|
|
|
Indian Pediatr 2012;49:
25-28 |
 |
Maternal Risk Factors Associated with Term Low
Birth Weight Neonates: A Matched-Pair Case Control Study |
|
Sachin S Mumbare,
#Girish
Maindarkar, ‡Rajesh Darade,
$Surekha Yenge, *Madhav Kumar
Tolani and †Kiran Patole
From the Departments of Community Medicine, *Pediatrics,
and †Obstetrics & Gynecology, NDMVPS Medical College, Nashik;
$Civil Hospital, Nashik; and Departments of #Pediatrics, and ‡Obstetrics;
Government Medical College, Latur; Maharashtra, India.
Correspondence to: Dr Sachin S Mumbare, Associate
Professor, Department of Community Medicine, NDMVPS Medical College,
Adgaon, Nashik 422 003. [email protected]
Received: September 04, 2010; Initial review: October 23,
2010;Accepted: January 11, 2011 .
Published online: 2011, May 30. PII:
S09747559INPE1000229-1
|
Objective: To study maternal risk factors associated with full term
low birth weight (LBW) neonates.
Design: Matched pair case control study.
Setting: Multicenter study including 2 medical
colleges and 1 civil hospital, between July 2009 to December 2009.
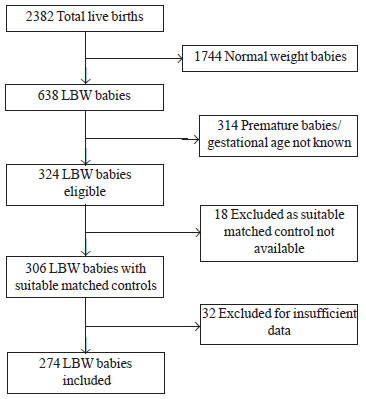
Patients: Of 2382 neonates screened, 274 full term
LBW babies (of 638) and 274 pair matched controls (of 1744) were included
in the study. 364 LBW babies were excluded because of premature
delivery/gestational age not known (314), unavailability of suitable
matched controls (18), and insufficient data (32).
Methods: Maternal factors including birth spacing,
height, pre-delivery weight and pregnancy weight gain, age, parity,
educational and economic status, type of family, antenatal care (ANC),
maternal exposure to tobacco, hypertension and anemia were studied.
Results: Birth spacing <36 months, maternal height
£145
cm, pre-delivery weight £55
kg, pregnancy weight gain ≤6
kg, exposure to tobacco, inadequate antenatal care, maternal hypertension,
low socio-economic status, maternal anemia and less maternal education
were associated with delivery of a low birth weight infants. Conditional
logistic regression analysis showed that significant risk factors
associated with low birth weight were inadequate ANC (OR-4.98, 95% CI-2.64
to 9.39), maternal weight before delivery ≤55 kg
(OR-4.81, 95% CI-2.53 to 9.15) and height ≤145 cm
(OR-4.13, 95% CI-2.04 to 8.37).
Conclusion: Maternal malnutrition, inadequate
antenatal care and poor weight gain during pregnancy are significant
predictors for delivery of a low birth weight neonate.
Key words: India, Full term, LBW, Maternal risk factors.
|
|
Low birth weight (LBW) (neonate weighing <2500 g) is
a multifactorial phenomenon [1]. Many maternal and fetal factors are found
significantly to be associated with the low birth weight [2]. Many of
these factors are interrelated and they can confound the results in
addition to modifying the independent estimates of relative risk
associated with a risk factor. We conducted this matched pair case control
study to identify the maternal risk factors associated with full term low
birth babies.
Methods
The present multicenter study was carried out in
Government Medical College, Latur; NDMVPS Medical College, Nashik, and
Civil Hospital, Nashik. Required minimum sample size was calculated as 173
using the formula provided by Bhalwar [3] and considering following
values: a
= 0.05, b
= 0.2, (proportion of controls likely to have exposure 20% and odds ratio
= 2.
Singleton live births, delivered between July 2009 to
December 2009, irrespective of the mode of delivery, were screened for
inclusion in the study. Birthweight of every child was measured in gram
using pretested and precalibrated weighing machines. World Health
Organization definition of low birth weight (LBW) babies i.e. birth
weight less than 2500 g [4] was used to label a child as LBW. Inclusion
criteria were low birth weight child, singleton pregnancy, exact duration
of amenorrhea was known (to calculate the gestational age at the time of
delivery), full term delivery ( ³38
weeks of gestation), mother willing to participate in the study, and
suitable matched control was available. If any of the above criteria was
not fulfilled then the child was not included as a case in the study. A
matched control, having birth weight more than 2500 g, was selected for
every case. Birth date within 1 month, sex, tehsil and religion
were matched for selection of the control in each and every pair. If two
or more suitable matched controls were available for a case, only one was
selected randomly.
