|
|
|
Indian Pediatr 2017;54: 37-45 |
 |
Teaching for Reducing Diagnostic Errors
|
|
*Devendra Mishra, #Piyush
Gupta and Tejinder Singh
From Departments of Pediatrics, *Maulana Azad Medical
College,and #University College of Medical Sciences, New
Delhi; and Christian Medical College, Ludhiana, Punjab; India.
Correspondence to: Dr Tejinder Singh, Department of
Pediatrics and Medical Education, Christian Medical College, Ludhiana
141 008, India.
Email: [email protected]
|
|
Diagnostic errors, constituted by a
missed, wrong, or delayed diagnosis detected later by additional tests
or findings, are one of the most vexing issues in medicine. They are one
of the commonest causes of patient-harm and also medical negligence
claims. Although a variety of constructs have been proposed to explain
diagnostic errors, the complex interplay of cognitive- and
system-factors that underlie these errors is rarely clear to the
clinicians. In this write-up, we discuss the reasons for diagnostic
errors and how medical students can be trained to avoid such errors. The
errors have been classified as Cognitive errors, System errors, and
No-fault errors, and cognitive interventions to address each of these
are detailed.
Key words: Clinical reasoning; Cognitive
errors; Diagnosis; Misdiagnosis-related harm.
|
|
O
ne of the most challenging and
stimulating
tasks of a clinician is to arrive at a diagnosis.
The diagnosis, for all practical purposes, is
usually a working hypothesis to decide the management of the patient
[1]. Medical diagnosis is the crux of the clinical encounter between the
doctor and the patient, and is the cornerstone of most of the management
decisions, and thereby, patient-satisfaction. However, medical diagnosis
is not always a yes-or-no situation, especially at the initial
consultation. It is a complex process involving many independent and
inter-dependent variables that are difficult to tease out and enumerate
completely. Arriving at a definitive diagnosis may require some or all
of a characteristic thinking process, additional history-taking or
examination, and further investigations or consultations. The Medical
Council of India Vision 2015 document, although not specifically
mentioning diagnostic errors, does stress on the diagnostic skills as
one of the competencies required for the Indian Medical Graduate [2].
Diagnostic Errors
What are Diagnostic Errors?
Diagnostic errors, defined as a diagnosis that is
missed, wrong, or delayed, as detected by some subsequent definitive
test or finding [3], are gradually receiving significant attention from
researchers and the authorities. The US Institute of Medicine Committee
on Diagnostic Error in Health Care has recently defined diagnostic error
as "the failure to (a) establish an accurate and timely
explanation of the patient’s health problem(s) or (b) communicate
that explanation to the patient" [4]. On the other hand, harm due to
diagnostic errors i.e., misdiagnosis-related harm, can be defined
as ‘preventable harm that results from the delay or failure to treat a
condition actually present (when the working diagnosis was wrong or
unknown) or from treatment provided for a condition not actually
present’ [5]. With the introduction of Consumer Protection Act, and the
increasing frequency of litigations related to wrong diagnosis or
treatment, there is a need for training clinicians to reduce such
errors.
Why these errors occur and how to reduce them is a
hotly debated issue. It has been suggested that the focus of clinical
teaching is mostly on ‘diagnosis’, and not as much on ‘misdiagnosis’ or
errors of diagnosis and ways to avoid them. The elucidation of various
theories on the cognitive process behind decision-making, and
recognition of variety of ways to teach clinical reasoning to students
have now enabled us to address the cognitive aspects of diagnostic
reasoning [6]. Various mechanisms for reducing diagnostic errors [7,8],
and teaching and assessing reduction of diagnostic errors [8,9] have
been suggested. Electronic decision-support website or mobile
applications (Apps) [10,11], written case-scenarios for teaching
diagnostic errors, electronic trigger tools (electronic algorithms that
identify potential adverse events by searching electronic health records
and flagging specific occurrences) [12,13], simulated patients [14] etc.
are increasingly being used as strategies to teach about and reduce
diagnostic errors.
How common are They?
Although exact prevalence data are not available, and
diagnostic errors are difficult to document reliably, these have been
estimated to be in the range of 5-15% [15,16]. In a survey of 726
pediatricians, more than half had made a diagnostic error at least once-
or twice-a-month (the frequency was 77% among trainees); and nearly half
reported diagnostic errors that harmed patients at least once- or
twice-a-year [17]. Data from other countries also shows similar trends
[18-21]. Incidence of medical errors in India is not documented, but
probably these occur frequently [22]; however, they are usually
under-reported, overlooked and remain a controversial area [23].
In addition to being highly prevalent, diagnostic
errors also have important implications for both the patients and the
physicians. Diagnostic errors are important causes of both adverse
events (second largest cause) [24] and also malpractice suits against
hospitals (second leading cause) [25]. Diagnostic discrepancy has been
noted even in 20% cases of autopsy [26]. They may also cause harm to
patients by inappropriate treatment, delayed treatment, or even harmful
treatment. In addition, they may have psychological or financial
repercussions, and lead to medical malpractice claims [4]. There is thus
an urgent need to teach students to address and respond to diagnostic
errors, and by extension, overall improvement in diagnosis.
