|
|
|
Indian Pediatr 2016;53: 67 -69 |
 |
Auxiliary Liver Transplantation for Acute
Liver Failure
|
|
Naresh P Shanmugam, *Tawfiq
Al-Lawati, Chaya Kelgeri and #Mohamed
Rela
From Department of Paediatric Gastroenterology, Hepatology and
Transplantation, and #Institute of Liver Diseases and
Transplantation, Global Health City, Chennai, India; and *Department of
Paediatric Gastroenterology, Hepatology and Nutrition, The Royal
Hospital, Sultanate of Oman.
Correspondence to: Dr Naresh P Shanmugam, Department of Paediatric
Gastroenterology, Hepatology and Transplantation, Global Health City,
439, Cheran Nagar, Perumbakkam,
Chennai 600 100, Tamilnadu, India.
Email: [email protected]
Received: May 13, 2015;
Initial review: July 08, 2015;
Accepted: September 30, 2015.
|
|
Background: Auxiliary partial
orthotopic liver transplantation is a technique where part of diseased
native liver is removed and replaced with healthy donor liver so that,
the left behind native liver could later regenerate. Case
characteristics: 2½-year-old girl with acute liver failure due to
Hepatitis A. She underwent a successful auxiliary partial orthotopic
liver transplantation. Outcome: Successful native liver
regeneration and immunosuppression withdrawal after two and half years
of surgery. Message: In selective cases of acute liver failure,
auxiliary partial orthotopic liver transplantation could provide a
chance for native liver regeneration and immunosuppression-free life.
Keywords: Cirrhosis, Hepatitis A, Liver
regeneration.
|
|
Acute liver failure (ALF) in children is a rare
but potentially fatal disorder, which could lead to multiorgan failure
and death within days to weeks of onset. Liver transplantation (LT) is
an accepted form of treatment that improves the survival in ALF
patients, who fulfill the criteria for liver transplantation. In
children with virus-induced ALF, International normalized ratio (INR) >4
or factor V levels <25% of normal should be considered for liver
transplantation [1]. The standard orthotopic liver transplant (OLT)
technique involves removal of the entire failing liver from the
recipient and replacing it with a healthy donor liver. Auxiliary partial
orthotopic liver transplant (APOLT) is a specialized technique where
either the right or the left lobe of diseased native liver is removed
and replaced with healthy donor liver. Given the tremendous regenerative
capacity, there is a potential for the failed native liver to regenerate
over a period of time.
Case Report
A 2½-year-old child from the Arabic Gulf with
Hepatitis A induced ALF developed hepatic encephalopathy and was
intubated and ventilated. As the child fulfilled liver transplantation
criteria, she was stabilized and airlifted to our center for Living
Related LT. At the time of surgery, she had already been ventilated for
12 days and was critically ill with INR of 6, lactate of 5.5 mmol/Land
bilirubin of 17.8 mg/dL. The native left liver lobe of the child was
resected and replaced with left lateral segment from the donor, who was
her paternal uncle. She was started on standard immunosuppression with
tacrolimus and steroids. Her lactate and INR normalized in two days and
bilirubin normalized in seven days. Postoperative period was complicated
by hypotension requiring inotropic support, sepsis, narcotic withdrawal,
and prolonged ventilation necessitating tracheostomy. She was
off-ventilator two weeks after APOLT, and was discharged home four weeks
after surgery.
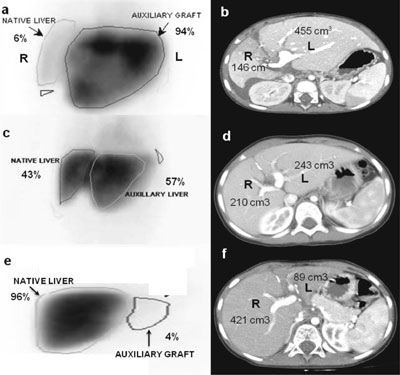
Di-isopropyl iminodiacetic acid (DISIDA) scan at four
weeks after APOLT showed that transplanted left lobe of the liver
contributed to 96% of the total liver function (Fig. 1a)
and computer tomography (CT) volumetry showed diseased native liver
(right lobe) volume of 146 cm 3
and graft (left lobe) of 455 cm3
(Fig. 1b). Histopathology of the native
liver showed near total absence of hepatocytes, consistent with
Hepatitis A induced ALF. The child was followed up with serial DISIDA
scan and CT volumetry on a 6-monthly basis. At 2 years post APOLT,
DISIDA scan and CT showed that native liver has regenerated and
contributed to 43% of liver function (Fig. 1c) and around
50% of total liver volume (Fig. 1d) respectively, with
histopathology showing restoration of normal architecture of the native
liver. Based on these positive indicators, immuno-suppression was
gradually weaned off over the following six months, allowing low-grade
rejection of the graft, which progressively lead to fibrosis and graft
atrophy. CT and DISIDA scan done immediately after stopping
immunosuppression confirmed that native right lobe contributed to 96% of
total function (Fig. 1e) and 83% (421 cm3)
of total liver volume (Fig. 1f) respectively. This implied
that the native liver has regenerated in terms of volume and
functionality. The child is completely off all immunosuppressive
medications and has normal liver function tests.