Data about the maternal exposure to different risk
factors in mothers of all cases and controls was recorded using a
pretested questionnaire. Information included sociodemographic profile of
the mother and her family; obstetric history of the mother, especially
information about previous births/abortions; antenatal services obtained
by the mother, including antenatal clinic (ANC) registration, antenatal
visits and checkups, tetanus toxoid injections, consumption of iron and
folic acid tablets, information relating to heavy work done, rest timings
etc exposure to possible risk factors like hypertension, exposure to any
form of tobacco, any other systemic disease; results of blood
investigations (especially hemoglobin percentage plus any other result)
done within 15 days prior to the delivery; weight of the mother before
delivery in kg rounded to two decimals; and height in cm. This information
was cross checked with the available records such as ANC cards and case
sheets to minimize the recall bias.
Adequate antenatal care was considered when the
pregnant woman was registered at any time, had at least three antenatal
checkups, was adequately vaccinated against tetanus, had consumed at least
100 tablets of iron and folic acid, was not involved in hard work, and had
taken adequate rest during pregnancy (minimum 2 hours sleep during day and
8 hours sleep during night). Low socioeconomic status was considered if
the family of mother belonged to a below poverty line family. Weight gain
was calculated by subtracting weight of the mother at 12 weeks or before
from weight of the mother at term, considering negligible weight gain up
to 12 weeks of gestation [5]. Maternal exposure to tobacco meant use of
any tobacco product such as tobacco or gutkha chewing, cigarette or
bidi smoking, or any other form of smoking.
All the pairs were divided into four subclasses
depending on the exposure of case and/or control to a risk factor, as
follows: (a) number of pairs in which both, case and control, were
exposed to the maternal risk factor; (b) number of pairs in which
only case and not control was exposed to the maternal risk factor; (c)
number of pairs in which only control and not case was exposed to the
maternal risk factor and (d), number of pairs in which neither case
nor control was exposed to the risk factor. Matched odds ratio with 95%
confidence interval was calculated using the method suggested by Liddell
[6]. McNemar chi square test, z test and t test were used to
compare the qualitative and quantitative exposures in cases and controls,
where applicable. Conditional logistic regression analysis was applied to
find out the effect of the potential confounders. StatsDirect software was
used for analysis of data.
Results
Total babies screened for birthweight were 2382. Number
of LBW babies born during the study period was 638 (26.78 %). Out of them
274 LBW babies were included in the study (Fig.1).
Table I shows the distribution of various factors among cases and
controls.
 |
|
Fig. 1 Flow chart showing process of case
selection. |
TABLE I Maternal Exposure to Various Risk Factors in Low Birthweight Babies and Controls
|
Maternal risk factor |
LBW |
Normal birthweight |
|
Height (cm) |
147.3 (4.79) |
152.3 (4.88) |
|
Spacing (mo) |
26.42 (4.56) |
31.25 (5.09) |
|
Pre-delivery weight |
61.6 (4.93) |
56.7 (4.51) |
|
#Weight gain (kg) |
5.84 (1.42) |
7.27 (1.06) |
|
Age (years) |
23.19 (3.37) |
23.72 (3.53) |
|
Parity 1 |
168 (61.3%) |
146 (53.3%) |
|
Anemia |
143 (52.2%) |
71 (25.9%) |
|
Hypertension |
64 (23.4%) |
25 (9.1%) |
|
Inadequate ANC |
171 (62.4%) |
87 (31.7%) |
|
Nuclear family |
143 (52.2%) |
147 (53.7%) |
|
Below poverty line |
130 (47.4%) |
65 (23.7%) |
|
Tobacco exposure |
73 (26.6%) |
25 (9.1%) |
|
†Maternal education |
202 (73.7%) |
166 (60.6%) |
|
‡Paternal education |
103 (37.6%) |
102 (37.2%) |
*Birth spacing; 106 LBW babies and 128 normal weight babies; #108 LBW babies and 192 normal weight babies;
†Less than Higher secondary; ‡Higher secondary or more; LBW: Low birth weight
|
Conditional logistic regression analysis was done to
eliminate the effects of potential confounders and to identify the
independent effect of various risk factors. It showed that the most
important risk factors associated with low birth weight babies were
inadequate ANC (OR -4.98, 95% CI -2.64 to 9.39), maternal weight before
delivery ≤55 kg
(OR-4.82, 95 % CI - 2.54 to 9.15) and height ≤145 cm (OR- 4.13, 95%
CI- 2.04 to 8.37).