Factors Contributing to Diagnostic Errors
Before we address the various mechanisms to teach
reduction of diagnostic errors, two issues need to be deliberated upon
viz., how physicians make diagnosis, and what are the causes of
diagnostic errors?
How Physicians Make Diagnosis?
The skills required during a clinical encounter,
including history-taking, physical-examination, synthesizing data, and
presenting this information, represent an amalgamation of multiple
cognitive and psychomotor skills and behaviors. The Dual Processing
theory is one of the widely accepted theories and proposes that
clinicians use two types of cognitive processes to arrive at a
diagnosis; System I and System II approaches [27]. System I approaches
are faster, more intuitive and based on past experience and
pattern-recognition, whereas system II approaches are analytical and
more deliberate [6]. A beginner primarily uses system II approach;
whereas experts primarily use the system I approach, though they may
switch between the approaches depending upon the complexity of the case
[28]. Further details of these processes have been previously published
[6].
Clinicians routinely use a lot of thumb-rules or
heuristics, whether explicitly stated or self-developed [29]. Although,
these are essential if multiple critical decisions need to be made in a
situation of constraints of time and information, a corollary of this
process is a fixed proportion of error, due to inherent biases
associated with each of these heuristics [30]. The principle that it is
more likely for a single disease to explain multiple symptoms than for
multiple diseases to occur, is called as the Occham’s razor [31].
Although infrequently acknowledged, this is one of the most frequently
relied upon argument for verifying a diagnosis. This is also accompanied
frequently by the tendency to be biased by our initial hypothesis and
thus paying minimal attention to other possibilities, also called as
Premature closure [32]. This may sometimes just be due to
overconfidence, but may occasionally be due to confirmation bias - a
tendency to favor evidence that confirms our hypothesis than evidence
favoring alternate diagnosis [30]. Clinicians frequently use diagnostic
tests to rule-in or rule-out clinical diagnosis, but mostly intuitively,
without using an objective method. Bayes’ theorem is a method [33] to
modify the probability of a particular diagnosis after the results of a
diagnostic test. However, it is infrequently used in clinical practice,
despite the information on pre- and post-test probability being
available for many of the tests in use. Although infrequently taught, in
practice, physicians use system I processes more often.
The deliberate diagnostic process consists of four
sequential activities, which sometimes occur so rapidly in experienced
clinicians so as to appear as if occurring simultaneously [30]. These
include the initial recognition of the abnormal data, abnormal physical
findings or radiological abnormalities (Perception); followed by
generation of a clinical framework for analysis or a list of highly
likely diagnosis (Hypothesis-generation). These initial diagnoses
are then evaluated in the light of available test results (Data-interpretation).
This is then followed by the confirmation of the working diagnosis (Verification).
There are a variety of steps in this cognitive process of diagnosis,
problems in either of which may lead to diagnostic errors.
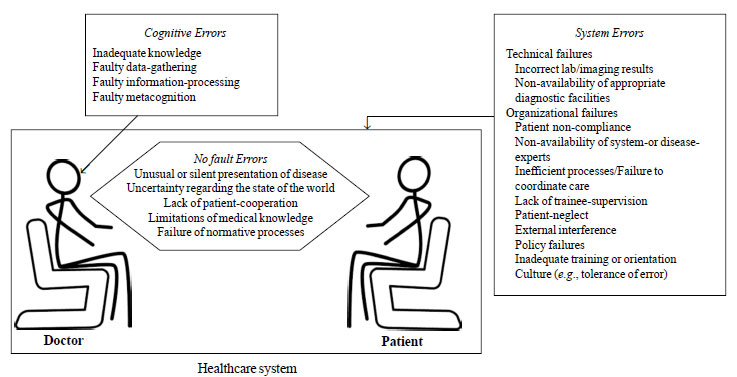
Causes of Diagnostic Errors
Diagnostic errors have been categorized as No-fault
errors, System errors, and Cognitive errors. A schematic representation
of these categories, with various examples [30] is shown in Fig.
1. Due to its etiological underpinnings, this is an important
differentiation as it also guides us towards preventive strategies to
address each group. We also need to appreciate that in addition to
multiple system errors, cognitive factors may co-exist, and an
interaction between the two may be at the root of many cases of
diagnostic errors [34]. Errors have been reported to be more likely to
occur when the level of uncertainty is high, there is unfamiliarity with
the patient, there are co-morbid disorders confusing the clinical
picture, and if atypical or non-specific manifestations are the
presenting feature [35].
 |
|
Fig. 1 Three types of diagnostic
errors in the healthcare system.
|
No-fault errors: These are cases where due to the
unique illness- or patient-characteristics, making the correct diagnosis
with the current state of medical knowledge is not likely to be routine
[35,36]. This may be due to a rare disease, an atypical presentation, a
non-compliant patient, and a new disease or an as yet unrecognized
manifestation.
System errors, on the other hand, can be ascribed
to the deficient functioning of the healthcare system, rather than on
the patient-doctor interaction. These reflect latent flaws in the system
[30], whether they are due to technical failure or failure of the
organizational policies and protocols. These range from those affecting
the individual diagnostician e.g., stress or workload, to those
affecting all beneficiaries/stakeholders of that system e.g.,
defective communication and weak policies.
