows shortening of distal ulna resulting in wrist
deformity. Arrow points to a hypo-intense tissue distal to the
distal end of ulna, which is likely to be fibrous tissue in
relation with the distal radio-ulnar joint.
|
Discussion
We noted the radiographic wrist deformity affecting
the distal ulna in children with b-thalassemia
major, which predominantly showed lucency and thinning of the ulnar
metaphysis, deformed small ulnar epiphysis and impaired growth of the
physeal cartilage leading to ulnar shortening. The clinical wrist
deformity was more apparent in older children as impaired physeal growth
of the ulna may have resulted in progressive shortening of the ulna in
comparison to the radius. In addition, MRI provided further information
regarding marrow signal and soft tissue involvement.
The study evaluated a population of patients visiting
our centre with wrist deformitis after being on iron chelators for
variable duration of time. The major limitation was that it was a
cross-sectional observational study, and there was no long-term,
longitudinal followed up to document the progession of this deformity.
The cumulative doses of iron chelators used were not calculated and
compared as they varied with age, weight and serum ferritin levels of
the children.
DFO therapy can result in skeletal dysplasia with
metaphyseal widening of long bone, rachitic changes, shortening of the
vertebrae, distal ulnar metaphyseal and occasional epiphyseal sclerosis
and thinning [7,8]. The mechanism of skeletal dysplasia may be either
due to the binding of zinc or the anti-proliferative effect of DFO [8].
Only six of our patients received DFO for a prolonged period of two
years or more after the age of ulnar epiphysis formation, and thus DFO
is unlikely to be the cause of ulnar deformities in our series of
patients. DFP can also cause chondromalacia, and is toxic to growing
tissues such as bone marrow [7,9]. DFP causes an arthropathy that
usually involves the knees [10]. However, Sharma, et
al. [5] reported abnormal wrist X-rays findings in 13 out of
40 patients receiving deferiprone; clinical ulnar deviation at the wrist
joint was noted in 4 patients in their series. There are no earlier
reports describing MRI findings of wrist in patients receiving iron chelation therapy.
The exact etiology of the arthropathy associated with
DFP remains uncertain; however, it has been hypothesized to be due to
the toxic effects mediated by free iron radicals, resulting from the
formation of 1:1 or 2:1 Deferiprone–iron complexes rather than the
usual, inert, 3:1 complexes [10,11]. These unstable complexes catalyze
the formation of free oxygen and hydroxyl radicals, damaging the distal
epiphysis and metaphysis of ulna.
Sharma, et al. [5] previously postulated that
the anti-proliferative effect of DFP may explain the toxic effects on
the growth cartilage. They further explained the propensity for ulnar
changes as ulnar epiphysis develops approximately between four to six
years of age [12], the age at which all their patients had been
receiving deferiprone. Prospective cohort
studies might help us understand the progression of this deformity and
the associated disability. Large controlled studies with different iron chelators are required to assess the causal relationship of this
deformity with DFP.
Contributors: RHM: conceptualized the study and
drafted the manuscript. AK: collected data, revised the manuscript and
evaluated radiological images; PD: collected data, reviewed literature,
revised the manuscript and critically reviewed it; AC: revised the
manuscript, evaluated radiological imaging and analysed data; DP: helped
in data analysis, radiological evaluation, manuscript writing and
literature search.
Funding: None; Competing interest: None
stated.
|
What This Study Adds?
• X -ray
and MRI changes in the wrist joint are seen in a subset of
children and adolescents with
b-thalassemia
major who received oral iron chelation therapy with deferiprone.
|
References
1. Cohen AR, Galanello R, Piga A. Safety profile of
the oral iron chelator deferiprone: A multi-centre study. Br J Haematol.
2000;108:305-12.
2. Naithani R, Chandra J, Sharma S. Safety of oral
iron chelator deferiprone in young thalassaemics. Eur J Haematol.
2005;74:217-20.
3. Al-Refaie FN, Hershko C, Hoffbrand AV, Kosaryan M,
Olivieri NF, Tondury P, et al. Results of long-term deferiprone
(L1) therapy: A report by the International study group on oral iron
chelators. Br J Haematol. 1995;91:224-9.
4. Kellenberger CJ, Schmugge M, Saurenmann T, Gennaro
LD, Eber SW, Willi UV, et al. Radiographic, MRI features of
deferiprone-related arthropathy of the knees in patients with
b-thalassemia.
Am J Radiol. 2004;183:989-94.
5. Sharma R, Anand R, Chandra J, Seth A, Pemde H,
Singh V. Distal ulnar changes in children with thalassemia and
deferiprone related arthropathy. Pediatr Blood Cancer. 2013;60:1957-62.
6. Frankel VH. The Terry-Thomas sign. Clin Orthop
Relat Res. 1977;129:321-2.
7. Chan YL, Pang LM, Chik KW, Cheng JC, Li CK.
Patterns of bone disease in transfusion dependent homozygous thalassemia
major: Predominance of osteoporosis and deferoxamine-induced bone
dysplasia. Pediatr Radiol. 2002;32:492-7.
8. Chan YL, Li CK, Pang LM, Chik KW. Deferoxamine
induced long bone changes in patients – radiographic features,
prevalence and relations with growth. Clin Radiol. 2000;55:610-4.
9. Berdoukas V, Bentley P, Frost H, Schnebli HP.
Toxicity of oral iron chelator L1. Lancet. 1993;341:1088.
10. Diav-Citrin O, Koren G. Oral iron chelation with
deferiprone. Pediatr Clin North Am. 1997;44:235-47.
11. Berkovitch M, Laxer RM, Inman R, Koren G,
Pritzker KP, Fritzler MJ, et al. Arthropathy in thalassemia
patients receiving deferiprone. Lancet. 1994;343:1471-2.
12. Greulich WW, Pyle SI. Radiographic atlas of
skeletal development of the hand and wrist. 2nd edition. Stanford,
California: Stanford University Press. October 1959. p. 513.
|
|
|
 |
|

