|
|
|
Indian Pediatr 2018;55: 27-30 |
 |
Nasal Continuous Positive Airway Pressure in
Bronchiolitis:
A Randomized Controlled Trial
|
|
Sandeep Narayan Lal, Jaspreet Kaur,
Pooja Anthwal,
Kanika Goyal,
Pinky Bahl and Jacob M Puliyel
From the Department of Pediatrics, St. Stephens Hospital, Tis Hazari,
Delhi, India.
Correspondence to: Dr Sandeep Narayan Lal, Department of Pediatrics,
St Stephens Hospital, Tis Hazari, Delhi 110054, India.
Email: sandeep.nlal@gmail.com
Received: October 28, 2016;
Initial review: February 14, 2017;
Accepted: September 09, 2017.
Published online: September 26, 2017
PII:S097475591600096
|
|
Objective: To evaluate the
efficacy of nasal continuous positive airway pressure (nCPAP) in
decreasing respiratory distress in bronchiolitis.
Design: Randomized controlled
trial.
Setting: Tertiary-care hospital
in New Delhi, India.
Participants: 72 infants (age
<1y) hospitalized with a clinical diagnosis of bronchiolitis were
randomized to receive standard care, or nCPAP in addition to standard
care, in the first hour after admission. 23 parents refused to give
consent for participation. 2 infants did not tolerate nCPAP.
Intervention: The outcome was
assessed after 60 minutes. If nCPAP was not tolerated or the distress
increased, the infant was switched to standard care. Analysis was done
on intention-to-treat basis.
Main outcome measures: Change in
respiratory rate, Silverman-Anderson score and a Modified Pediatric
Society of New Zealand Severity Score.
Results: 14 out of 32 in nCPAP
group and 5 out of 35 in standard care group had change in respiratory
rate ³10
(P=0.008). The mean (SD) change in respiratory rate [8.0 (5.8)
vs 5.1 (4.0), P=0.02] in Silverman-Anderson score [0.78
(0.87) vs 0.39 (0.73), P=0.029] and in Modified Pediatric
Society of New Zealand Severity Score [2.5 (3.01) vs. 1.08 (1.3), P=0.012]
were significantly different in the nCPAP and standard care groups,
respectively.
Conclusion: nCPAP helped reduce
respiratory distress significantly compared to standard care.
Keywords: nCPAP Ventilation,
Respiratory distress, Respiratory Syncytial Virus, Wheezing infant.
|
|
B
ronchiolitis is characterized by edema, mucus
secretions and damage of airway epithelium with necrosis, causing
airflow obstruction and distal air trapping, atelectasis and a
ventilation perfusion mismatch that leads to hypoxemia and increased
work of breathing [1,2].
Clinical improvement with significant falls in respiratory rate, pulse
rate and pressure of carbon dioxide (pCO2)
has been reported with the use of Continuous positive airway pressure
(CPAP) in Bronchiolitis [3,4]. In this study, we evaluated
whether CPAP is clinically beneficial in infants with moderate-to-severe
bronchiolitis during the first hour of treatment.
Methods
This randomized control trial was conducted at St.
Stephen’s Hospital (SSH), Delhi, between November 2014 and March 2016.
All patients who were hospitalized with a clinical diagnosis of acute
bronchiolitis were eligible for inclusion in the study. Bronchiolitis
was defined as respiratory distress (respiratory rate
³50/min) in an infant
aged 1 month to 1 year, along with wheezing on auscultation and
hyper-inflated lung. Infants who were in imminent need of ventilator
support were excluded.
Approval for the trial was obtained from the
hospital’s research ethics committee. Informed consent of the parents of
eligible children was obtained. Patients were then randomized to receive
CPAP or standard care. Randomization into the two groups was done in
blocks of 8 using computer software (www.randomization.com) seed
number 14184) and allocation to the groups was done using
sequentially-numbered opaque sealed envelopes. All patients received
standard care, which included maintenance of adequate hydration and
oxygenation, while the intervention group received bubble CPAP in
addition to the standard care. Bubble CPAP was delivered in the
pediatric ward with a Gregory circuit [5,6]. Oxygen saturation was noted
before starting treatment and oxygen was supplemented if the saturation
was <92%. Those in the intervention group received oxygen through the
bubble CPAP system while the standard care group received oxygen through
mask or hood. All children were monitored continuously during the study
period. The protocol mandated that CPAP would be stopped if the distress
of the patients increased (defined as increase in RR of more than 10),
or if the infant was very restless and not tolerating CPAP. If the
saturation fell below 90% in either group and persisted to be so for
more than >15 minutes despite oxygen supple-mentation, the child was
considered for mechanical ventilation. Treatment decisions were based on
the judgment of the treating physician but the changes made were
documented.