Cognitive errors: are those in which the problem
is with the individual diagnostician and include inadequate knowledge or
faulty data-gathering, inaccurate clinical reasoning, or faulty
verification [9,35,36].
Teaching to Reduce Diagnostic Errors
Although many complex constructs to explain
diagnostic errors exist, most clinicians are unaware of the cognitive
and system-based underpinnings of this phenomenon [7]. Whether some or
all diagnostic errors can be prevented is not known presently, with
experts even questioning the goal of zero diagnostic errors [30]. Still,
it stands to reason that all attempts should be made to increase
diagnostic reliability and decrease diagnostic errors. An expert
committee of the Institute of Medicine in US has outlined eight goals to
reduce diagnostic errors and improve diagnosis [4]. Two of these are
primarily focused on teaching-learning activities viz., "Enhance
health care professional education and training in the diagnostic
process" and "Research on the diagnostic process and diagnostic error";
in addition to the process of reflection addressed by the goal: "Develop
and deploy approaches to identify, learn from, and reduce diagnostic
errors and near missed in clinical practice" [4].
One major problem with addressing diagnostic errors
is the multiplicity of the underlying factors; an average of six
contributory factors per error were identified in an internal medicine
department, with almost two-third being system-related ones [34].
Strategies to reduce diagnostic errors may focus on two inter-related
aspects viz., Educational activities (teaching–learning
activities to teach avoidance of diagnostic errors), and System-related
or Managerial strategies, which can be used in practice to address some
aspects of diagnostic errors. In this communication, the focus would be
on the educational interventions to reduce diagnostic errors.
Educational interventions can be used to address both system-related and
cognitive root causes [36,37]. Although, it may appear intuitive that
only cognitive errors would be amenable to teaching-learning strategies
and it may not be possible to address system-errors, educational
strategies have been suggested for both. Cognitive interventions to
reduce diagnostic errors have been classified into three mutually
exclusive categories by some experts [36-38]: (a) Interventions
to increase clinicians’ knowledge and experience; (b)
Interventions to improve clinical reasoning and decision-making skills;
and (c) interventions that assist clinicians with tools or access
to other clinicians or experts.
Education for Reducing Cognitive Errors
Two educational strategies have been suggested for
reducing diagnostic errors viz., efforts to directly improve
cognition, and an indirect system-related approach. However, we need to
be aware that cognitive shortcomings can always undermine potential
improvements from system changes, and thus educational efforts to
directly improve cognition are the lynchpins for reducing diagnostic
errors. Moreover, cognitive shortcomings play a dominant role in
contributing to diagnostic error [36-38], and thus need to be primarily
addressed.
Directly improving cognition
The primary responsibility for training and teaching
the diagnostic process and provide more opportunities for learning the
same, is on medical colleges and clinical departments, so as to develop
highly competent diagnosticians [36,37].
Although the normative approach to diagnosis
(consisting sequentially of differential diagnosis, narrowing to a
limited number possibilities, and Bayesian probability evaluation) is
diligently taught and re-taught in medical school, it is infrequently
used in clinical practice, and in fact may not work if the case is just
too complicated [37-40]. The current paradigm of the diagnostic process
by a knowledgeable and experienced physician is called as dual-process
model, part automatic and part conscious [36-40]. The system 1 or the
subconscious, rapidly acting automatic system solves the common
problems; whereas, the conscious, rational and analytical cognition
(System II) comes into play when problems are complicated and not
amenable to automatic decision-making, and also to check on the
solutions to the easy problems. This process of diagnosis needs to be
taught to trainees so that they know what are its shortcomings and ways
to overcome these. The traditional model of medical education aiming for
initial building up of the basic sciences theoretical knowledge,
followed by clinical exposure and application of the knowledge, has been
replaced completely by a Problem-based learning curriculum, where all
teaching-learning activities are in the setting of a clinical problem
[40,41].
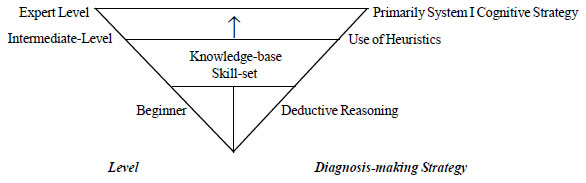
A framework for considering educational interventions
for reducing diagnostic errors has been suggested by Graber [36,37],
wherein the diagnostician progresses from the basic level (using
deductive reasoning) to intermediate level (using heuristics) to expert
level skills, with increasing reliability and accuracy, in addition to
decreased cost and effort (Fig. 2). Two possible
educational strategies have been suggested based on this framework
viz., by improving expertise, and by conscious, reflective review.
As Croskerry [38-42] has suggested, this allows a cross-check of the
solutions provided by the subconscious, System I.
 |
|
Fig. 2 An inverted pyramid model of
diagnostic proficiency.
|
Enhancing expertise is the apparently easier
strategy to improve the diagnostic reliability and thereby reduce
diagnostic errors. Students need to be trained for being better thinkers
by teaching discriminative skills and providing more examples and
repetitions. This improves their clinical-decision making skills.
However, it needs long-term sustained efforts, changes in the
educational curriculum, and application over the whole duration of the
course.