 |
|
Fig.1 Serial DISIDA scan at 1, 24 and
30 months after APOLT showing gradual recovery of native liver
(right lobe) function (a,c,e); and corresponding CT images of
gradual volumetric regeneration of native liver (right lobe) (b,d,f).
L: left lobe (transplanted liver), R; right lobe (native liver).
|
Discussion
Though first case of successful liver regeneration
after APOLT for ALF was reported in 1991, only few centers perform this
procedure as it is technically challenging [2]. One center reported 100%
mortality with APOLT in ALF, with none surviving long enough to stop
immuno-suppression, while another center reported 85% survival in
children with ALF who underwent APOLT [3,4]. The reason behind failure
of native liver regeneration is difficult to predict based on
quantitative hepatocyte loss. Quaglia, et al. [5] showed that new
hepatocytes could be derived from both mature cholangiocytes and
putative progenitor cells located within the bile ductular epithelium.
The patients in whom the native liver failed to regenerate are not at
disadvantage as they just need to continue immunosuppressive medications
similar to patients having standard OLT.
Candidate selection for APOLT in ALF is crucial and
ideally suits patients with a one-time insult leading on to ALF such as
drug poisoning, acute viral hepatitis and that of indeterminate
etiology. Cirrhotic liver disease is a contraindication for APOLT as
there will be problems in portal flow to native liver due to portal
hypertension and also there is a possibility of malignant transformation
in the left over cirrhotic native liver. Though autoimmune liver disease
and Wilson diseases could present as ALF, these livers would be
cirrhotic at the time of presentation. Performing APOLT in a cirrhotic
liver defies the whole purpose of this technique, as these patients
would need the donor organ support lifelong and weaning of
immunosuppression might not be possible. In ALF, there is massive liver
cell necrosis due to the disease process. In standard OLT whole liver is
removed, but in APOLT the retained necrotic liver can release several
cytokines causing hemodynamic and metabolic instability during
post-operative period. This complication has to be anticipated and
managed appropriately by the intensivist.
Once the volume and function of native liver (based
on CT and DISIDA scan) is approximately equal to the transplanted
liver, immunosuppression should be gradually weaned over several months,
so that the transplanted liver graft atrophies slowly. Abrupt
immunosuppression withdrawal might lead on to hepatic artery thrombosis
and graft infarction, which might require surgical removal of the graft.
In selective cases of ALF, APOLT preserves native
liver and provides a chance for native liver regeneration and
immunosuppression-free life. The fact that children have a longer life
expectancy, offering a medication- free life makes APOLT an attractive
option. Appropriate case selection, surgical expertise and
post-operative manage-ment are the key elements in successful outcome of
APOLT in ALF.
Contributors: NPS: drafted the article;
TAL: review of literature; CK: helped with image artwork; MR: review of
manuscript. All authors participated in patient management.
Funding: None; Competing interests: None
stated.
References
1. Shanmugam NP, Dhawan A. Selection criteria for
liver transplantation in paediatric acute liver failure: The saga
continues. Pediatr Transplant. 2011;15:5-6.
2. Gubernatis G, Pichlmayr R, Kemnitz J, Gratz K.
Auxiliary partial orthotopic liver transplantation (APOLT) for fulminant
hepatic failure: First successful case report. World J Surg.
1991;15:660-5.
3. Kasahara M, Takada Y, Egawa H, Fujimoto Y, Ogura
Y, Ogawa K, et al. Auxiliary partial orthotopic living donor
liver transplantation: Kyoto University experience. Am J
Transplant. 2005;5:558-65.
4. Faraj W, Dar F, Bartlett A, Melendez HV, Marangoni
G, Mukherji D, et al. Auxiliary liver transplantation for
acute liver failure in children. Ann Surg. 2010;251:351-6.
5. Quaglia A, Portmann BC, Knisely AS, Srinivasan P,
Muiesan P, Wendon J, et al. Auxiliary transplantation for
acute liver failure: Histopathological study of native liver
regeneration. Liver Transpl. 2008;14:1437-48.
|
|
|
 |
|