The respiratory rate (RR), Silverman-Anderson score,
and a Modified Pediatric Society of New Zealand severity score
(MPSNZ-SS) were assessed before starting treatment and at 1 hour
following the start of treatment. Respiratory rate was assessed by the
staff nurse on duty. The respiratory rate was counted for 60 seconds
continuously or in 2 blocks of 30 seconds. The Silverman-Anderson score
was assessed by the doctor on duty. The MPSNZ-SS was also assessed by
the doctor on duty based on the history and the clinical parameters. It
was evaluated by modifying the Pediatric Society of New Zealand (PSNZ)
severity scoring system that is based on six parameters (respiratory
rate, chest wall indrawing, nasal flaring or grunting, feeding, history
of behaviour, cyanosis) [7]. The original PSNZ guidelines used cyanosis
as a criteria but we substituted it with oxygen saturation. Each of
these parameters was assigned a score of 1 to 3 with increasing severity
and a final score was calculated.
The primary outcome was to compare the change in
respiratory rate after the first hour of treatment among the two groups.
A decrease in respiratory rate of 10 or more was considered clinically
significant difference. The secondary outcomes were the change in
Silverman-Anderson score and the MPSNZ-SS.
A previous study reported a 24% change in respiratory
rate (RR) in the study group compared to negligible change in the
standard care group [4]. For a type I error of 0.05 and a type II error
of 0.2, we calculated that a sample size of 72 was needed for a 1:1
ratio of standard care to CPAP.
Statistical analysis: Normality of data was
tested by Kolmogorov-Smirnov test. If the normality was rejected, non
parametric tests were used. Respiratory rate (RR) at admission, change
in respiratory rate after 1 hour of treatment ( DRR),
and modified Pediatric Society of New Zealand Severity Score (MPSNZ-SS)
at admission were normally distributed and were compared using
independent T test and non-parametric data as age in months, RR at the
end of 1 hour, Silverman-Anderson (SA) score, MPSNZ-SS at the end of 1
hour, and the change in MPSNZ-SS (DMPSNZ-SS)
were compared using Mann-Whitney test between two groups. Change in RR (DRR
<10 and ³10)
was compared using chi square test between the two groups. Wilcoxon
ranked sum test was used to compare RR, SA Score and MPSNZ-SS within
groups across follow-up.
Results
The study was continued till 72 patients were
recruited. A total of 117 children were hospitalized with a provisional
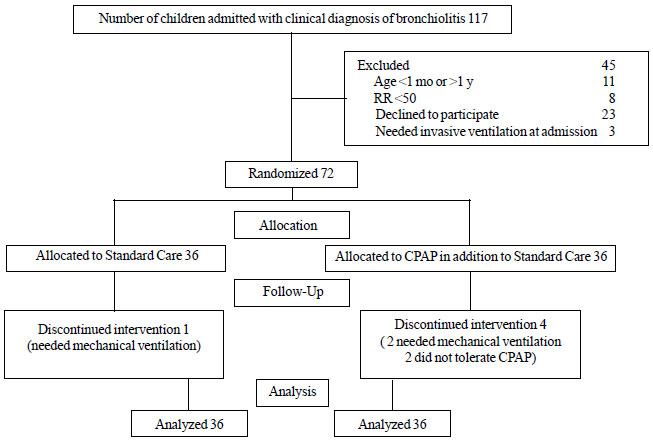
diagnosis of bronchiolitis during this period. Fig. 1
depicts the flow of participants in the study.
 |
|
Fig. 1: Study flow chart.
|
The baseline characteristics of the two groups are
described in Table I. There was no significant difference
between the two groups. Table II shows the mean change in
respiratory rate, Silverman-Anderson score and MPSNZ-SS in the two
groups after 1 hour of treatment. There was statistically significant
improvement in RR, SA score and MPSNZ-SS in the bubble CPAP group when
compared to standard care group.