A satisfactory skill-set coupled with an adequate
knowledge base gives the ability to recognize patterns in disease
presentations and make reliable diagnoses [42,43]. For the
undergraduates, it will primarily involve acquiring knowledge and the
skills required to apply this for diagnosis i.e., history-taking
and examination skills. It has been the experience of many, and also
published literature [43,44], that these skills are infrequently
achieved. Failure to gather information through history, physical
examination or chart-review was the most common system factor reported,
according to a physician survey in US [17]. Although postgraduates
already have a wide range of competencies, still further development is
possible, though difficult. It requires extensive practice combined with
formative feedback [36,37]. We need to recognize these principles and
use the opportunity to teach superior diagnostic skills through
opportunities to practice on a wide-range of diseases with all their
spectrum of presentations – definitely a tall order in the limited
period residents are in training. Simulated patients [44,45], especially
for uncommon diseases or unusual presentations, may be helpful in this
regard.
Encouraging sub (or so-called ‘super’)-specialization
is another way to make available expert diagnosticians to diagnose
diseases in a focused filed, as their knowledge-base and skill set are
still higher. However, in the absence of a trained person making an
initial diagnosis and referring correctly to the appropriate specialist,
and given the unequal distribution of expertise in our scenario,
ensuring access to primary-care by a basic doctor may be a better goal
than this approach.
Conscious reflective review: In the short term,
conscious reflective review may gainfully be employed to improve
clinical diagnosis and reduce diagnostic errors. The subconscious
problem-solving, utilized to make diagnosis in a large number of cases,
is characterized by automatic actions [38-40]. For effective use of
reflections, the user needs to be taught and made aware of these and
other pitfalls in the diagnostic process, though the benefits of
reflections for improving diagnosis have also been questioned [45-48].
Students must be encouraged and provided an
opportunity to reflect on their diagnostic approach, and think about
what they could be missing. Morbidity and mortality conferences are a
good place to do this [6]. Residents can be asked to reflect on their
delivery of patient care based on actual case records (case based
discussions) or on the discharge papers of patients (chart-stimulated
recall) [6].
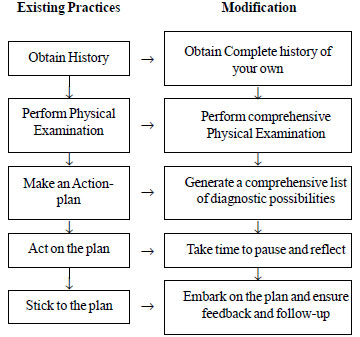
Use of a checklist to have a review of the diagnostic
process and ensure a feedback loop has been suggested [36,37]. Using a
checklist has a long history in other high-pressure multiple
decision-making settings like aviation, and can be used to benefit the
process of diagnosis. A checklist ensures that no step is overlooked and
the same steps are followed by all team members; one with an inbuilt
feedback loop has been suggested recently [36, 37, 48,49]. The same has
also been detailed in Fig. 1.
Metacognitive training: Metacognition, the
ability of being aware of one’s thinking process, is apparently a unique
human ability. One of the applications of this process is active
open-mindedness, and has been shown to lead to ‘better’ decisions [30].
Training strategies for the same have been described and can be used to
improve the cognitive process for diagnosis-making.
To incorporate these principles in to day-to-day
clinical teaching, clinical case-presentations and case-based
discussions are important opportunities. Structured case presentation
models like SNAPPS (Summarize the case, Narrow the differentials,
Analyze the differentials, Probe the preceptor about uncertainties, Plan
management for the patient, Select case related issues for self-study)
and One-Minute Preceptor (OMP) provide opportunities to get knowledge,
probe students’ reasoning and provide opinion [6]. The opportunity to
describe one’s clinical reasoning and being guided to the correct
diagnosis provides important insight to the students regarding the
diagnosis-making process. Such a metacognitive approach may help
learners to recognize the need to slow down and avoid errors that occur
due to premature closure of reasoning [49].
System-related approach
Majority of these inputs are administrative in nature
and have only a small educational component.
Clinical Guidelines and Clinical decision-support
systems: Clinical guidelines, and their extension, clinical
decision-support systems, are likely to be helpful in reducing
diagnostic errors [36,37]. Guidelines, if developed by considering
appropriate prevalence rates and probability estimates, with efforts to
minimize errors due to heuristics, may help to improve diagnosis in the
clinical setting [50,51]. The problems with clinical guidelines are
many, including clinicians being unaware of their existence or unwilling
to follow them, not being available to all levels of healthcare, and
quite a few of these themselves being heuristic in nature. Teaching
about the evidence-based medicine, and consensus-building for
synthesizing research evidence to generate guidelines will help in
ensuring development of clinically relevant guidelines that are
widely-accepted. Guidelines have in fact, been shown to be ineffective
in reducing diagnostic errors, though effective in reducing errors in
treatment and preventive settings [51,52].
 |
|
Fig. 3 Steps in improving the
reliability of diagnosis (developed from Graber, 2009 [24]).
|
Use of technology in health-management and patient
care, the so called Health-information technology (HIT) approaches, are
one of the most rapidly expanding areas in the field of patient-safety.
