Neonates with respiratory distress need continuous distending pressure
to achieve adequate functional residual capacity. Any change in the
severity of pulmonary disease is reflected as a change in need for the
distending pressure or fraction of inspired oxygen (FiO2)
or both. A tool incorporating these parameters would potentially help in
objectively assessing the severity of the pulmonary disease.
Current assessment of pulmonary disease is with blood
gas, chest X-ray and Oxygenation index (OI). OI cannot be
calculated for babies on Continuous Positive Airway Pressure (CPAP) and
Non-invasive Positive Pressure Ventilation (NIPPV), and has resource
implications. A non-invasive assessment tool would allow clinicians to
use it more frequently. Non-invasive tools such as Oxygen saturation
index and Respiratory severity score [1,2] cannot be used in babies on
CPAP or non-invasive ventilation. Saturation (SPO2),
Oxygen (FiO2) and distending
Pressure (PEEP) index, or SOP index, attempts to objectively
score respiratory disease with parameters available in babies on CPAP or
non-invasive ventilation.
This was a single-centre prospective observational
study undertaken in a Canadian tertiary care Neonatal intensive care
unit (NICU). Our primary objective was to evaluate if the SOP index
correlates with Oxygenation index in neonates. Secondary objective was
to find the cut-off values of SOP index for mild, moderate and severe
pulmonary disease. Both term and preterm neonates on conventional
mechanical ventilation were enrolled. Babies with severe congenital
anomalies and congenital heart disease and SPO2
above 98% were excluded from the study. Consent waiver for the study was
provided by the McMaster Research Ethics Board.
SOP index was calculated by the formula, PEEP
X FiO2/ SpO2.
PEEP, FiO2 and SpO2
on the monitor was recorded prior to arterial blood gas sampling. SPO2
was recorded when there was a good waveform.
Thirty-six patients were recruited and total of 72
data sets were obtained. The first obtained value for each patient was
separately tabulated. Pearson product moment correlation between SOP
index and Oxygenation index was calculated. All the data sets combined
were analyzed using linear mixed model effect with random intercept for
predictive equation. We calculated sensitivity and specificity of SOP
index corresponding to oxygenation index of <5, 5 -15 and >15 using ROC
curve. We did not stratify the patients according to gestational age.
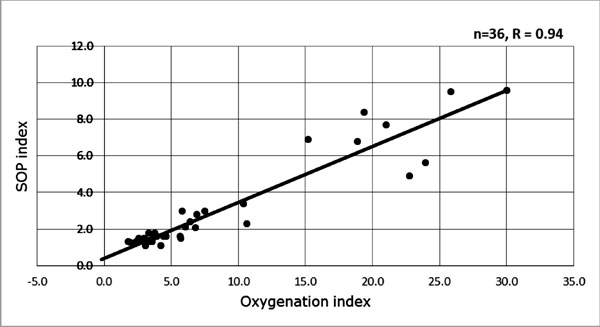
Pearson product moment correlation (r) of 0.94 (P=0.001)
was noted between SOP index and Oxygenation index (Fig.1).
The calculated predictive equation for SOP index was 0.28 X OI
+ 0.87. SOP indices corresponding to OI <5 (mild), 5-15 (moderate)
and >15 (severe lung disease) are <2, 2 to 3.7 and >3.7, respectively.
With 89% sensitivity and 94% specificity. The sensitivity and
specificity of SOP index for mild, moderate and severe pulmonary disease
was 89.5% and 94.1%, 89.5% and 94.1%, and 100% and 94.6%, respectively.
 |
|
Fig. 1 Linear correlation between SOP
index and Oxygenation index.
|
SOPI is calculated with PEEP. This makes it possible
to use SOP index in babies who are on CPAP or NIPPV, where only PEEP is
reliable. Lung injury assessment with PaO2:FiO2
[3] and Oxygenation index, which has been successfully used in neonates
[4], can only be measured by an arterial puncture or indwelling
catheter.
SOP index has very good correlation with oxygen
index. SOPI of <2, 2 to 3.7 and greater than 3.7 indicates pulmonary
disease with high sensitivity and specificity. SOP index has potential
to be used for assessment of the severity of acute pulmonary disease in
babies on CPAP and NIPPV.
Acknowledgement: Respiratory therapists at
McMaster University NICU for their help in collecting the required data.
Contributors: SMD: conceived and designed the
study. He analysed the data and prepared the manuscript; and will act as
the guarantor. AAC: study design and collection of the data. He has
revised and approved the manuscript. PM: helped in designing the study
and data analysis. He has revised the manuscript and approved for
submission.
Funding: None; Competing interests; None
stated.
References
1. Thomas NJ, Shaffer ML, Douglas F, Willson, Shih
MC, Curley MAQ. Defining acute lung disease in children with the
oxygenation saturation index. Pediatr Crit Care Med. 2010;11:12-7.
2. Iyer NP, Mhanna JM. Non-invasively derived
respiratory severity score and oxygenation index in ventilated newborn
infants. Pediatr Pulmonol. 2013;48:364-9.
3. Bernard GR, Artigas A, Brigham KL, Carlet J, Halke
K, Hudson L, et al. The American-European Consensus Conference on
ARDS definitions, mechanisms, relevant outcomes, and clinical trial
coordination and the consensus committee. Am J Respir Crit Care Med.
1994;149:818-24.
4. Konduri G, Solimano A, Sokot GM, Singer J,
Ehrenkranz RA, Singhal N, et al. A randomized trial of early
versus standard inhaled nitric oxide therapy in term and near-term
newborn infants with hypoxic respiratory failure. Pediatrics.
2004;113:559-64.