TABLE I Baseline Characteristics in the Study Groups
|
Characteristics |
Bubble CPAP
|
Standard care |
P value
|
|
group (n= 36) |
group (n=36) |
|
|
Age (mo) |
4.0 (2.6)
|
4.7 (3.1)
|
0.36 |
|
Male gender, No. (%) |
26 (72.2) |
28 (77.8) |
0.59 |
|
Respiratory rate |
70 (11) |
67 (7) |
0.17 |
|
SA score
|
4.2 (2.1)
|
3.8 (1.7)
|
0.74 |
|
MPSNZ-SS |
12.4 (2.7)
|
11.7 (2.4)
|
0.21 |
|
SA: Silverman Anderson; MPSNZ-SS: Modified Pediatric Society of
New Zealand Severity Score; All values in mean (SD).
|
In the bubble CPAP group, 14 out of 32 patients
showed clinically significant improvement ( DRR
³10), whereas
5 out of 35 patients had clinically significant improvement in the
standard care group (P=0.008). Three patients needed mechanical
ventilation within 1 hour of starting treatment as the distress
progressively worsened. Of these, two were from the CPAP group and one
was from standard treatment group. CPAP had to be stopped in two
children before 1 hour, as they were very restless and became more
agitated following start of CPAP. Table II compares the
outcomes between two groups.
TABLE II Comparison of Change in Respiratory Distress in the Two Groups After 1 Hour
|
Parameter |
Bubble CPAP |
Standard care |
P value |
|
Respiratory rate
|
8 (6) |
5 (4) |
0.02 |
|
SA score |
0.78 (0.87)
|
0.39 (0.73)
|
0.03 |
|
MPSNZ-SS |
2.5 (3.0)
|
1.1 (1.3)
|
0.01 |
|
SA:Silverman-Anderson; MPSNZ-SS: Modified Pediatric Society
of New Zealand Severity Score; All values in mean (SD). |
Discussion
In this randomized controlled trial, we documented
that CPAP significantly reduced the respiratory rate in comparison to
standard care in infants with bronchiolitis. The Silverman-Anderson
score and MPSNZ-SS also showed significant improvement with CPAP during
the first hour of treatment.
Bronchiolitis is a clinical diagnosis with limited
role of laboratory and radiological evaluation [1,8]. We included all
infants during the bronchiolitis season with respiratory distress and a
respiratory rate ³50,
at the time of admission. As pneumonia is also common in this age group
and it also presents with similar symptoms initially, it is possible
that few patients included in the study were cases of pneumonia. Ours
was an open label study and could have been influenced by observer bias.
Patient parameters were assessed by the doctors and nurses on duty who
were aware of the intervention, and that may have resulted in assessment
bias. Though our study was continued for an hour, in children who
benefited from CPAP, this was continued beyond 1 hour, till the
clinician decided that CPAP was no longer necessary. Exact data on
duration of CPAP was not collected as it was not part of the protocol.
We evaluated the respiratory rate only for the first hour; functional
outcome such as need for invasive ventilation and duration of hospital
stay were not evaluated.
The magnitude of change in the mean RR in our study
was much less than that seen in a study from Ghana [4], where children
(age 3 months to 5 years) with respiratory distress (including asthma
and pneumonia) were treated with CPAP. Among studies that evaluated at
the role of CPAP in bronchiolitis, Milesi, et al. [9] found that
the use of CPAP decreased inspiratory work in young infants with
bronchiolitis. Thia, et al. [10] studied the effect of CPAP on
change in partial pressure of CO 2
(pCO2) in children with
bronchiolitis, and observed a significant reduction in pCO2
with use of CPAP when compared to standard care. Machen, et al.
[11] also studied the role of CPAP in infants and children with
respiratory distress, and documented that CPAP was most beneficial for
infants with bronchiolitis. However, a Cochrane review suggests that
effect of CPAP in children with bronchiolitis is uncertain and larger
trials with adequate power are required to further evaluate it [12].
The mechanism by which CPAP works in bronchiolitis is
likely to be multifactorial. CPAP works by keeping the airways open,
increasing clearance of secretion and improving gas exchange [13,14].