These tools and algorithms can be characterized as those assisting: (i)
information gathering; (ii) information organization and display;
(iii) differential diagnosis generation; (iv) weighing of
diagnoses; (v) generation of diagnostic plan; (vi) access
to diagnostic reference information; (vii) facilitating
follow-up; (viii) screening for early detection in asymptomatic
patients; (ix) collaborative diagnosis; and (x)
facilitating diagnostic feedback to clinicians [52,53]. Recognizing the
importance of information technology for the doctor of today, the
General Medical Council in UK advocates that medical graduates should be
able to "make effective use of computers and other information systems,
including storing and retrieving information" [53], something which the
MCI document overlooks [2]. A recent systematic review showed that HIT
is efficacious in improving quality and efficiency of medical care [54];
though, electronic health records and electronic decision-support
systems were the two of the HIT modalities most commonly used. There is
an urgent need to incorporate these in the health management system, and
train students in their appropriate use for a patient-centric
healthcare.
Clinical decision-support systems directly
incorporate computer-based decision system into the clinical practice of
medicine at the bedside. These are gradually being used more widely, but
the evidence of efficacy for clinical diagnosis is sketchy, though they
have been shown to improve patient outcomes and provider behavior
related to drug-dosing, preventive care and general process of care
[54,55]. One reason for this could be the poor quality of input into the
system [30], thereby limiting the functionality of the system, which
could either be due to time constraints preventing complete input of
data, or biased data due to the initial hypothesis being considered, or
sufficient input data has not been collected.
Improving perception: The method of presenting
data has a major impact on our ability to pick up abnormalities [30].
Presenting data in such a way that abnormal findings stand out e.g.,
highlighting (or using bold typeface) the abnormal results in a report,
and presentation as graphs/figures may be more helpful in identifying an
abnormal result from a series of normal results. SMS-based or other
app-based reminders for abnormal results or need for follow-up a patient
may also reduce diagnostic errors.
Expert-opinion: Non-availability of appropriate
experts is a recognized reason for missed findings leading to diagnostic
errors [55,56], and has been reported even from emergency-rooms in
developed countries. It is likely to be more common in the developing
country scenario. Although more training may appear a low-cost and
direct method, its sustainability is questionable. As far as the
educational aspects are considered, improved supervision of trainees
[30] and posting of residents of varying seniority together are ways of
making expert-opinion available on call, and possibly reducing
diagnostic errors.
An extension of this approach, especially in
non-urgent situations will be the concept of second opinion. These have
been proven effective in decreasing medication errors and can also
gainfully be utilized in diagnostic errors whether for diagnostic tests
or for complex or difficult clinical diagnoses [57,58].
Education for Reducing System Errors
Given that system errors affect all persons and
activities concerned with patient-care, addressing these is likely to
reduce diagnostic errors for all diagnosticians working in the system,
and also have a long-term effect [30].
A major educational strategy for system-related
errors could be addressing communication-related deficits including
communication between patient and healthcare personnel, and between
various members of the healthcare team (among physicians, between
physicians and other team members). This should also address the process
of handing- and taking-over of patients’ records at the time of shift
changes (‘handoffs’ or ‘sign-outs’), an issue that is especially
relevant in the current scenario of restricted work hours of residents
[59,60]. Improper handoffs may lead to insufficient clinical or
test-related information being communicated, which may lead to increased
opportunity for diagnostic errors [59].
Improvements in verbal and written communication
between health care providers during patient handoffs can reduce
injuries due to medical errors by up to 30 percent [61]. A study on a
system of bundled communication and training tools for handoff of
patient care between providers significantly increased patient safety
without significantly burdening existing clinical workflows. Moreover,
physicians in a study ranked access to electronic health records and
following up with patients as effective strategies in preventing
diagnostic errors [17].
There is ample evidence to demonstrate that
communication skills can be increased through directed training [62];
thus making these a promising target for educational interventions.
However, the current Attitudes and Communications (ATCOM) module of MCI
is focusing primarily at doctor-patient communication [63], and needs to
be expanded to also include communication between healthcare workers.
Improving communication skills has been shown to reduce diagnostic
errors due to communication-related system errors [61,64]. New tools to
improve communication like Situation, Background, Assessment, and
Recommendation (SBAR) technique (a framework for effective communication
among members of the health care team) [65], and techniques for improved
hand-off [66] can be included into training curricula of nursing staff
and residents and serve as an opportunity to address diagnostic errors
by educational intervention. Training of emergency medicine residents in
SBAR [67] has been used to improve communication during hand-offs. Team
training, is another educational intervention that may improve
communication between the healthcare team and reduce system-related
diagnostic errors [36,37]. Most of these educational interventions could
gainfully be incorporated during the internship and residency training.
Education for Reducing No-fault Errors
As primarily these are due to the shortcomings of
current medical knowledge and technological abilities of the diagnostic
armamentarium, there is likely to be gradual reduction in them with
advancement of medical knowledge and technological progress, which will
allow recognition of newer diseases and also permit diagnosis at early
stages of the disease.
However, there is certain inevitability about these
errors and they are unlikely to be eliminated, e.g., atypical
presentations, early non-specific manifestations, emerging diseases (new
diseases, new pathogens, or side-effects of newer drugs etc.) may
continue to lead to diagnostic errors, and medical science will need to
continuously evolve to catch up with the utopia of nil diagnostic
errors. Patient-specific factors include both non-compliance (due to a
variety of reasons [67,68]), and the patients’ appreciation and
description of their symptoms (which may vary depending on their
socio-cultural or educational background, and their belief-system). Such
training in communication and coordination of care would go a long way
in reducing this group of errors.
