The World Association of Perinatal Medicine defines a
fetus as viable when it is mature enough to survive into the neonatal
period with the clinical support that is available. More objectively,
Periviable birth is currently defined as delivery occurring from 20 0/7
weeks to 25 6/7 weeks of gestation [1]. The outcome of these babies
ranges from certain or near-certain mortality to likely survival with a
high chance of long-term morbidities. When delivery is anticipated near
the limit of viability, both the family and caregiver are faced with
many complex and ethically challenging decisions.
The clinical support available in India varies across
the country and even within cities. The lack of widespread accreditation
of neonatal units makes it difficult to determine the type of support
available in a given unit. Currently, the focus is increasingly on the
ethics of giving support to neonates that are born very preterm. Since
most of India receives healthcare from out-of-pocket expenses, the
debate around care of the extremely preterm neonates often attracts
unfavorable media attention.
In this article, we discuss issues on survival and
outcomes of extremely premature infants, available guidelines, and try
to provide guidance on the need to develop a process locally that can
address this issue.
Survival and Long-term Outcomes
Historically, neonatal mortality is considered an
inevitability at or before 24 weeks of gestation [2,3]. While, we do not
have any data on the outcomes of these babies from India, a review of
studies from the past few decades do reveal an increase in the rate of
survival of newborns born at 22-25weeks of gestation [4-7]. The rates of
survival to discharge increase with increasing gestational age of
periviable babies (23-27% for births at 23 weeks, 42-59% for births at
24 weeks, and 67-76% for births at 25 weeks) [4,5,7].
Data trends on long-term sequelae are the same,
showing better outcomes at higher gestations. A follow-up study of a
cohort of periviable babies in England, demonstrated a decrease in the
proportion of children at age 30 months with severe or moderate
impairment, with increasing gestational age at birth (45% at 22-23
weeks, 30% at 24 weeks, and 17% at 25 weeks of gestation) [8]. A review
by Moore, et al. [9] also established that the incidence of
moderate-to-severe neurodevelopmental impairment among survivors at 4-8
years improved with higher gestational age at birth: 43% at 22 weeks,
40% at 23 weeks, 28% at 24 weeks, and 24% at 25 weeks of gestation.
However, even though the combined rate decreased, the rate of severe
neuro-developmental impairment alone did not vary significantly with
gestational age. A study from United States discussed survival and
long-term neurologic outcomes in more than 4,000 births from 2001 to
2011 that were between 22 to 24 weeks of gestation [9]. The results
demonstrated an actual increase in rate of survival without impairment
in the study duration, whereas the rate of survival with impairment has
remained constant. However, the lack of data from Indian settings makes
us wary of drawing any such conclusions.
The Ethics of Decision-making in the Delivery Room
The ethical principles, even in preterm infants,
remain the same as applied to other areas of medicine. The guiding
principles for the neonatologist are – beneficence (doing good), non-maleficence
(doing no harm), autonomy (respecting individual preferences) and
justice.
The principle of beneficence is a major force behind
the efforts to rescue these newborns. Traditionally, medicine’s ability
to prolong life is taken as unqualified good. However, in case of these
very premature babies, it needs to be decided whether use of medical
technology is actually postponing death rather than prolonging life.
Furthermore, life may not always be preferable to death, when continuing
life means deep suffering, a common scenario for these very premature
babies. The principle of non-maleficence is then taken into account as
significant suffering must be justified by expected outcome, while
inflicting such suffering may become unjustifiable when the likelihood
of survival becomes extremely small.
The application of the principle of autonomy is
complicated, as infants have no autonomy. Both parents and physicians
have a moral right and a legal duty to make treatment decisions in the
best interests of the baby. Parents and physicians may disagree
regarding the course of action – pertaining to uncertain medical
outcomes, different values, resources, tools and outlook [10]. For
physicians, there is a greater focus on technical components, such as
outcome data, evidence-based prognostic tools, and the clinical picture,
such as the actual presentation of the baby at birth. Conversely,
parents are generally more emotionally and psychologically invested in
any decision made, lacking the technical expertise to assess complex
clinical information.
Lastly, the principle of justice implies not only
treating similar preterm babies similarly, but also effectively using
resources (distributive justice). Aggressive care of extremely premature
babies with a remote possibility of intact survival may be considered an
inappropriate allocation of resources. Add to this a public-private
co-operation health system with variation in availability of resources,
inherently leading to unfairness.