Although CPAP has been associated with adverse effects such as nasal
mucosal damage, mucosal excoriation, scarring, pressure necrosis,
pneumothorax and a decrease in cardiac output [12], none of the patients
included in our study had any significant adverse effect.
Our study suggests that CPAP significantly decreases
the respiratory rate in patients of acute bronchiolitis in the first
hour of treatment. Trials are needed to further investigate if CPAP
could be of value in decreasing need of invasive mechanical ventilation
and the total duration of hospital stay in children with bronchiolitis.
Contributors: Study was conceived by JP, PB and
SNL. The data were collected and analyzed by SNL, JK, PA, KG. The first
draft was written by SNL and JP; all the authors approved the final
draft.
Funding: None; Competing interest: None
stated.
|
What is Already Known?
•
CPAP decreases respiratory rate
in children with respiratory distress of varied etiology.
What This Study Adds?
•
CPAP is useful in reducing respiratory rate in hospitalized
children with bronchiolitis.
|
References
1. Ralston SL, Lieberthal AS, Meissner HC, Alverson
BK, Baley JE, Gadomski AM, et al. Clinical practice guideline:
the diagnosis, management, and prevention of bronchiolitis. Pediatrics.
2014;134:e1474-502.
2. Oymar K, Skjerven HO, Mikalsen IB. Acute
bronchiolitis in infants, a review. Scand J Trauma Resusc Emerg Med.
2014;22:3.
3. Beasley JM, Jones SE. Continuous positive airway
pressure in bronchiolitis. Br Med J (Clin Res Ed). 1981;283:1506-8.
4. Wilson PT, Morris MC, Biagas KV, Otupiri E,
Moresky RT. A randomized clinical trial evaluating nasal continuous
positive airway pressure for acute respiratory distress in a developing
country. J Pediatr. 2013;162: 988-92.
5. Gregory GA, Kitterman JA, Phibbs RH, Tooley WH,
Hamilton WK. Treatment of the idiopathic respiratory-distress syndrome
with continuous positive airway pressure. N Engl J Med.
1971;284:1333-40.
6. Kaur C, Sema A, Beri RS, Puliyel JM. A simple
circuit to deliver bubbling CPAP. Indian Pediatr. 2008;45:312-4.
7. Paediatric Society of New Zealand. 2005. Best
Practice Evidenced Based Guidelines. Wheeze and Chest Infection In
Infants Under 1 Year. Available from: http://www.
paediatrics.org.nz/files/guidelines/Wheezeendorsed. pdf. Accessed
February 22, 2017.
8. Verma N, Lodha R, Kabra SK. Recent advances in
management of bronchiolitis. Indian Pediatr. 2013;50: 939-49.
9. Milesi C, Matecki S, Jaber S, Mura T, Jacquot A,
Pidoux O, et al. 6 cmH2O continuous positive airway pressure
versus conventional oxygen therapy in severe viral bronchiolitis: A
randomized trial. Pediatr Pulmonol. 2013;48:45-51.
10. Thia LP, McKenzie SA, Blyth TP, Minasian CC,
Kozlowska WJ, Carr SB. Randomised controlled trial of nasal continuous
positive airways pressure (CPAP) in bronchiolitis. Arch Dis Child.
2008;93:45-7.
11. Machen HE, Mwanza ZV, Brown JK, Kawaza KM,
Newberry L, Richards-Kortum RR, et al. Outcomes of patients with
respiratory distress treated with bubble CPAP on a pediatric ward in
Malawi. J Trop Pediatr. 2015;61:421-7.
12. Jat KR, Mathew JL. Continuous positive airway
pressure (CPAP) for acute bronchiolitis in children. Cochrane Database
Syst Rev. 2015;1:CD010473.
13. Oymar K, Bardsen K. Continuous positive airway
pressure for bronchiolitis in a general paediatric ward; a feasibility
study. BMC Pediatr. 2014;14:122.
14. Essouri S, Durand P, Chevret L, Balu L, Devictor
D, Fauroux B, et al. Optimal level of nasal continuous positive
airway pressure in severe viral bronchiolitis. Intensive Care Med.
2011;37:2002-7.
|
|
|
 |
|