Educational intervention can be aimed at improving
cognition directly by training better history-takers (able to tease out
hidden aspects of history from the patient), and better communicators
(thereby ensuring compliance with investigations, treatment and
follow-up). The students need to be taught, in addition, to practice
worst-case scenario medicine (always consider the worst possible
diagnosis when faced with a particular symptom), and ask what
(consider what symptoms or findings cannot be explained by the
diagnosis) and why (thinking about the reason why some problem
occurred, especially for an acute exacerbation of a chronic disorder)
questions [7]. Addressing the culture of non-performance and tolerance
of errors also needs to be addressed by educational interventions;
departmental and Institutional mortality reviews and difficult-case
meetings should aim to address these.
Conclusions
Improving the diagnostic process is not only
possible, but also represents a moral, professional, and public health
imperative [4]. Although, the individual physicians may be more
comfortable in discussing the ‘system-faults’ rather than cognitive
errors, which are apparently more personal, it is the cognitive aspect
that is more amenable to educational interventions. Addressing
diagnostic errors systematically will require a comprehensive approach;
developing formal curricula to educate trainees about misdiagnoses is
one such [68,69]. We hope that individual institutions and teachers will
take the onerous responsibility of carrying out teaching-learning
activities for reduction of diagnostic error, till such time
professional or regulatory bodies develop such curricula.
References
1. Athreya BH. Handbook of Clinical Skills. World
Scientific, Singapore; 2010.
2. Medical Council of India. Vision 2015. MCI, Delhi;
2011.p.15-16. Available from: http://www.mciindia.org/tools/
announcement/MCI_booklet.pdf. Accessed January 25, 2016.
3. Graber M. Diagnostic errors in medicine: a case of
neglect. Jt Comm J Qual Patient Saf. 2005;31:106-13.
4. Committee on Diagnostic Error in Health Care,
Institute of Medicine. Improving Diagnosis in Health Care. September,
2015. Available from:
https://iom.nationalacademies.org/~/media/Files/Report%20Files/2015/Improving-Diagnosis
/Diagnostic Error_ReportBrief.pdf. Accessed December 12, 2015.
5. Newman-Toker DE, Pronovost PJ. Diagnostic
errors–the next frontier for patient safety. JAMA. 2009; 301:1060-2.
6. Modi JN, Anshu, Gupta P, Singh T. Teaching and
assessing clinical reasoning skills. Indian Pediatr. 2015; 52:787-94
7. Trowbridge RL. Twelve tips for teaching avoidance
of diagnostic errors. Med Teach. 2008;30:496-500.
8. Croskerry P. The importance of cognitive errors in
diagnosis and strategies to minimize them. Acad Med. 2003;78:775-80.
9. Bordage G. Why did I miss the diagnosis? Some
cognitive explanations and educational implications. Acad Med.
1999;74(10 suppl):S138-S143.
10. McLeod W, Eidus R, Stewart E. Clinical decision
support: Using technology to identify Patients’ Unmet Needs. Fam Pract
Manag. 2012;19:22-8. Available from: http://www.aafp.org/
fpm/2012/0300/p22.html. Accessed January 27, 2016.
11. Apps: Bloice MD, Simonic KM, Holzinger A.
Casebook: a virtual patient iPad application for teaching
decision-making through the use of electronic health records. BMC Med
Inform Decis Mak. 2014;14:66.
12. Murphy DR, Wu L, Thomas EJ, Forjuoh SN, Meyer AN,
Singh H. Electronic trigger-based intervention to reduce delays in
diagnostic evaluation for cancer: a cluster randomized controlled trial.
J Clin Oncol. 2015;33:3560-7.
13. Singh H, Giardina TD, Forjuoh SN, Reis MD, Kosmach
S, Khan MM, et al. Electronic health record-based surveillance of
diagnostic errors in primary care. BMJ Qual Saf. 2012;21:93-100.
14. Olsen DE, Sticha D. Interactive simulation
training: computer simulated standardized patients for medical
diagnosis. Stud Health Technol Inform. 2006;119:413-5.
15. Berner ES, Graber ML. Overconfidence as a cause
of diagnostic error in medicine. Am J Med. 2008;121 (5 Suppl):S2-23.
16. Singh H, Giardina TD, Meyer AN, Forjuoh SN, Reis
MD, Thomas EJ, et al. Types and origins of diagnostic errors in
primary care settings. JAMA Intern Med. 2013;173:418-25.
17. Singh H, Thomas EJ, Wilson L, Kelly PA, Pietz K,
Elkeeb D, et al. Errors of diagnosis in pediatric practice: a
multi-site survey. Pediatrics. 2010;126:70-9.
18. Ordi J, Ismail MR, Carrilho C, Romagosa C, Osman
N, Machungo F, et al. Clinico-pathological discrepancies in the
diagnosis of causes of maternal death in sub-saharan Africa:
retrospective analysis. PLoS Med. 2009;6:e1000036.