Despite, such complexities in decision-making, it
must be remembered that the decisions that are made are going to impact
the entire life of the baby and the family; and many decisions such as
stopping care are not reversible and can have long-term impact on the
mental health of the parents. Hence, having a decision-making framework
is beneficial for all stakeholders in the process.
President’s Commission, 1983
This was a landmark decision-making framework,
although not meant specifically for treatment dilemmas at the threshold
of viability, the commission proposed ethically appropriate physician
responses to parental requests for the provision or withholding of
treatment in each of three treatment categories, viz., clearly
beneficial, of uncertain benefit, or futile [11] (Table I).
TABLE I President’s Commission’ 1983 [11]
|
Physician assessment of treatment |
Parents prefer to accept treatment
|
Parents prefer to forego treatment
|
|
Clearly beneficial to the infant
|
Provide treatment
|
Provide treatment (seek legal or other review) |
|
Ambiguous or uncertain benefit to the infant
|
Provide treatment
|
Withhold/ withdraw treatment
|
|
Futile
|
Provide treatment unless provider declines to do so
|
Withhold/ withdraw treatment |
As long as this choice does not cause substantial
suffering for the child, providers should accept it. Although,
individual health care professionals who find it personally offensive to
engage in futile treatment may arrange to withdraw treatment.
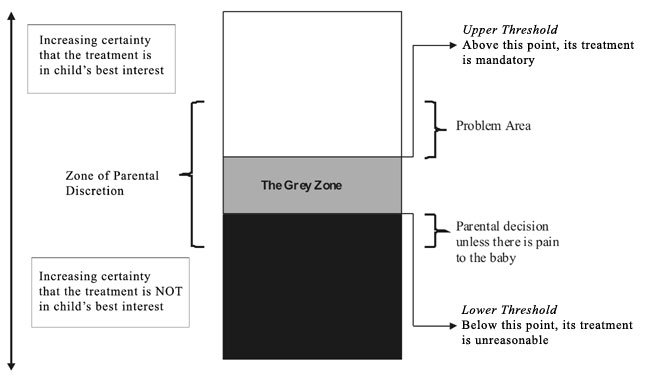
The Grey Zone and Zone of Parental Discretion
Most of the periviable babies die, while majority of
survivors have long-term morbidities. It is a difficult decision for
doctors and parent – whether you decide to treat them with the knowledge
that more often than not such efforts will be unsuccessful and result in
huge discomfort to the baby. On the other hand, not giving treatment
allows some of these babies to die who might have been saved? This is
the Grey Zone [12].
The zone of parental discretion is the ethically
protected space where parents may legitimately make decisions for their
children, even if the decisions are sub-optimal for those children [13].
|
Box 1 Guiding Principles in the Grey Zone
• Understand parents’ view on optimizing
survival or minimizing suffering beforehand during antenatal
counselling and discussion sessions.
• Keep in mind the institutional policies and
local laws.
• A stepwise approach based on newborn’s
condition and parental wishes is appropriate. Care should be
regularly re-evaluated and redirected.
• Decision for continuing care or otherwise
should be individualized – specific clinical issues, family
values/wishes, and ongoing evaluation of fetal or neonatal
condition.
• Multidisciplinary neonatal palliative care
should be provided in babies with the decision to withdraw or
withhold care.
• Healthy parent-clinician relationship with sharing of the
decision-making responsibility.
|
In the Grey Zone, the dictum is to follow parents’
wishes. The major problem area for neonatologists is when the zone of
parental discretion overlaps with area above the grey zone where
treatment is considered mandatory, but there is difference of opinion
between caregivers and parents (Fig. 1). The major guiding
principles in the Grey zone are detailed in Box 1.
 |
|
Fig. 1 Conceptual framework for the
grey zone in treatment decisions.
|
Shared Decision-making
Under ordinary circumstances, parents are likely to
be the best advocates for their infants. Therefore, parental wishes
should generally be followed, and issues important to them should be
considered in decision-making. In cases of borderline viability,
clinicians may feel compelled to advocate for the neonate and provide
treatment against parental wishes. Such decisions are not ethically
justifiable if it is impossible to weigh up the potential harms to the
child or to consider what is in the best interests of the child due to a
lack of prognostic certainty.