TABLE II Conditional Logistic Regression Analysis
|
Factor |
Odds ratio 95% CI |
P value |
|
Inadequate ANC# |
4.98(2.64-9.39) |
<0.00 |
|
Weight ≤55 kg* |
4.81(2.53-9.15) |
<0.00 |
|
Height ≤145 cm |
4.13(2.04-8.37) |
<0.00 |
|
Tobacco exposure |
4.10(1.85-9.06) |
<0.00 |
|
Anaemia |
3.36(1.91-5.88) |
<0.00 |
|
Hypertension |
3.32(1.55-7.10) |
0.002 |
|
Low SES |
3.27(1.81-5.91) |
<0.001 |
|
Parity 1 |
1.55(0.85-2.80) |
0.148 |
|
Maternal education |
1.17(0.67-2.04) |
0.580 |
|
Paternal Education |
1.10(0.60-2.00) |
0.755 |
|
Nuclear family |
0.91(0.55-1.50) |
0.711 |
|
Age of the mother |
0.53(0.24-1.19) |
0.123 |
|
*Pre-pregnancy; SES: Socioeconomic status; #Antenatal
care. |
Discussion
This multicenter matched pair case control study was
done to identify the maternal risk factors associated with full term low
birth weight babies. Proportion of low birth weight babies was 26.8%,
which is more than the prevalence of LBW (21.5%) observed in National
Family Health Survey (NFHS-3) [7]. This was expected as the study was
carried out in tertiary care hospitals where many of the pregnant women
are referred from the peripheral hospitals because of high risk pregnancy.
This study has shown that full term low birth weight
was significantly associated with inadequate antental care, pre-delivery
weight ≤55 kg,
height ≤145 cm,
weight gain ≤6
kg, spacing <36 months, maternal exposure to any form of tobacco
hypertension, low socio-economic status, and anemia.
Kramer’s meta-analysis [8], and other studies conducted
in developing countries [9-14] have identified maternal weight (<45kg),
maternal height (<145cm) as potential risk factors for LBW babies. Low
socioeconomic status and low educational status leads to low health
consciousness, lower nutritional status and low antenatal attendance,
leading to the increased risk of LBW babies [15]. The finding of
significant association of low socioeconomic status and LBW babies shown
by this study is consistent with previous studies [7,13,16,17]. Present
study has not identified maternal age and parity as significant risk
factors for LBW babies. This finding is consistent with the findings of
Mavalankar [10], Fikree [11] in Pakistan and Acharya, et al. [14].
Many studies [15,17] have; however, shown that young maternal age and
parity are significant risk factors of LBW. The finding of maternal
stature as a significant risk factor for LBW is consistent with the
literature [1,18] Risk of
delivering LBW was 4.1 times high in women exposed to any tobacco product
as compared to those who were not exposed to tobacco. The finding is
confirmatory to the findings of Deshmukh, et al. [1], Gupta, et
al. [19] and Ward [20]. Thus not only smoking, which is widely
accepted as an independent risk factor for LBW, tobacco chewing is also a
risk for the same.
Spacing and weight gain could not be included in the
conditional logistic regression analysis because there were only 53 and 82
pairs in which data were available. Imputation method to deal with these
missing values was not used, as spacing is not applicable at all for
primigravida. There were 192 (70.07%) pairs in which data related to
weight gain in case and/or control was missing. The confounding effect of
maternal education was probably due to its association with low
socioeconomic status.
Thus findings of this study emphasizes the need for
improving the quality and utilization of antenatal care, nutritional
education to improve the weight gain during pregnancy, spacing, avoidance
of tobacco, and prevention and proper management of risk factors like
anemia and hypertension.
Acknowledgment: Dr Mrunal Patil, Dean, NDMVP
Medical College, Nashik for allowing us to carry out the study and
providing the required manpower. Dr Balaji Almale and Dr Sandip Gundare
for helping in data collection, feeding and analysis.
Contributors: SSM conceived and designed the study.
