|
|
|
Indian Pediatr 2018;55:41-44 |
 |
Effect of Face-to-Face
Education on Anxiety and Pain in Children with Minor Extremity
Injuries Undergoing Outpatient Suturing in Emergency Department
|
|
Marzieh Beigom Bigdeli Shamloo 1,
Sahar Zonoori2,
Abbas Naboureh3,
Morteza Nasiri4,
Hadi Bahrami1,
Mohammad Maneiey1
and Fatemeh Allahyari Bayatiani1
From 1Department of Nursing, Nursing and
Midwifery faculty, Dezful University of Medical Sciences, Dezful, and
2Shahid Khoromi Hospital, Khorramabad; 3Department
of Critical Care Nursing, Nursing and Midwifery faculty, Tehran
University of Medical Sciences, Tehran; and 4Department of
Operating Room Technology, Paramedical School, Qom University of Medical
Sciences,
Qom; Iran.
Correspondence to: Morteza Nasiri, Department of
Operating Room Technology, Paramedical School, Qom University of Medical
Sciences, Qom, Iran.
Email:
mortezanasiri.or87@yahoo.com
Received: September 22, 2016;
Initial review: February 08, 2017;
Accepted: August 31, 2017.
Published online:
September 26, 2017.
Trial Registration: Iranian Registry of
Clinical Trials (IRCT2016020714930N4)
PII:S097475591600094
|
Objective: To assess the effect of face-to-face
education on anxiety and pain in children with minor extremity injuries
undergoing outpatient suturing. Methods: Children in intervention
and control groups received face-to-face education (10 minutes) and no
specific education, respectively. The anxiety and pain was measured
using Modified-Yale Preoperative Anxiety Scale, and pain by Faces Pain
Scale–Revised, respectively in 3 stages viz, pre-procedure and
pre-intervention, post-procedure. Results: Children in the
intervention group were less anxious than the control at pre-procedure
and post-intervention stage (41.1 (13.8) vs. 46.3 (19.1),
respectively, P=0.03) and post-procedure and post-intervention
stage (32.3 (17.2) vs. 40.2 (12.9), respectively, P=0.01).
Children in the intervention group experienced less pain than the
control at pre-procedure and post-intervention stage (3.9 (3.8) vs.
4.9 (3.1), respectively, P<0.001) and post-procedure and
post-intervention stage (3.1 (1.2) vs. 4.0 (2.1), respectively,
P=0.001). Conclusions: Face-to-face education could reduce
anxiety and pain in children undergoing suturing in the emergency
department.
Keywords: Intervention, Management,
Perioperative, Stress.
|
|
M
ost children undergoing outpatient procedures in
emergency department (ED) may experience anxiety and pain, which is
commonly managed unsatisfactorily [1,2]. The American Academy of
Pediatrics suggests that health care professionals create favorable
conditions for children to manage these two problems in the ED [3].
Face-to-face education has been shown to be effective
for management of adults’ anxiety and pain [4,5], but this education is
not provided routinely to children, particularly in the ED [6]. Due to
limited evidences on the efficacy of face-to-face education on anxiety
and pain in children, we assessed the effect of this education on
anxiety and pain in children undergoing suturing with local anesthesia
in the ED.
Methods
Children were eligible for inclusion if they had one
minor injury in upper or lower extremities, which occurred at least 1
hour and maximally 6 hours before admission, and had indication of
suturing with local anesthesia. Inclusion criteria were age 6-12 years,
lack of any sign of bone fractures, dislocation, amputation, presence of
a foreign body, nerve damage, fever and infection, presence of
children’s parents (either mother or father), lack of using sedative or
analgesic before the procedures, lack of developmental, physical or
psychological problems, not having previous hospitalization, ED
admission or outpatient procedures after 18 months of age, and lack of
long-term illness and/or pain that requires special medical care.
This study was approved by Ethic Review Board of
Dezful University of Medical Sciences (Khuzestan, Iran). Once a child
met the study inclusion criteria, a written informed consent was
obtained from the parents. Based on an earlier study [6], the sample
size was calculated as 39 subjects considering type I error of 5%, type
II error of 20%, and children’s anxiety as a key variable. Expecting a
10% dropout rate, we planned 43 subjects in each group. A Random
allocation software [7] was used by the first researcher assistant to
allocate children, who was the only person with access to the
randomization. Block randomization method was used to stratify children
into blocks based on injury sites (lower and upper extremities) and age
groups (6-9 and 9-12 years).
The primary outcome was anxiety, which was evaluated
with Modified-Yale Preoperative Anxiety Scale (M-YPAS) scoring from
23-100, with higher scores showing greater anxiety [6].
As secondary outcome, we used Faces Pain
Scale–Revised (FPS-R) to measure pain. FPS-R is on a metric scale of 0
to 10. Zero denoted no pain, and 10 denoted the most severe pain [8].
Scales were completed at three stages viz., pre-procedure and
pre-intervention (30 min before the procedure), pre-procedure and
post-intervention (immediately after the end of the intervention and 15
min before the procedure), and post-procedure (15 and 30 min after the
end of the procedure for M-YPAS and FPS-R, respectively).