19. Herman AA, Stein DJ, Seedat S, Heeringa SG,
Moomal H, Williams DR. The South African Stress and Health (SASH) study:
12-month and lifetime prevalence of common mental disorders. South
African Med J. 2009;99:339-44.
20. Cheng XJ1, Cheng Q, Xu LZ, Zhao HQ, Zhao Z, Wang
W, et al. Evaluation of multiple sclerosis diagnostic criteria in
Suzhou, China—risk of under-diagnosis in a low prevalence area. Acta
Neurol Scand. 2010;121:24-9.
21. Kotovicz F, Mauad T, Saldiva PHN. Clinico-Pathological
Discrepancies in a General University Hospital in São Paulo,
Brazil. Clinics (Sao Paulo, Brazil). 2008;63:581-88. Available from:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2664713/. Accessed
January 26, 2016.
22. Prashanth LK, Taly AB, Sinha S, Arunodaya GR,
Swamy HS. Wilson’s disease: diagnostic errors and clinical impli-cations.
J Neurol Neurosurg Psychiatry. 2004;75:907-09.
23. Parikh PM, Nair V, Malhotra H, Ranade AA,
Bhattacharyya GS. Medical Errors – Aiming to improve the Art and Science
of Healthcare. Medicine Update 2008.p.873-81. Available from:
http://www.apiindia.org/pdf/medicine_ update_2008/chapter_115.pdf.
Accessed January 26, 2016.
24. Leape LL, Brennan TA, Laird N, Lawthers AG,
Localio AR, Barnes BA, et al. The nature of adverse events in
hospitalized patients. Results of the Harvard Medical Practice Study II.
N Engl J Med. 1991;324:377-84.
25. Bartlett EE. Physicians’ cognitive errors and
their liability consequences. J Healthcare Risk Manage. 1998;18:62-9.
26. Tai DYH, El-Bilbeisi H, Tewari S, Mascha EJ,
Wiedermann HP, Arroliga AC. A study of consecutive autopsies in a
medical ICU: a comparison of clinical cause of death and autopsy
diagnosis. Chest. 2001; 119:530-6.
27. Croskerry P. The theory and practice of clinical
decision making. Can J Anesth. 2005;52:R1-R8.
28. Norman G. Dual processing and diagnostic errors.
Adv Health Sci Educ Theory Pract. 2009;14:37-9.
29. Elstein AS. Heuristics and biases: selected
errors in clinical reasoning. Acad Med. 1999;74:791-4.
30. Graber M, Gordon R, Franklin N. Reducing
diagnostic errors in medicine: what’s the goal? Acad Med.
2002;77:981-92.
31. Wardrop D. Ockham’s Razor: sharpen or re-sheathe?
J R Soc Med. 2008: 101: 50-51.
32. Voytovich AE, Rippey RM, Suffredini A. Premature
closure in diagnostic reasoning. J Med Educ. 1985;60: 302-7.
33. Herrle SR, Corbett EC, Fagan MJ, Moore CG,
Elnicki M. Bayes’ theorem and the physical examination: probability
assessment and diagnostic decision-making. Acad Med. 2011;86:618-27.
34. Graber ML, Franklin N, Gordon R. Diagnostic error
in internal medicine. Arch Intern Med. 2005;165:1493-9.
35. Kostopoulou O, Delaney BC, Munro CW. Diagnostic
difficulty and error in primary care - a systematic review. Fam Pract.
2008;25:400-13.
36. Kassirer JP, Kopelman RI. Cognitive errors in
diagnosis: instantiation, classiûcation, and consequences. Am J Med.
1989;86:433-41.
37. Graber ML. Educational strategies to reduce
diagnostic error: can you teach this stuff? Adv Health Sci Educ.
2009;14:63-9
38. Graber ML, Kissam S, Payne VL, Meyer AN, Sorensen
A, Lenfestey N, et al. Cognitive interventions to reduce
diagnostic error: a narrative review. BMJ Qual Saf. 2012;21:e535-57.
39. Wears RL. What makes diagnosis hard? Adv Health
Sci Educ Theory Pract. 2009;14 (Suppl 1):19-25
40. Croskerry, P. Clinical cognition and diagnostic
error: applications of a dual process model of reasoning. Adv Health Sci
Educ. 2009; 14 (Suppl 1):27-35.
41. Diemers AD, van de Wiel MW, Scherpbier AJ, Baarveld
F, Dolmans DH. Diagnostic reasoning and underlying knowledge of students
with preclinical patient contacts in PBL. Med Educ. 2015;49:1229-38.
42. Croskerry, P. Cognitive forcing strategies in
clinical decision making. Ann Emergency Med. 2003; 41:110–20.
43. Bowen JL. Educational strategies to promote
clinical diagnostic reasoning. NEJM. 2006; 355:2217-25.
44. Hauer KE, Teherani A, Kerr KM, O’Sullivan
PS, Irby DM. Student performance problems in medical school clinical
skills assessments. Acad Med. 2007;82(10 Suppl):S69-72.
45. Murray DJ, Freeman BD, Boulet JR, Woodhouse
J, Fehr JJ, Klingensmith ME. Decision making in trauma settings:
simulation to improve diagnostic skills. Simul Healthc. 2015;10:139-45.
