|
|
|
Indian Pediatr 2015;52: 69 -70 |
 |
Teratoma at the Esophagogastric Junction in a
Neonate
|
|
Rui Dong, Chun Shen and Shan Zheng
From Department of Pediatric Surgery, Children’s
Hospital of Fudan University, and Key Laboratory of Neonatal Disease,
Shanghai, China.
Correspondence to: Dr Shan Zheng, Department of
Pediatric Surgery, Children’s Hospital of Fudan University, and Key
Laboratory of Neonatal Disease, Ministry of Health, 399 Wan Yuan Road,
Shanghai 201102, China.
Email: [email protected]
Received: July 07, 2014;
Initial review: August 04, 2014;
Accepted; October 08, 2014
|
|
Background: Teratoma at the esophagogastric junction is extremely
rare. Case Report: A 26-day-old male neonate who presented with
vomiting and melena. Observation: Investigations revealed a mass
at the esophagogastric junction, which was excised and confirmed to be a
teratoma. Outcome: A fistula at the lower end of the esophagus
and an esophageal hiatal hernia were observed as complications.
Message: A careful surgical approach is warranted for a teratoma in
esophagogastric junction, to avoid postoperative complications.
Keywords: Neonate, Teratoma, Vomiting.
|
|
A
teratoma containing hair, teeth, bone and, very
rarely, more complex organs or processes may occur at any site [1], but
its location at the esophagogastric junction is extremely rare. We
report a newborn with immature teratoma of the esophagogastric junction.
Case Report
A 26-day-old male neonate presented with intermittent
vomiting of approximately two weeks duration, and malena for one day.
The general physical and systemic examinations were unremarkable. An
initial contrast-enhanced computed tomography (CECT) scan showed upper
esophageal dilation, unclear lower esophagus, and a large tumor mass
between the esophagus and gastric fundus. The upper gastrointestinal
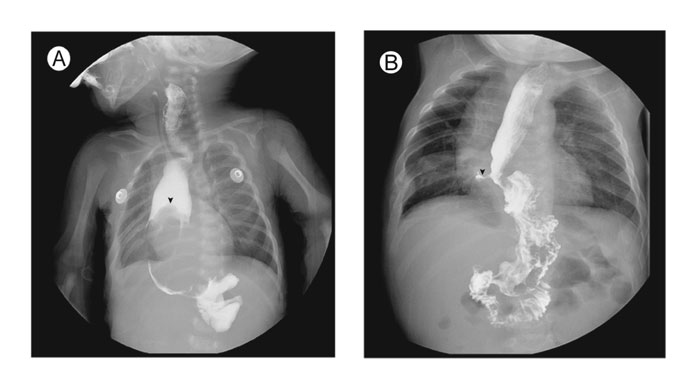
barium study (Fig. 1a) revealed a large tumor mass
in the lower esophagus involving the cardia and gastric fundus. The
laboratory tests were within normal limits, including liver function
tests, lactate dehydrogenase, ferritin, carcino-embryonic antigen, and
neuron-specific enolase. Alpha fetoprotein was elevated with 5284 ng/mL.
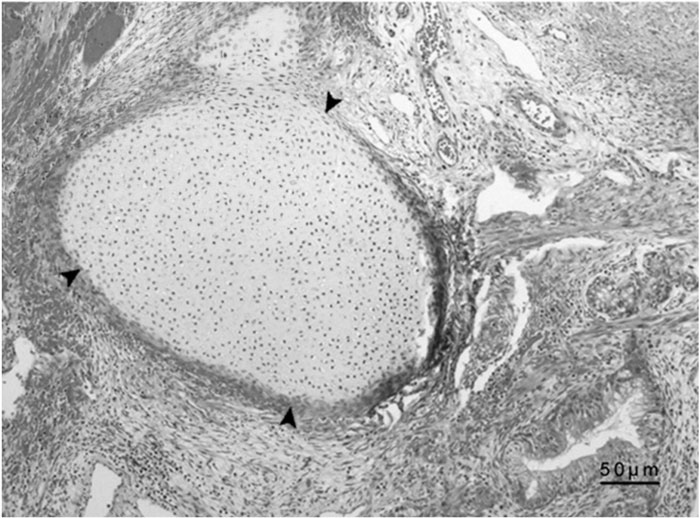
A biopsy was taken from the margins of the tumor mass, and
immuno-histochemistry revealed an immature teratoma (Fig. 2).The
tumor mass was surgically excised. The post-operative period was
uneventful. The infant was discharged home after 2 weeks. He was
breastfeeding well and there was no vomiting.