Children in the control group received standard care
by hospital staff, while the intervention group received standard care
plus education. All educational interventions were provided in a
consultation room by the same research assistant on a one-to-one basis
for duration of 10 minutes, about 15 minutes before the procedure. Based
on children’s desire for perioperative information [9] and viewpoints of
an independent group of expert pediatric nurses and two anesthesia
consultants, the children were trained in a simple way about the ED
environment, family support, feeling of anxiety and pain (including
whether they would experience these, how long these would last, and how
bad these would be), and procedural information (time, potential
complications, anesthesia, and what to expect during and after the
procedure). In all cases, suturing and local anesthesia (with Lidocaine
2% using an insulin syringe) were performed by the same staff with the
same technique. During the procedure, parents in both groups were asked
to be present next to their child. The decision as to which parent would
accompany the child was left to them.
Statistical analysis: To examine group
differences, independent sample t-test and chi-square test were used for
quantitative and qualitative variables, respectively. Repeated measures
ANOVA were applied to assess variables over time. Statistical analysis
was done by SPSS software version 18 (SPSS, Inc. Chicago, IL, USA). P
value <0.05 was considered as significant.
Results
One hundred and ten children admitted to ED of Dezful
Ganjavian Hospital, Khuzestan, Iran, from December 20, 2015 through
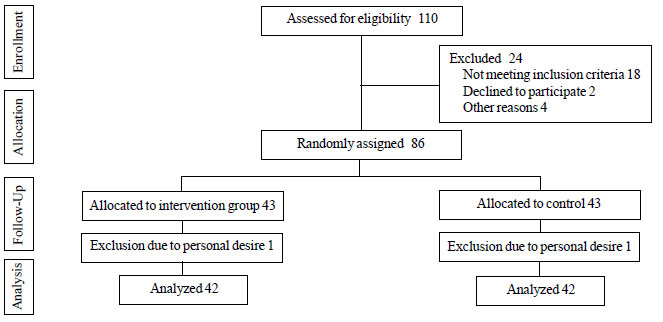
February 14, 2016, were recruited (Fig.1). Both groups
were not significantly different pertaining to demographic and clinical
characteristics (Table I).
 |
|
Fig. 1 Study flow chart.
|
TABLE I Characteristics of the Children Undergoing Outpatient Suturing (N=84)
|
Variables |
Intervention |
Control
|
|
(n=42) |
(n=42) |
|
Age (6-9 years); n (%) |
30 (71.3) |
28 (66.7) |
|
Gender (Male); n (%) |
28 (66.7) |
25 (59.5) |
|
Kind of parent (both mother |
18 (42.9) |
20 (47.6)
|
|
and father); n (%)
|
|
|
|
Site of injury and sutures, No. (%)
|
|
|
|
Upper extremity * (right) |
14 (33.4) |
14 (33.4) |
|
Lower extremity # (left) |
16 (38.1) |
17 (40.4) |
|
$Size of injury (cm2)
|
93.3 (4.2) |
89.6 (3.3) |
|
$Time spent in suturing (min)
|
8.1 (1.6) |
7.5 (1.2)
|
|
Kind of sutures, No. (%)
|
|
|
|
Simple interrupted
|
36 (85.7) |
33 (78.6) |
|
Simple vertical mattress (far and near) |
6 (14.3) |
9 (21.4) |
*Including finger, wrist, lower arm, elbow, and upper arm; #Including toe, foot, ankle, lower leg, knee, upper leg, and
lower trunk; P<0.05 for all comparison; $mean (SD).
|
Except in the first stage, in others stages children
in the intervention group experienced significantly lower anxiety and
pain. Both variables significantly differed between the two groups and
over time, and an interaction of time and group was observed (Table
II). Comparison of anxiety and pain during various stages is
shown in WebFig. 1.
TABLE II Comparison of Anxiety and Pain in the Intervention group (N=42) and Control Group (N=42)
|
Stages
|
Intervention
|
Control |
|
group
|
group |
|
Anxiety (M-YPAS), mean (SD) |
|
|
|
Pre-intervention (baseline) |
45.4 (16.7) |
47.6 (12.8) |
|
Post-intervention |
41.1 (13.8) |
46.3 (19.1) |
|
*Post-procedure
|
32.3 (17.2) |
40.2 (12.9) |
|
Pain (FPS-R), mean (SD) |
|
|
|
Pre-intervention (baseline) |
4.9 (0.2) |
5.1 (1.2) |
|
#Post-intervention |
3.9 (3.8) |
4.9 (3.1) |
|
$Post-procedure |
3.1 (1.2) |
4.0 (2.1) |
|
M-YPAS: Modified Yale Preoperative Anxiety Scale; FPS-R: Faces
Pain Scale–Revised; *P=0.001;#P<0.001; $P=0.011. |
Discussion
Children’s anxiety and pain were significantly lower
in the intervention group. We used a single-blind technique and only the
investigator was blinded, as it was not possible to blind the children,
parents, staffs and the educator nurse. However, to ensure that the
intervention would have no effect on the control group, preparation was
made separately for the groups and we asked nursing staffs to not
provide information for children and their parents. In the present
study, a homogenous sample of children aged 6-12 years was recruited.