Neonatal Palliative Care
In newborns affected by life-threatening or
life-limiting conditions, when prolonging survival is no longer a goal,
a plan of care focused on the infant’s comfort is essential. These
strategies identify and address the basic needs of the newborn such as
bonding, maintenance of body temperature, relief of hunger/thirst, and
alleviation of discomfort. It is a multidisciplinary care given the
complex needs of infants and their families. Professionals like social
workers, workers from non-governmental sector, psychologists, child life
specialists, and spiritual representatives need to be actively involved
in the care to address psychosocial, financial, emotional, practical,
and spiritual needs of the family.
It is no surprise that parents of babies who have
received palliative services are more likely to be satisfied with the
care compared with parents whose infant did not receive it [14]. Thus,
the authors feel that there is an urgent requirement to standardize
neonatal palliative care practices and educate caregivers regarding
palliative care.
Withdrawal and Withholding of Care
Both ethicists and clinicians generally accept that
there is no significant ethical difference between withholding and
withdrawing intensive care measures [15]. However, for some parents
withdrawing is more difficult than withholding intensive care measures.
This may be secondary to increased emotional attachment as time
progresses. Proper understanding of this concept between parents and
clinicians, can lead to initiation of resuscitation in uncertain cases
with an option kept open to withdraw care if the situation warrants it.
In fact, the authors feel that such a pathway should be preferred
because with the passage of time a better clinical picture is formed to
base the decision.
Available Guidelines
The European Resuscitation Council 2015 guidelines
mention a variation of opinions regarding aggressive therapies in such
babies. Parents desire to participate in a larger manner in the decision
to resuscitate and continue life support. Local survival and outcome
data are essential to appropriately guide and counsel the parents [16].
The American Academy of Pediatrics/ American Health Academy’s 2015
resuscitation guidelines takes 25 weeks’ gestation as a cut-off point.
It cautions into considering various factors that can affect survival,
and using region-specific guidelines while counselling parents and
constructing a prognosis [17].
The 2017 consensus of American College of
Obstetricians and Gynecologists (ACOG) and Society of Maternal-Fetal
Medicine on Pre-viable birth recommends resuscitation from 24 0/7 weeks
onwards and considers resuscitation between 22 0/7 to 23 6/7 weeks
gestational age. Below 22 weeks, resuscitation is not recommended [18].
The guidelines further state that a stepwise approach considering
neonatal circumstances and parental wishes is appropriate. Care
decisions should be re-evaluated regularly and potentially redirected
based on the evolution of the clinical situation.
Clinicians also use certain tools to predict the
outcome of babies especially those in the grey zone. One of the most
commonly used models is the NICHD Neonatal Research Network tool that is
based on prospectively collected large data of extremely premature
infants [19]. There are some fallacies of such models. Most importantly,
gestational age, generally a key component in these models may not be
known accurately in all cases. The major problem by defining outcomes
based on completed weeks is that it eliminates the differences between a
fetus at 23 0/7 weeks and 23 6/7 weeks of gestation, as well as the
similarities between a fetus at 23 6/7 weeks and 24 0/7 weeks of
gestation. The inaccuracy of ultrasound-estimated fetal weight also
introduces a degree of uncertainty to the prediction of newborn outcomes
[18]. Lastly, the response of an individual neonate to resuscitation
cannot be predicted.
Thus, when a specific estimated probability for an
outcome is offered, it should be stated clearly that this is an estimate
for a population and not a prediction of a certain outcome for a
particular patient in a given institution.
Complexity of the Indian Scenario
In India, the scope and extent of medical services
ranges across a spectrum from poor healthcare to the best in the world.
In situations where appropriate care is not available, it would be
ethically correct that the parents should be given a choice to seek care
elsewhere.
The turmoil between ethics, logic and progress is
deep-rooted and intense in India. In addition to expenses being out of
pocket, we have cultural norms, which define who pays for first delivery
or second delivery, decisions to treat or not to treat are taken by an
extended family, the health care personnel are fewer in number and are
poorly trained in ethics as well as communication. Even proper
documented communication may be refuted by parents as we see in a
recently published paper from India [20]. In addition, India is a
cultural melting pot with multiple religions and sects with varying
approaches to births and deaths and often with gender preferences. In
such a scenario, making a blanket prescription for periviability is a
prescription for disaster.
There is an urgent need for a national consensus for
management of periviable babies and development of a database to collect
outcomes in this group. Analyzing the facts of neonatal survival,
morbidity and impact on families, we feel that each newborn should be
treated individually. The predefined gestational age limits should be
replaced with a more proactive approach. The neonatologist must develop
a personal approach towards decision-making.