He also analyzed and interpreted the data; GM and RD coordinated data
collection in Government Medical College, Nashik and were involved in
manuscript writing; SY coordinated the data collection in Civil Hospital
Nashik and MT and KP in NDMVPS Medical College, Nashik. They were involved
in critical evaluation and necessary modifications in the contents of the
manuscript. All the authors approved the final manuscript.
Funding: None; Competing interests: None
stated.
|
What is Already Known?
• Predictors of full term LBW babies have been
previously described.
What This Study Adds.
• Inadequate antenatal care, maternal weight
£55
kg at the time of delivery, height ≤145
cm, weight gain
£6
kg or spacing <36 month are important predictors of full term LBW
baby.
|
References
1. Deshmukh JS, Motghare DD, Zodpey SP, Wadhva SK. Low
birth weight and associated maternal factors in an urban area. Indian
Pediatr. 1998;35:33-6.
2. Singh G, Chouhan R, Sidhu K. Maternal factors for
low birth weight babies. Medical Journal Armed Forces India.2009; 65:10-12
3. Bhalwar R. Case control studies: Planning, design,
conduct and analysis. Journal of Community Health. 2007; 9:31-9.
4. International Classification of Disease, Ninth
revision, Volume 1. Geneva: World Health Organization; 1977.
5. Humphreys RC. An analysis of the maternal and fetal
weight factors in normal pregnancy. J Obstet Gynecol Br Empire.
1954;61:764-71.
6. Liddell FD. Simplified exact analysis of
case-referent studies; matched pairs; dichotomous exposure. J Epidemiol
Community Health. 1983;37:82-4.
7. International Institute of Population Sciences,
National Family Health Survey, India. 2005-06 (NFHS-3, Vol. 1) 2007:225.
8. Kramer MS. Determinants of low birth weight:
Methodological assessment and metaanalysis. Bull WHO. 1987;65:663-737.
9. Ferraz EM, Gray RH, Cunha TM. Determinants of
preterm delivery and intrauterine growth retardation in north-east Brazil.
Int J Epidomiol. 1990;19:101-8.
10. Mavalankar DV, Gray RH, Trivedi CR. Risk factors
for preterm and term low birth weight in Ahmedabad, India. Int J Epidemiol.
1992;21:263-72.
11. Fikree FF, Berendes HW. Risk factors for term
intrauterine growth retardation: Community based study in Karachi. Bull
WHO. 1994;72:581-7.
12. Pelletier D, Arimond M, Johnson FC, Liang E, Low J,
Mvula P, et al. Maternal anthropometry predictors of IUGR and
prematurity in Malawi Maternal and Child Nutrition study (OMS Supplement).
Bull WHO. 1995;73:81.
13. Jafari F, Eftekhar H, Pourreza A, Mousavi J.
Socio-economic and medical determinants of low birth weight in Iran: 20
years after establishment of a primary healthcare network. Public Health.
2010;124:153-8.
14. Acharya D, Nagraj K, Nair NS, Bhat HV. Maternal
determinants of intrauterine growth retardation: a case control study in
Udupi District, Karnataka. Indian J Community Med. 2004;29:181-3.
15. Mann LI, Tejani NA, Weiss RR. Antenatal diagnosis
and management of small for gestational age fetus. Am J Obstet Gynecol.
1974;120:995-1004.
16. Sharma MK, Kumar D, Huria A, Gupta P. Maternal risk
factors of low birth weight in Chandigarh India. Internet J Health.
2009: 9. Available from http://www.ispub.com/journal/the_internet_journal_of_health/volume_9_
number_1_12/article/maternal-risk-factors-of-low-birth-weight-in-chandigarh-india.html.
Accessed 10 December, 2010.
17. Viengsakhone L, Yoshida Y, Harun-Or-Rashid M,
Sakamoto J. Factors affecting low birth weight at four central hospitals
in vientiane, Lao PDR. Nagoya J Med Sci. 2010;72:51-8.
18. Ghosh S. Hooja V, Mittal SK, Verma RK, Ghosh S,
Hooja V, et al. Biosocial determinants of birth weight.. Indian
Pediatr. 1977;14:107-13.
19. Gupta PC, Sreevidya S. Smokeless tobacco use, birth
weight, and gestational age: population based, prospective cohort study of
1217 women in Mumbai, India. BMJ. 2004;328:1538.
20. Ward C, Lewis S, Coleman T. Prevalence of maternal
smoking and environmental tobacco smoke exposure during pregnancy and
impact on birth weight: retrospective study using Millennium Cohort. BMC
Public Health. 2007;7:81.
|
|
|
 |
|