Therefore it is not clear whether children below this age range can also
benefit from the intervention as younger children are more vulnerable to
anxiety and pain [10,11]. Moreover, all the data were collected in one
setting and only children undergoing outpatient suturing with local
anesthesia were included. This might limit the ability to generalize the
results.
Previous studies have either evaluated other
educational interventions, or have been conducted in the operating room
during general anesthesia [12,13]. Among children undergoing outpatient
surgical procedures under general anesthesia, it was shown that
preoperative education (simple explanations with a focus on separation
anxiety, reassurance, the use of dolls and positive behavior
reinforcement) reduced overall anxiety but group differences were not
significant, while education significantly reduced children’s
postoperative pain [12]. In another trial, it was demonstrated that
perioperative information and dialogue with children undergoing
outpatient surgical procedures requiring general anesthesia was
associated with significantly lower anxiety on the day of surgery and
postoperatively compared to control but no significant differences were
observed in pain scores [13]. The discrepancy may be due to differences
in the age of children, educational interventions, procedures,
anesthesia, and setting.
Based on our results, face-to-face education may be
effective for anxiety- and pain-reduction in children undergoing
outpatient suturing with local anesthesia. Further trials are
recommended in different settings, clinical procedures, and age-range to
extend this research.
Acknowledgments: Research Deputy vice-chancellor
for research affairs of Dezful University of Medical Sciences, Iran, for
technical support as well as valuable assistance.
Contributors: All authors contributed equally to
the concept, design, data collection, acquisition of data, analysis and
interpretation of data and drafting the manuscript. All authors read and
approved the study.
Funding: Dezful University of Medical Sciences,
Iran (grant number: DUMS.REC.1394.16).
Competing interests: None stated.
|
What This Study Adds?
•
Face-to-face education is
effective for pain-relief and anxiety-reduction in children
undergoing outpatient suturing in the emergency department.
|
References
1. Fortier MA, Kain ZN. Treating perioperative
anxiety and pain in children: A tailored and innovative approach.
Paediatr Anaesth. 2015;25:27-35.
2. Heilbrunn BR, Wittern RE, Lee JB, Pham PK,
Hamilton AH, Nager AL. Reducing anxiety in the pediatric emergency
department: A comparative trial. J Emerg Med. 2014;47:623-31.
3. Fein JA, Zempsky WT, Cravero JP. Committee on
Pediatric Emergency Medicine and Section on Anesthesiology and Pain
Medicine; American Academy of Pediatrics: Relief of Pain and Anxiety in
Pediatric Patients in Emergency Medical Systems. Pediatrics. 2012;130:
e1391-405.
4. Nkhoma K, Seymour J, Arthur A. An educational
intervention to reduce pain and improve pain management for Malawian
people living with HIV/AIDS and their family carers: A randomized
controlled trial. J Pain Symptom Manage. 2015;50:80-90.
5. Constantino RE, Braxter B, Ren D, Burroughs JD,
Doswell WM, Wu L, et al. Comparing online with face-to-face HELPP
intervention in women experiencing intimate partner violence. Issues
Ment Health Nurs. 2015;36:430-8.
6. Fortier MA, Bunzli E, Walthall J, Olshansky E,
Saadat H, Santistevan R, et al. Web-based tailored intervention
for preparation of parents and children for outpatient surgery (WebTIPS):
Formative evaluation and randomized controlled trial. Anesth Analg.
2015;120:915-22.
7. Saghaei M. Random allocation software for parallel
group randomized trials. BMC Med Res Methodol. 2004;4:26.
8. Hicks CL, Von Baeyer CL, Spafford PA, Van Korlaar
I, Goodenough B. The faces pain scale-revised: Toward a common metric in
pediatric pain measurement. Pain. 2001;93:173-83.
9. Fortier MA, Chorney JM, Rony RY, Perret-Karimi D,
Rinehart JB, Camilon FS, et al. Children’s desire for
perioperative information. Anesth Analg. 2009;109:1085-90.
10. Margolis JO, Ginsberg B, Dear GL, Ross AK, Goral
JE, Bailey AG. Paediatric preoperative teaching: Effects at induction
and postoperatively. Paediatr Anaesth. 1998;8:17-23.
11. Copanitsanou P, Valkeapää K. Effects of education
of paediatric patients undergoing elective surgical procedures on their
anxiety: A systematic review. J Clin Nurs. 2014;23:940-54.
12. Fincher W, Shaw J, Ramelet AS. The effectiveness
of a standardized preoperative preparation in reducing child and parent
anxiety: A single-blind randomised controlled trial. J Clin Nurs.
2012;21:946-55.
13. Wennström B, Törnhage CJ, Nasic S, Hedelin H,
Bergh I. The perioperative dialogue reduces postoperative stress in
children undergoing day surgery as confirmed by salivary cortisol.
Paediatr Anaesth. 2011;21:1058-65.
|
|
|
 |
|