 |
|
Fig. 1 Upper gastrointestinal barium
study showing (a) tumor mass in the lower esophagus involving
the cardia and gastric fundus before surgery (arrows ); (b) a
fistula (arrows) located at the lower end of the esophagus,
fundus being pulled up to the diaphragm, and an esophageal
hiatal hernia at 1-month follow up.
|
 |
|
Fig. 2 Immunohistochemistry reveals an
immature teratoma (arrow shows the bone content). (See
website for color image).
|
At the three-month follow-up, alpha fetoprotein
levels had reduced to normal, 2.83 ng/mL. At follow-ups at 6 months and
1 year, the boy was in a better condition, accepting normal food and his
growth and development were normal. An upper gastrointestinal barium
study at 1 month after surgery revealed a fistula located at the lower
end of the esophagus, fundus pulled up to the diaphragm, and an
esophageal hiatal hernia (Fig. 1b). The infant is
being followed closely and the decision to repair the fistula is
pending.
Discussion
Teratomas most often occur in a para-axial location,
in the midline from the brain to the sacral area, or in the gonads.
Teratoma at the esophagus and stomach is extremely rare in children,
accounting for less than 1% of all teratomas. To date, only one such
case has been reported in the English literature [2]. Bernat, et al.
[3] reported seven cases of benign esophageal tumors treated in a
hospital from 1972 to 1990, only one of them was finally diagnosed as
mature teratoma. He reported complete cure in all patients after surgery
[3].
Gastric teratoma is believed to arise from the
pluripotent cells of the gastric visceral wall [4]. The majority is
benign and immature. The site of gastric teratoma is variable, most
commonly arising from the greater curvature and posterior wall. The
clinical features of esophagogastric junction teratoma in the neonate of
the present case appeared at three weeks of life, with vomiting and
melena, and without abdominal distension, constipation, or respiratory
distress.
The melena could be due to mucosal bleeding at the
tumor site. The CECT scan suggested the possibility of a leiomyosarcoma
or neuroblastoma. The final diagnosis of teratoma can only be confirmed
by histopathological examination of tissue. The alpha fetoprotein levels
reflect the treatment response after excision, and may be of
significance when chemotherapy is recommended in immature teratomas.
Complete excision of the teratoma carries a good prognosis.
Few post-operative complications were noted in the
present case. An inadequately dissected fundus may pull it into the
chest, which could increase the anastomotic tension between the
esophagus and stomach, and lead to the postoperative fistula. On the
other hand, the hiatal hernia could have been induced by an inadequately
repaired esophageal hiatus. In addition, difficulties during surgery,
especially exposing the mass, looking for a surgical entry point, and
complete removal of the tumor may have added to the risk of
postoperative complications.
While resecting such masses, full dissociation of the
fundus and pulling it into the chest may reduce esophageal and gastric
anastomotic tension and thereby avoid the occurrence of postoperative
fistula.
References
1. Peterson CM1, Buckley C, Holley S, Menias CO.
Teratomas: A multimodality review. Curr Probl Diagn Radiol.
2012;41:210-9.
2. Giacomoni MA, Zaffaroni G. Teratoma of the gastro-esophageal
junction in an infant. Arch Ital Chir. 1968;94:781-7.
3. Bernat M1, Strutyńska-Karpińska M, Lewandowski A,
Blaszczuk J, Grabowski K, Czapla L. Benign esophageal tumors. Wiad Lek.
1993;46:24-7.
4. Logani KB, Tayal A, Bhan S, Choudhary M, Uma G. Gastric teratoma
in infants-a report of two cases. Indian J Cancer. 1983;30:34-7.
|
|
|
 |
|