46. Croskerry P1, Petrie DA, Reilly JB, Tait G.
Deciding about fast and slow decisions. Acad Med. 2014;89:197-200
47. Monteiro SD, Sherbino J, Patel A, Mazzetti
I, Norman GR, Howey E. Reflecting on diagnostic errors: taking a second
look is not enough. J Gen Intern Med. 2015; 30:1270-4
48. Schiff GD. Minimizing diagnostic error: The
importance of follow-up and feedback. Am J Med. 2008;121:S38-S42.
49. Moulton CE, Regehr GE, Mylopoulos M, MacRae HM.
Slowing down when you should: A new model of expert judgment. Acad Med.
2007;82:S109-S116.
50. Garfield FB, Garfield JM. Clinical judgement and
clinical practice guidelines. Int J Technol Assess Health Care.
2000;16:1050-60.
51. Klassen TP, Ropp LJ, Sutcliffe T, Blouin R,
Dulberg C, Raman S, et al. A randomized controlled trial of
radiograph ordering for extremity trauma in a pediatric emergency
department. Ann Emerg Med. 1993;22:1524-9.
52. El-Kareh R, Hasan O, Schiff GD. Use of health
information technology to reduce diagnostic errors. BMJ Qual Saf.
2013;22:ii40-51.
53. General Medical Council. Tomorrow’s Doctors:
Outcomes for Graduates, 2015, p. 7. Available from:
http://www.gmc-uk.org/Outcomes_for_graduates_Jul_15.pdf_61408029. pdf.
Accessed May 11, 2016.
54. Chaudhry B, Wang J, Wu S, Maglione M, Mojica W,
Roth E, et al. Impact of health information technology on
quality, efficiency, and costs of medical care. Ann Intern Med.
2006;144:742-52.
55. Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of
computer–based clinical decision support systems on physician
performance and patient outcomes: a systematic review. JAMA.
1998;283:2816-21.
56. Kripalani S, Williams MV, Rask K. Reducing errors
in the interpretation of plain radiographs and computed tomography
scans. In: Shojania KG, Duncan BW, McDonald KM, Wachter RM (eds).
Making Health Care Safer. A Critical Analysis of Patient Safety
Practices. Rockville, MD: Agency for Healthcare Research and Quality,
2001.
57. Kronz JD, Westra WH, Epstein JI. Mandatory second
opinion surgical pathology at a large referral hospital. Cancer.
1999;86:2426-35.
58. Payne VL, Singh H, Meyer AN, Levy L, Harrison
D, Graber ML. Patient-initiated second opinions: systematic review of
characteristics and impact on diagnosis, treatment, and satisfaction.
Mayo Clin Proc. 2014;89:687-96.
59. Riesenberg LA, Leitzsch J, Massucci JL, Jaeger J,
Rosenfeld JC, Patow C, et al. Residents’ and attending
physicians’ handoffs: a systematic review of the literature. Acad Med
2009;84:1775-87.
60. DeRienzo CM, Frush K, Barfield ME, Gopwani PR,
Griffith BC, Jiang X, et al. Handoffs in the era of duty hours
reform: a focused review and strategy to address changes in the
Accreditation Council for Graduate Medical Education Common Program
requirements. Acad Med. 2012;87: 403-10.
61. Starmer AJ, Spector ND, Srivastava R, West DC,
Rosenbluth G, Allen AD, et al. for the I-PASS Study Group.
Changes in medical errors after implementation of a handoff
program. NEJM. 2014; 371:1803-12D.
62. Modi JN, Anshu, Chhatwal J, Gupta P, Singh T.
Teaching and assessing communication skills during undergraduate
training. Indian Pediatr. 2016:53:.
63. Medical Council of India. Sensitization Program
on Attitude and Communication Module (AT-COM). MCI decisions on MET.
2015. Available from:
http://www.mciindia.org/fdp/MCI_decisions_on_MET.pdf. Accessed
October 3, 2015.
64. Singh H, Naik AD, Rao R, Petersen LA. Reducing
diagnostic errors through effective communication: harnessing the power
of information technology. J Gen Intern Med. 23:489-94.
65. WHO Collaborating Centre for Patient Safety
Solutions. Communication during patient handovers. Patient Safety
Solutions 2007; 1: 3. Available from:
http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution3.pdf.
Accessed January 21, 2016.
66. Kemp CD, Bath JM, Berger J, Bergsman A, Ellson T,
Emery K, et al. The top 10 list for a safe and effective
sign-out. Arch Surg. 2008;143:1008-10.
67. Tews MC, Liu JM, Treat R.
Situation-Background-Assessment-Recommendation (SBAR) and emergency
medicine residents’ learning of case presentation skills. J Grad Med
Educ. 2012;4:370-73.
68. Jin J, Sklar GE, Min Sen Oh V, Chuen Li S.
Factors affecting therapeutic compliance: A review from the patient’s
perspective. Therapeut Clin Risk Manag. 2008;4:269-286.
69. Khullar D, Jha AK, Jena AB. Reducing diagnostic
errors – why now? NEJM. 2015;373:2491-3. Available from:
http://www.nejm.org/doi/full/10.1056/NEJMp1508044. Accessed December
15, 2015.
|
|
|
 |
|