1. Raju TN, Mercer BM, Burchfield DJ, Joseph GF Jr.
Periviable birth: executive summary of a joint workshop by the Eunice
Kennedy Shriver National Institute of Child Health and Human
Development, Society for Maternal- Fetal Medicine, American Academy of
Pediatrics, and American College of Obstetricians and Gynecologists.
Obstet Gynecol. 2014;123:1083-96.
2. Lubchenco LO, Searls DT, Brazie JV. Neonatal
mortality rate: relationship to birth weight and gestational age. J
Pediatr.1972;81:814-22.
3. Koops BL, Morgan LJ, Battaglia FC. Neonatal
mortality risk in relation to birth weight and gestational age: update.
J Pediatr.1982;101:969-77.
4. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook
AR, Walsh MC, et al. Eunice Kennedy Shriver National Institute of
Child Health and Human Development Neonatal Research Network. Neonatal
outcomes of extremely preterm infants from the NICHD Neonatal Research
Network. Pediatrics. 2010;126:443-56.
5. Costeloe KL, Hennessy EM, Haider S, Stacey F,
Marlow N, Draper ES. Short term outcomes after extreme preterm birth in
England: comparison of two birth cohorts in 1995 and 2006 (the EPICure
studies). BMJ. 2012;345:e7976.
6. Moore GP, Lemyre B, Barrowman N, Daboval T.
Neurodevelopmental outcomes at 4 to 8 years of children born at 22 to 25
weeks’ gestational age: A meta-analysis. JAMA Pediatr. 2013;167:967-74.
7. Bolisetty S, Legge N, Bajuk B, Lui K. Preterm
infant out- comes in New South Wales and the Australian Capital
Territory. New South Wales and the Australian Capital Territory Neonatal
Intensive Care Units’ Data Collection. J Paediatr Child Health.
2015;51:713-21.
8. Moore T, Hennessy EM, Myles J, Johnson SJ, Draper
ES, Costeloe KL, et al. Neurological and developmental out- come
in extremely preterm children born in England in 1995 and 2006: the
EPICure studies. BMJ. 2012;345:e7961.
9. Younge N, Goldstein RF, Bann CM, Hintz SR, Patel
RM, Smith PB, et al. Eunice Kennedy Shriver National Institute of
Child Health and Human Development Neonatal Research Network. Survival
and neurodevelopmental outcomes among periviable infants. N Engl J Med.
2017; 376:617-28.
10. Lee SK, Penner PL, Cox M. Comparison of the
attitudes of healthcare professionals and parents toward active
treatment of very low birth weight infants. Pediatrics.1991;88:110-4.
11. President’s Commission for the Study of Ethical
Problems in Medicine and Biomedical and Behavioral Research. Deciding to
Forego Life-Sustaining Treatment: A Report on the Ethical, Medical, and
Legal Issues in Treatment Decisions. Washington, DC: Government Printing
Office; 1983.
12. Singh J, Fanaroff J, Andrews B, et al.
Resuscitation in the "gray zone" of viability: Determining physician
preferences and predicting infant outcomes. Pediatrics. 2007;120:519-26.
13. Gillam L. The zone of parental discretion: An
ethical tool for dealing with disagreement between parents and doctors
about medical treatment for a child. Clin Ethics. 2016; 11:1-8.
14. Petteys AR, Goebel JR, Wallace JD, Singh-Carlson
S. Palliative care in neonatal intensive care, effects on parent stress
and satisfaction: a feasibility study. Am J Hosp Palliat Care.
2015;32:869-75.
15. Mercurio MR. The ethics of newborn resuscitation.
Semin Perinatol. 2009;33:354-63.
16. Wyllie J, Bruinenberg J, Roehr CC, Rüdiger M,
Trevisanuto D, Urlesberger B. European Resuscitation Council Guidelines
for Resuscitation 2015. Resuscitation. 2015;95:249-63.
17. Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS,
Kattwinkel J, Perlman JM, et al. Part 13: Neonatal Resus-citation:
2015 American Heart Association Guidelines Update for Cardiopulmonary
Resuscitation and Emergency Cardiovascular Care. Circulation.
2015;132:S543-60.
18. American College of Obstetricians and
Gynecologists; Society for Maternal-Fetal Medicine. Obstetric care
consensus No. 6: Periviable Birth. Obstet Gynecol. 2017;130:e187-e99.
19. Tyson JE, Parikh NA, Langer J, Green C, Higgins
RD. Intensive care for extreme prematurity - moving beyond gestational
age. N Engl J Med. 2008;358:1672e8.

